Guidelines in a nutshell: The 2021 GOLD report
Practice Nurse 2020;50(10):23-25
Practice Nurse 2020;50(10):23-25
The key change in the latest update to the GOLD report on COPD is on the management of this condition during the COVID-19 pandemic
Not surprisingly given the circumstances over the last 12 months, the annual update of the Global Initiative for Chronic Obstructive Lung Disease (GOLD) report has only comparatively minor changes to its main recommendations. However, it does include a comprehensive guide to the management of COPD during the coronavirus pandemic.
The last major update, the fourth since the GOLD programme was set up in 1998, was published in 2017 and was based on a wide-reaching reassessment of previous recommendations for diagnosis, assessment and treatment. There have been updates each year since then. You can catch up with a summary of the 2020 report in the ‘Guidelines’ section at practicenurse.co.uk.
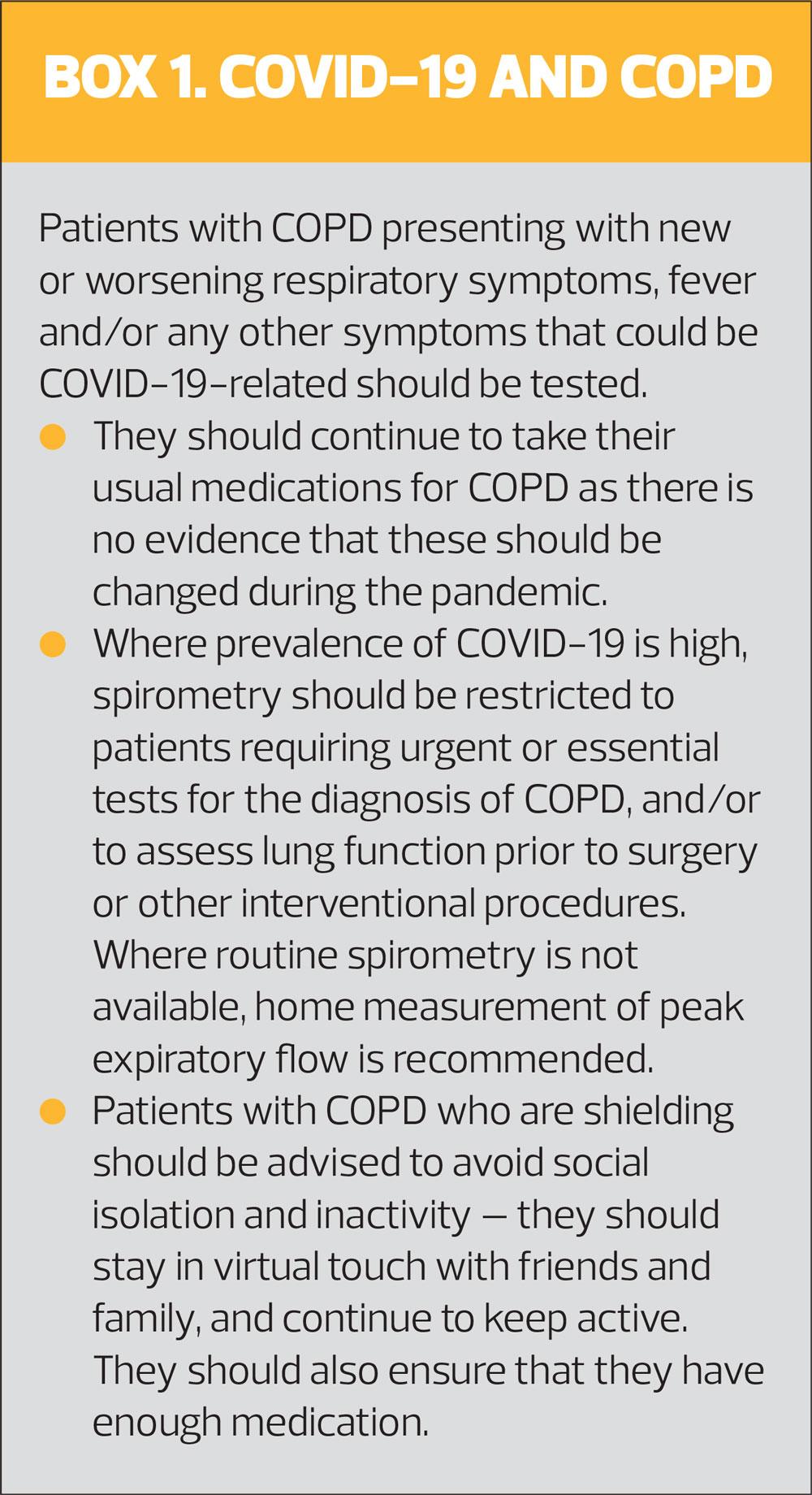
IMPACT OF COVID-19
Not only has COVID-19 has made the diagnosis and routine management of COPD more difficult, but also COPD makes the diagnosis of COVID-19 more complicated.
