GINA 2023: Guideline in a nutshell
Practice Nurse 2023;53(5): online only
Practice Nurse 2023;53(5): online only
The latest report from the Global Initiative for Asthma (GINA) strongly advises against prescribing short acting beta2 agonist (SABA) inhalers alone, even for patients with infrequent symptoms
GINA has reinforced its previous recommendation that an inhaled corticosteroid (ICS) should be given to all patients with asthma to reduce their risk of serious exacerbations.
Patients with asthma should also be prescribed a reliever – but GINA prefers the anti-inflammatory-reliever (AIR) approach to using a separate bronchodilator. GINA’s preferred treatment option uses ICS-formoterol, because it reduces the risk of severe exacerbations compared with other treatment options in which the reliever is SABA.
The rationale for this choice of reliever is:
- Patients with infrequent symptoms can still have severe or fatal exacerbations
- Adherence with daily ICS is poor in patients with infrequent symptoms, exposing them to the risks of SABA-only treatment
- There is no evidence for the safety or efficacy of SABA-only treatment. Regular use of SABA for 1-2 weeks leads to increased airway hyper-responsiveness and reduced bronchodilation
- It avoids former conflicting messages – patients were told to use SABA for symptom relief but then (despite the patient’s perception that this was effective) told to use ICS every day to cut down SABA use
- Starting treatment with SABA alone teaches the patient to regard SABA as their primary asthma treatment
SABA-only treatment of asthma is not recommended
For safety, GINA does not recommend treatment of asthma in adults or adolescents with SABA alone. All patients should receive ICS, either regularly, or in patients with ‘mild’ asthma, as as-needed ICS-formoterol to reduce their risk of serious exacerbations and asthma death.
SABA-only treatment is associated with increased risk of exacerbations, lower lung function, and of asthma-related death.
Regular use of SABA (i.e. three or more 200-dose inhalers dispensed in a year) is associated with an increased risk of severe exacerbations. Dispensing of 12 or more SABA inhalers, or possibly fewer than this, increases the risk of asthma-related death.
- ICS-containing treatment should be started as soon as possible after the diagnosis of asthma
- Even patients with mild asthma can have severe exacerbations
- Low-dose ICS markedly reduces asthma hospitalisations and death
- Low-dose ICS is very effective in preventing severe exacerbations, reducing symptoms, improving lung function, and preventing exercise-induced bronchoconstriction, even in patients with mild asthma
ANTI-INFLAMMATORY RELIEVER (AIR) THERAPY
GINA has endorsed the AIR approach to asthma management for adults and adolescents (See Anti-inflammatory reliever therapy for asthma: putting evidence into practice )
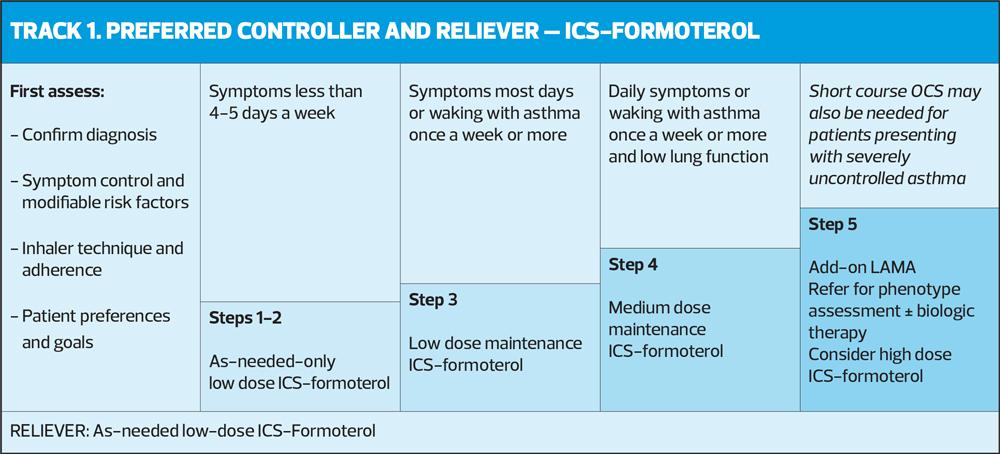
The preferred treatment pathway comprises five steps, as shown in the figure, Track 1.
- Steps 1 – 2. As-needed-only ICS-formoterol (AIR only)
- Steps 3 – 5. Maintenance and reliever therapy (MART with ICS-formoterol)
In all steps, the reliever should be as-needed low-dose ICS-formoterol.
