Acute Otitis media: Diagnosis and management
INTRODUCTION
Acute otitis media is a common infection, especially in young children, and may be of viral or bacterial origin. Most cases will resolve spontaneously within 3-7 days, but there are circumstances when a prescription for antibiotics may be appropriate, and in some cases urgent referral or admission is warranted.
LEARNING OBJECTIVES
On completion of this module you will be better able to:
- Make an accurate diagnosis of acute otitis media (AOM)
- Prescribe antibiotic and analgesic treatment, if appropriate
- Know when to admit or refer to secondary care
- Manage people with persistent or recurrent AOM
- Give advice on measures to reduce the risk of recurrent episodes
PRACTICE NURSE FEATURED ARTICLE
Antibiotic resistance: what can we do? Dr Ed Warren
This resource is provided at an intermediate level. Read the article and answer the self-assessment questions, and reflect on what you have learned.
Complete the resource to obtain a certificate to include in your revalidation portfolio. You should record the time spent on this resource in your CPD log.
Contents
Acute Otitis media: Diagnosis and management
WHAT IS ACUTE OTITIS MEDIA?
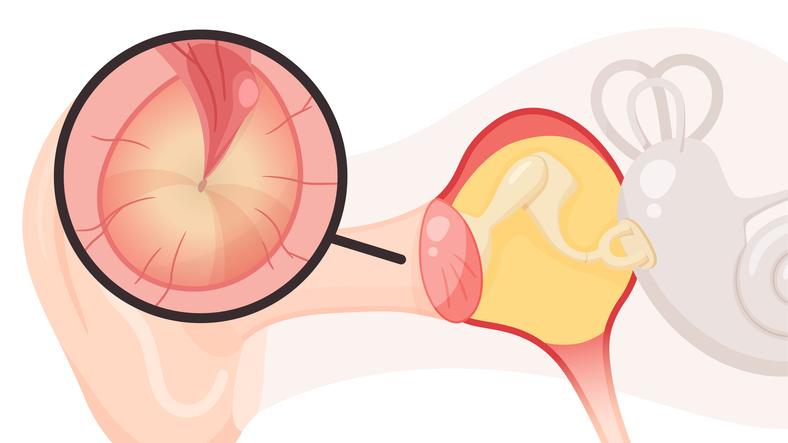
Acute otitis media (AOM) is defined as the presence of inflammation in the middle ear, associated with an effusion and accompanied by the rapid onset of symptoms and signs of an ear infection.
Otitis media with effusion (OME), is characterised by fluid in the middle ear, but is not associated with symptoms and signs of an acute ear infection.
Persistent AOM is defined as a patient returning for medical advice with the same episode of AOM, either because symptoms persist after initial management or because symptoms are worsening.
Recurrent AOM is defined as three or more separate AOM episodes in the preceding 6 months, or four or more episodes in the preceding 12 months with at least one episode in the past 6 months.
WHAT CAUSES ACUTE OTITIS MEDIA?
Acute otitis media can be caused by both viruses and bacteria, and commonly both are present at the same time.
The most common bacterial pathogens are Haemophilus influenzae, Streptococcus pneumoniae, Moraxella catarrhalis, and Streptococcus pyogenes.
Viral pathogens associated with AOM include respiratory syncytial virus (RSV), rhinovirus, adenovirus, influenza virus, and parainfluenza virus.
In recurrent AOM, the microbiology may be more complex, but the most common bacterial pathogens are the same as occasional episodes.
WHAT ARE THE RISK FACTORS?
Risk factors for developing acute otitis media include:
- Young age. Children are more likely to develop AOM because they acquire viral infections more often than adults, and have shorter and more horizontal eustachian tubes. Children from birth to 4 years of age are most likely to present with AOM. It most frequently affects children between 6 and 24 months old, with incidence peaking at 9–15 months of age.
- Male sex
- Smoking and/or passive smoking
- Frequent contact with other children such as daycare or nursery attendance or having siblings
- Formula feeding – breastfeeding has a protective effect
- Craniofacial abnormalities (such as cleft palate)
- Use of a dummy
- Prolonged bottle feeding in the supine position
- Family history of otitis media
- Lack of pneumococcal vaccination
- Gastro-oesophageal reflux
- Prematurity
- Recurrent upper respiratory tract infection
- Immunodeficiency.