The increased difficulty in routine management of COPD is largely as a result of the reduced availability of face-to-face consultations, spirometry and pulmonary rehabilitation programmes.
While COPD does not appear to increase the risk of COVID-19 infection (although this may be the result of protective strategies such as shielding), it does seem to increase the risk of severe disease. The pandemic has also led to fewer hospital admissions for people with COPD. The reasons for this are unclear, but patients with symptoms of an exacerbation should be evaluated as usual, and admitted if necessary.
The presence of COPD may make it less easy to diagnose COVID-19, especially when COVID symptoms are mild. A high index of suspicion should be maintained in patients presenting with an exacerbation, especially if they have fever, impaired taste or smell, or gastrointestinal symptoms.
Maintenance pharmacotherapy
The use of systemic or inhaled corticosteroids (ICS) has been controversial during the pandemic. ICS have an overall protective effect against exacerbations in COPD, but are associated with an increased risk of pneumonia – leading to fears that ICS could leave people at increased susceptibility to COVID-19 infection. However, there are no conclusive data to support changes to COPD treatment.
Non-pharmacological treatment
Many pulmonary rehabilitation programmes have been put on hold to reduce the risk of transmission, so it is important to encourage patients with COPD to keep active at home, and where possible offer web- or app-based rehabilitation that they can do at home.
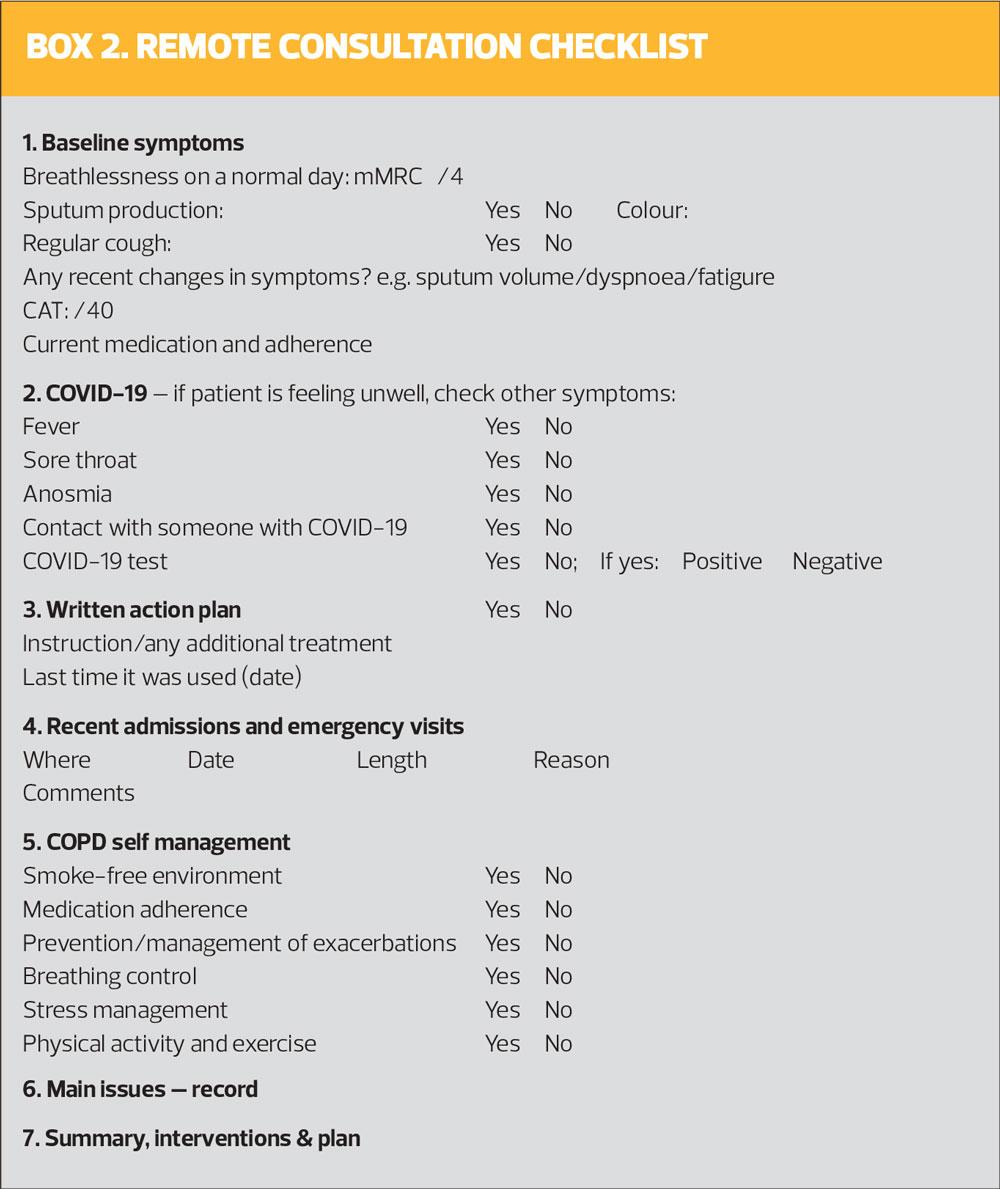
Review of COPD patients