Step 1 treatment (AIR only) with low-dose ICS-formoterol taken as needed for symptom relief is recommended for adults and adolescents as:
- Initial treatment for patients with infrequent symptoms (less than twice a month) and no exacerbation risk factors
- Step down treatment for patients whose asthma is well controlled on low-dose ICS-formoterol or low-dose ICS.
There is no evidence available for AIR use in children aged 6-11, so GINA suggests that they take ICS whenever SABA is taken, to avoid SABA-only treatment.
STARTING TREATMENT – AIR ONLY
Please refer to the figure for Track 1.
How to prescribe low-dose ICS-formoterol e.g. budesonide-formoterol 200/6 mcg
- Steps 1–2: 1 inhalation whenever needed for symptoms
- Step 3: 1 inhalation once or twice a day PLUS 1 inhalation whenever needed for symptoms
- Steps 4–4: 2 inhalations twice a day PLUS 1 inhalation whenever needed for symptoms
- As-needed doses of ICS-formoterol can also be taken before exercise or allergen exposure.
The usual dose of as-needed budesonide-formoterol is one inhalation of 200/6 mcg (4.5 mcg delivered dose) dry powder inhaler (DPI) taken whenever needed for symptom relief. For pMDIs containing 3 mcg formoterol (2.25 mcg delivered dose), take 2 inhalations each time.
Maximum dose
- Budesonide-formoterol: maximum 12 inhalations for adults (8 inhalations for children) in a single day (as-needed + maintenance)
- Beclometasone-formoterol: maximum total 8 inhalations per day
However, most patients needed far fewer doses than this.
N.B. ICS-LABA with a non-formoterol LABA cannot be used as needed.
After starting initial asthma treatment, review response after 2-3 months, and consider stepping down when asthma has been well-controlled for 3 months. However, ICS should not be completely stopped.
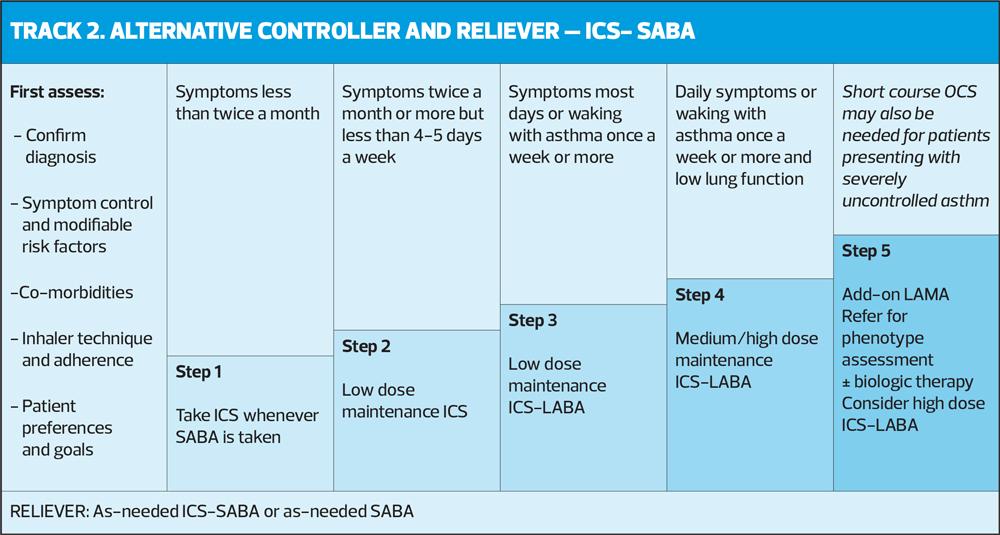
TRACK 2 – ALTERNATIVE CONTROLLER AND RELIEVER
An alternative, when Track 1 is not possible, or not preferred by a patient with stable asthma and no exacerbations on current therapy, is set out in the figure for Track 2
In Track 2, the reliever is as-needed SABA or ICS-SABA, but before prescribing a regimen with SABA as the reliever, consider whether (or not) the patient is likely to adhere to the ICS-containing inhaler, as otherwise they will be exposed to the risks of SABA-only treatment.
In Step 1, the patient takes a SABA and a low-dose ICS together for symptom relief when symptoms occur, in a combination inhaler, or with the ICS taken immediately after the SABA.
In Steps 2–5, the patient also takes maintenance ICS-containing medication every day. The option of using ICS-SABA as needed has been added as an option in Track 2 for Steps 3–5, with the most benefit of this option seen in Step 3, recommended for patients who experience asthma symptoms most days, or who wake with asthma once a week or more.