PROGNOSIS AND COMPLICATIONS
Prognosis
Without antibiotic treatment, symptoms will improve within 24 hours in 60% of children with AOM, and most people will recover within 3 days.
Recurrent episodes of AOM are not uncommon. Recurrent AOM will resolve as the child gets older, often at 3–4 years of age.
Long term complications are very rare.
What are the complications?
Complications of acute otitis media include
- Persistent otitis media with effusion
- Recurrence of infection
- Hearing loss (usually temporary conductive loss)
- Tympanic membrane perforation
- Labyrinthitis
Rarely, the following can result from an episode of AOM: mastoiditis, meningitis, intracranial abscess, sinus thrombosis, and facial nerve paralysis.
HOW DO I MAKE A DIAGNOSIS OF ACUTE OTITIS MEDIA?
Diagnose acute otitis media if there is:
Acute onset of symptoms, including:
- In older children and adults — earache.
- In younger children — holding, tugging, or rubbing of the ear, or non-specific symptoms such as fever, crying, poor feeding, restlessness, behavioural changes, cough, or rhinorrhoea.
On otoscopic examination, the following signs may indicate AOM
- A distinctly red, yellow, or cloudy tympanic membrane.
- Moderate to severe bulging of the tympanic membrane, with loss of normal landmarks and an air-fluid level behind the tympanic membrane (which indicates a middle ear effusion).
- Perforation of the tympanic membrane and/or discharge in the external auditory canal.
Consider whether findings may be explained by other causes of middle ear inflammation or effusion.
Note that clinical features which are not suggestive of AOM include a tympanic membrane which is not bulging (with or without erythema or cloudiness), and an air-fluid level without a bulging tympanic membrane.
In children younger than 6 months of age (and particularly younger than 3 months of age), diagnosis can be difficult because:
- There may be coexisting systemic illness, such as bronchiolitis
- Symptoms are likely to be non-specific
The tympanic membrane may not be visible; it often lies in an oblique position and the ear canal is narrow making the tympanic membrane difficult to visualise
DIFFERENTIAL DIAGNOSIS – WHAT ELSE MIGHT IT BE?
Other causes of middle ear inflammation or effusion include:
- Otitis media with effusion (glue ear) – fluid in the middle ear without symptoms or signs of acute infection. On examination with an otoscope, an effusion and air fluid levels or bubbles are visible, with normal tympanic membrane landmarks. The most common presentation is conductive hearing loss.
- Chronic suppurative otitis media — persistent inflammation and perforation of the tympanic membrane with draining discharge for more than 2 weeks.
- Myringitis — erythema and injection of the tympanic membrane are visible on otoscopy but there are no other features of otitis media.
- Otalgia (earache) is a common problem, and can also be caused by otitis externa. Other causes of ear pain include eustachian tube dysfunction, temporomandibular joint dysfunction, mastoiditis, malignancy, and referred pain from a dental source.
HOW DO I MANAGE ACUTE OTITIS MEDIA?
Patients who have systemic infection or complications or are unwell
Admit for immediate specialist assessment:
- People with a severe systemic infection.
- People with suspected acute complications of AOM, such as meningitis, mastoiditis, intracranial abscess, sinus thrombosis, or facial nerve paralysis.
- Children younger than 3 months of age with a temperature of 38°C or more.
Consider admitting:
- Children younger than 3 months of age.
- Children 3–6 months of age with a temperature of 39°C or more.
For all people with AOM:
- Advise that the usual course of acute otitis media is about 3 days, but can be up to 1 week
- Advise regular doses of paracetamol or ibuprofen for pain, using a dosing schedule appropriate for the age and weight of a child. Explain that there is no evidence to support the use of decongestants or antihistamines for the management of symptoms.
For people who do not require admission to hospital but are systemically very unwell, have symptoms and signs of a more serious illness or condition, or have a high risk of complications:
- Offer an immediate antibiotic prescription
- Advise them to seek medical advice if symptoms worsen rapidly or significantly or they become systemically very unwell
Should I offer antibiotics for acute otitis media?