We have all seen a dramatic growth in the use of remote consultations, over the phone or using video solutions. GOLD supports their use as ‘superb tools’ – both as a way of minimising the risk of coronavirus transmission, and of increasing the efficiency and capacity of healthcare systems into the future.
GOLD has produced a tool to support remote consultations, with a checklist for follow-up (Box 2), and available at https://goldcopd.org/wp-content/uploads/2020/11/GOLD-REPORT-2021-v1.0-16Nov20_WMV.pdf.
Follow up of COPD patients who have had COVID-19
- Patients who developed mild COVID-19 should be followed up as usual for patients with COPD
- Patients who have had moderate COVID-19 (hospitalisation and pneumonia but no respiratory failure) should be monitored more frequently and accurately than usual. Consider need for oxygen therapy
- If chest X-ray abnormalities have not resolved at hospital discharge, a chest X-ray or CT scan should be considered at 6 months to 1 year
- COPD survivors of severe COVID-19 should be considered at high risk of developing chronic critical illness linked not only to the acute infectious episode but also to their underlying conditions before they became severely ill
Of course the 2021 report covers all aspects of COPD, and not just the impact of the pandemic on management. Some of the other main changes are summarised below.
SMOKING CESSATION
The 2021 report reminds us of the importance of smoking cessation, which remains – probably – the single most effective intervention in the management of COPD. Smoking cessation has the greatest capacity to influence the natural history of COPD. Where time and resources are available, long term quit success rates of up to 25% can be achieved.