STEPPING UP TO MART
For adults and adolescents whose symptoms are not well controlled at Step 1 – 2, consider stepping up treatment to low-dose ICS-formoterol maintenance and reliever therapy (Step 3).
Whether or not the patient has a history of severe exacerbations, this combination has been shown to reduce the risk of exacerbations compared with other options (maintenance ICS-long-acting beta2 agonist [LABA], higher dose ICS, or conventional best practice with as-needed SABA), with a similar level of symptom control.
Before stepping up, check adherence, inhaler technique, environmental exposures and comorbidities.
At any step under Track 1 recommendations, when a patient has asthma symptoms, they should use low-dose ICS-formoterol. In Steps 3 – 5, patients also take combination ICS-formoterol as their daily maintenance treatment (MART).
NB. ICS-formoterol should not be used as the reliever by patients taking any other, non-formoterol ICS-LABA or ICS-LABA-LAMA (long acting antimuscarinic agonist).
INHALER CHOICE
Before prescribing, consider:
- What is the right medication for this patient?
- To control symptoms and reduce exacerbations
- Which inhaler can the patient use correctly?
- Incorrect technique leads to more exacerbations
- What are the environmental implications of these inhalers?
- Propellant (for pMDIs)
- Recycling potential
- Is the patient satisfied with the treatment and the inhaler?
- Consider the patient’s environmental priorities
- Avoid ‘green guilt’, which may affect adherence
- Check inhaler technique frequently
REVIEW, ASSESS, ADJUST
Patients should be seen between 1 and 3 months after starting treatment, and every 3 – 12 months after that. Patients should also be seen within 1 week of an exacerbation. Frequency of review depends on the individual patient’s
- Symptom control
- Risk factors
- Response to initial treatment
- Ability and willingness to self-manage, following a written, personalised asthma action plan (PAAP)
Regardless of whether Track 1 (preferred) or Track 2 (alternative) is followed, treatment can be stepped up or down, using the same reliever at each step, or it can be switched between tracks. But before stepping up, check for common issues such as incorrect inhaler technique, poor adherence, modifiable risk factors (e.g. smoking), and confirm that the symptoms are due to asthma or to a comorbid condition such as allergic rhinitis.
Consider stepping down once good asthma control has been achieved and maintained for 2–3 months, to find the lowest treatment level that controls symptoms and prevents exacerbations, and minimises side-effects. Do not completely stop ICS in adults or adolescents with asthma, unless to confirm the diagnosis of asthma, and make sure that you have arranged a follow-up appointment.
EXACERBATIONS
All patients with asthma should be provided with a written asthma action plan so they know how to recognise and respond to worsening asthma.
For patients on Track 1, advise the patient to take extra doses of low-dose ICS-formoterol whenever needed for symptom relief, and for Steps 3–5, to continue their usual maintenance dose(s). Patients who need to take more than 12 inhalations of budesonide-formoterol (or 8 inhalations of beclometasone-formoterol) a day, or whose symptoms are rapidly deteriorating, should seek medical attention without delay.
For patients on Track 2, advise them to take SABA when needed for symptom relief, and to increase their ICS-containing maintenance treatment, the dose of ICS can be increased x 4. For patients on maintenance ICS-LABA with non-formoterol LABA, step up to a higher dose formulation or add a separate ICS inhaler to achieve a large (4x) increase in ICS dose.
Instructions should also be provided on when to start a course of oral corticosteroids (OCS).
FOLLOW-UP AFTER EXACERBATION
An exacerbation can be seen as a failure of routine asthma care, and provides an opportunity to review management.
Review:
- The patient’s understanding of the cause of the exacerbation
- Modifiable risk factors e.g. smoking
- Choice of treatment track – Track 1 (AIR) reduces the risk of further severe exacerbations
- Understanding the purposes of medications
- Inhaler technique
- Adherence with ICS
- Written asthma action plan – revise if necessary.
AND FINALLY...
This ‘Guideline in a Nutshell’ summarises the key changes in the 2023 GINA report but we strongly urge you to read the full guidance – or at the very least the Pocket Guide for Asthma Management and Prevention – which contains a vast amount of information that any general practice nurse involved in asthma management should be aware of.
Global Initiative for Asthma. Pocket Guide for Asthma Management and Prevention; 2023. https://ginasthma.org/pocket-guide-for-asthma-management-and-prevention/
Related guidelines
View all Guidelines