For people who may be more likely to benefit from antibiotics (those with otorrhoea, or those aged less than 2 years with bilateral infection) take account of evidence that acute complications such as mastoiditis are rare with or without antibiotics, and the possible adverse effects of antibiotics and consider:
- No antibiotic prescription — with advice about an antibiotic not being needed and seeking medical help if symptoms worsen rapidly or significantly, do not improve after 3 days, or the person becomes systemically very unwell, or
- A back-up antibiotic prescription — with advice about an antibiotic not being needed immediately; using the back-up prescription if symptoms do not start to improve within 3 days or worsen significantly or rapidly at any time; and seeking medical help if symptoms worsen rapidly or significantly, or the person becomes systemically very unwell, or
- An immediate antibiotic prescription — with advice to seek medical advice if symptoms worsen rapidly or significantly or the person becomes systemically very unwell.
For other people who may be less likely to benefit from antibiotics, take into account that antibiotics make little difference to symptoms or the development of common complications (which are rare with or without antibiotics) and possible adverse effects of antibiotics and consider:
- No antibiotic prescription — with advice about an antibiotic not being needed and seeking medical help if symptoms worsen rapidly or significantly, do not improve after 3 days, or the person becomes systemically very unwell, or
- A back-up antibiotic prescription — with advice about an antibiotic not being needed immediately; using the back-up prescription if symptoms do not start to improve within 3 days or worsen significantly or rapidly at any time; and seeking medical help if symptoms worsen rapidly or significantly, or the person becomes systemically very unwell.
If an antibiotic is required:
- Prescribe a 5–7 day course of amoxicillin
- For people who are allergic to, or intolerant of, penicillin, prescribe a 5–7 day course of clarithromycin or erythromycin (erythromycin is preferred in pregnant women).
HOW DO I MANAGE FOLLOW UP?
Reassess at any time if symptoms worsen rapidly or significantly, taking account of:
- Alternative diagnoses, such as otitis media with effusion (glue ear). Any symptoms or signs suggesting a more serious illness or condition.
- Previous antibiotic use which may lead to resistant organisms.
Routine follow up is not required in the absence of persistent symptoms of AOM.
If an episode of acute otitis media (AOM) fails to improve or worsens, reassess the person and exclude other causes of middle ear inflammation and pain.
- Consider referring adults with persistent acute otitis media to an ear, nose, and throat specialist, especially if symptoms last more than 6 weeks or are associated with persistent hearing loss.
Consider admission if patients develop complications or systemic symptoms.
If admission or referral is not necessary and the person has not taken an antibiotic:
- Prescribe a 5–7 day course of amoxicillin.
- For people who are allergic to, or intolerant of, penicillin, prescribe a 5–7 day course of clarithromycin or erythromycin (erythromycin is preferred in pregnant women).
If admission or referral is not necessary and symptoms are worsening despite taking a first–line antibiotic for at least 2–3 days, offer a second–line antibiotic:
- Prescribe a 5–7 day course of co-amoxiclav.
- For people who are allergic to, or intolerant of, penicillin, seek specialist advice from the local microbiology department.
If symptoms persist despite two courses of antibiotics, seek specialist advice from a local microbiologist or an Ear, Nose and Throat specialist if the diagnosis is uncertain.
Refer urgently (within 2 weeks) to an ear, nose, and throat (ENT) specialist if nasopharyngeal cancer (rare) is suspected, especially in the presence of any one of the following:
- Persistent symptoms and signs of otitis media with effusion in between episodes (for example, conductive hearing loss) due to obstruction of the eustachian tube orifice.
- Persistent cervical lymphadenopathy (usually in the upper levels of the neck).
- Epistaxis and nasal obstruction.
Consider referral to an ENT specialist for all people with recurrent AOM, especially if:
- The person has a craniofacial abnormality (Down's syndrome or a cleft palate).
- Recurrent episodes are unexplained, very distressing or associated with complications.
- An adult is affected.
If referral is not necessary, manage acute episodes in the same way as for initial presentation.
In people with grommets (tympanostomy or ventilation tubes) who present with acute discharge:
- Consider taking an ear swab for culture and sensitivity.
- Treat as for initial presentation or seek advice from an ENT specialist.
Provide advice on measures to prevent recurrence of AOM, including:
- In children – avoiding exposure to passive smoking, use of dummies, and supine feeding.