Nicotine replacement therapy (NRT) remains the cornerstone of pharmacotherapy to aid smokers to quit. However, it is not suitable for everyone, and among the contraindications for NRT is recent myocardial infarction. The contraindication to NRT after acute coronary syndrome is less clear cut, but GOLD advises that treatment should be delayed for at least 2 weeks after a cardiovascular event.
A more recent aid to smoking cessation has been electronic cigarettes (e-cigarettes, vaping). GOLD points out that effectiveness is controversial, with one study suggesting that e-cigarettes were only modestly effective in helping smokers to quit, and no more effective than nicotine patches.2 In contrast, a more recent randomised controlled trial, based in UK Stop Smoking services found that the 1-year quit rate in the e-cigarette arm was almost twice that in the NRT arm.3 It also confirmed that – because e-cigarettes incur lower NHS costs than NRT and generate a higher quit rate – e-cigarette use is more cost effective than NRT.3
One barrier to the use of vaping products as an aid to smoking cessation was the emergence last year (2019) of a spate of cases of lung disease related to e-cigarettes. GOLD says that as of February 2020, more than 2,800 cases of vaping product use-associated lung injury (EVALI) and 68 deaths, had been reported. Since the identification of vitamin E acetate, an additive in some e-cigarettes, as a primary cause of EVALI, there has been a decline in the number of new cases.
VACCINATIONS
The benefits of flu and pneumococcal vaccination in reducing exacerbations of COPD and subsequent hospitalisation are well established, but it is now recommended in the US that adults with COPD should also receive vaccination against pertussis in those who were not vaccinated as adolescents.
PHARMACOTHERAPY
Pharmacological therapy for COPD is used to reduce symptoms, reduce the frequency and severity of exacerbations, and improve exercise tolerance and health status. To date, GOLD, says, there is no conclusive clinical trial evidence that any existing medications for COPD modify the long-term decline in lung function.
As in previous versions of the guideline, treatment choice should be individualised as the relationship between severity of symptoms, airflow limitation and severity of exacerbations can differ between patients.
GOLD states:
- Inhaled bronchodilators are central to symptom management
- Regular and as-needed use of short-acting beta 2 agonists (SABA) or short-acting antimuscarinics (SAMA) improves FEV1 and symptoms
- Combinations of SABA and SAMA are superior to either medication along in improving FEV1 and symptoms
- Long-acting beta 2 agonists/ antimuscarinics (LABAs/LAMAs) significantly improve lung function, dyspnoea, health status, and reduce exacerbations
- LAMAs have a greater effect on reducing exacerbations than LABAs and decrease hospitalisations
- Combination treatment with a LABA and LAMA increases FEV1, reduces symptoms, and reduces exacerbations, compared with monotherapy
Most studies show that treatment with ICS alone does not modify the long-term decline of FEV1 nor mortality in patients with COPD, and some studies have reported a trend toward higher mortality in patients treated with ICS alone compared with those receiving ICS/SABA. There is some evidence that an ICS alone or in combination with a LABA may be associated with a slower decline in FEV1 compared with LABA alone.
GOLD concludes that in patients with moderate to very severe COPD and exacerbations, ICS combined with a LABA is more effective than either component alone in improving lung function, health status and reducing exacerbations.
Triple therapy (LABA+LAMA+ICS) can improve lung function, patient reported outcomes and reduce exacerbations compared with LAMA alone, LABA/LAMA and LABA/ICS.
Long-term use of oral corticosteroids has numerous side effects, with no evidence of benefits.
INHALER TECHNIQUE
The importance of education and training in inhaler device technique cannot be over-emphasised, GOLD reminds us. Most of the patients included in clinical trials to establish the efficacy of treatments are those who have mastered inhaler technique and have received proper education and follow up – and therefore may not be representative of normal clinical practice. On average, more than two thirds of patients make at least one error when using their inhaler device.
Factors that contribute to poor inhaler technique (in asthma patients, as well as those with COPD) include older age, use of multiple devices, and lack of education on inhaler technique. Education improves technique in some, but not all patients, especially when using the ‘teach-back’ approach – when patients are asked to demonstrate how their device has to be used. Patients who cannot master their inhaler may need a different device. Technique – and adherence – should be checked before the clinician concludes that current therapy is insufficient.
A new recommendation in this report is that pharmacist-led and lay health coaching can improve inhaler technique and adherence in patients with COPD.
COPD AND COMORBIDITIES
COPD often coexists with other conditions that may have a significant impact on prognosis. Some of these comorbidities may share common causes or risk factors, and some diseases may increase the risk or severity of the other.
Heart failure
Heart failure is a frequent comorbidity with COPD, with prevalence ranging from 20–70%. Unrecognised heart failure may be mistaken for or accompany acute COPD – 40% of COPD patients who are mechanically ventilated for respiratory failure have evidence of left ventricular dysfunction.
Treatment with beta blockers improves survival in heart failure and is recommended in patients with heart failure who also have COPD, but beta blockers should not be used to treat COPD unless they have cardiovascular indications.
- See Success in heart failure – new evidence, new approaches, page 18
Ischaemic heart disease
Ischaemic heart disease should be considered in all COPD patients, depending on their risk profile, and treatment initiated in accordance with current guidelines. Patients who have an exacerbation of COPD are at increased risk of a cardiovascular event, both during the exacerbation and for 90 days afterwards. Treatment should be according to guidelines, irrespective of the presence of COPD.
Atrial fibrillation (AF)
AF is common in patients with COPD, and associated with a lower FEV1. In COPD patients with severe, worsening dyspnoea, AF is frequently found, and it may either be a trigger for or result of an acute exacerbation. The presence of AF does not alter the treatment of COPD. Although bronchodilators may precipitate arrhythmia, the available evidence suggests that the safety profile of long-acting bronchodilators is acceptable. Use caution when prescribing short-acting beta2-agonists and theophylline, which may provoke AF and make control of ventricular response rate difficult.
Lung cancer
There is a confirmed association between COPD and lung cancer, and the two disease may have more in common than simply exposure to tobacco. Nonetheless, the best preventive measure for both conditions is smoking prevention and/or cessation.
Osteoporosis
Osteoporosis is a major comorbidity but is often under-diagnosed. It is often associated with emphysema and low body mass index. Low bone mineral density and fractures are common in COPD patients, even after adjustment for steroid use, smoking history, and exacerbations. Oral corticosteroids significantly increase the risk of osteoporosis, and repeated courses for COPD exacerbations should be avoided if possible.
Osteoporosis should be treated according to usual guidelines, and COPD should be treated as usual, despite the presence of osteoporosis.
Anxiety and depression
Anxiety and depression are common in patients with COPD, and both are associated with a poor prognosis. Conversely, COPD is also common in patients with other psychiatric illnesses, and is often under-diagnosed and treated.
There is no evidence that anxiety and depression should be treated differently in the presence of COPD, and likewise COPD should be treated as usual. Pulmonary rehabilitation may be particularly useful, as physical exercise is beneficial in both COPD and depression.
REFERENCES
1. GOLD. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease (2021 report); November 2020. https://goldcopd.org/wp-content/uploads/2020/11/GOLD-REPORT-2021-v1.0-16Nov20_WMV.pdf
2. Bullen C, Howe C, Laugeson M, et al. Electronic cigarettes for smoking cessation: a randomised controlled trial. Lancet 2013;382(9905):1629-37
3. Hajek P, Phillips-Waller A, Przulj D, et al. E-cigarettes compared with nicotine replacement therapy within the UK Stop Smoking Services: the TEC RCT. Health Technol Assess 2019;23(43):1-82
Related guidelines
View all Guidelines