- In children – ensuring they have had a complete course of pneumococcal vaccinations as part of the routine childhood immunization schedule, and that any gastro-oesophageal reflux disease (GORD) is managed appropriately. In adults – avoiding smoking and/or passive smoking.
Do not start long-term prophylactic antibiotics in primary care.
ANTIBIOTIC REGIMENS
Amoxicillin
The treatment duration for AOM is 5–7 days.
In children, prescribe:
- 1 –11 months: 125 mg three times a day.
- 1–4 years: 250 mg three times a day.
- 5–17 years: 500 mg three times a day.
The dose should be reduced in children (weighing 40 kg or less) with renal impairment:
- If the glomerular filtration rate (GFR) is 10–30 ml/minute, prescribe 15 mg/kg twice daily (maximum 500 mg twice daily).
- If the GFR is less than 10 ml/minute, prescribe 15 mg/kg but only once daily (maximum 500 mg).
In adults, prescribe 500 mg three times a day.
The dose should be reduced in adults (and children weighing more than 40 kg) with renal impairment. If the GFR is less than 30 ml/minute an increase in the dosage interval and a reduction in the total daily dose is recommended:
- If GFR is 10–30 ml/minute, prescribe a maximum 500 mg twice a day.
- If GFR is less than 10 ml/minute, prescribe a maximum 500 mg once a day.
Clarithromycin
The treatment duration for AOM is 5–7 days.
In children, prescribe:
1 month to 11 years, with a body weight of:
- Under 8 kg: 7.5 mg/kg twice daily.
- 8–11 kg: 62.5 mg twice daily.
- 12–19 kg: 125 mg twice daily.
- 20–29 kg: 187.5 mg twice daily.
- 30–40 kg: 250 mg twice daily.
12–17 years:
- 250 mg twice daily, increased if necessary in severe infections to 500 mg twice daily.
In children with renal impairment, if estimated glomerular filtration rate (eGFR) is less than 30 ml/minute/1.73m2:
- Prescribe half the normal dose of clarithromycin.
- Avoid Klaricid XL® or clarithromycin M/R preparations.
In adults, prescribe 250 mg twice daily, increased in severe infections to 500 mg twice daily.
In adults with renal impairment, if the eGFR is less than 30 ml/minute/1.73m2:
- Prescribe half the normal dose of clarithromycin.
- Avoid Klaricid XL® or clarithromycin M/R preparations.
Co-amoxiclav
The treatment duration for AOM is 5–7 days.
For children:
- 1–11 months: 0.25 ml/kg of 125/31 suspension three times a day.
- 1–5 years: 5 ml of 125/31 suspension three times a day or 0.25 ml/kg of 125/31 suspension three times a day.
- 6–11 years: 5 ml of 250/62 suspension three times a day or 0.15 ml/kg of 250/62 suspension three times a day.
- 12–17 years: 250/125 mg or 500/125 mg three times a day.
In children with renal impairment:
- If the eGFR is 10–30 ml/minute/1.73 m2, prescribe the normal dose every 12 hours.
- If the eGFR is less than 10 ml/minute/1.73 m2, use the normal dose recommended for mild to moderate infections every 12 hours.
In adults, prescribe one 250/125 strength tablet three times a day; increased in severe infections to one 500/125 strength tablet three times a day.
In adults with renal impairment:
- If the eGFR is 10–30 ml/minute/1.73 m2, prescribe one 250/125 strength tablet every 12 hours or one 500/125 strength tablet every 12 hours.
- If the eGFR is less than 10 ml/minute/1.73 m2, prescribe one 250/125 strength tablet every 24 hours or one 500/125 strength tablet every 24 hours.
Erythromycin
The treatment duration for AOM is 5–7 days.
Children:
- 1 month to 1 year: 125 mg four times a day or 250 mg twice a day.
- 2 years to 7 years: 250 mg four times a day or 500 mg twice a day.
- 8 years to 17 years: 250–500 mg four times a day or 500-1000 mg twice a day.
In children with severe renal impairment, the dose of erythromycin should be reduced.
In adults, prescribe 250–500 mg four times a day.
In adults with severe renal impairment, prescribe a maximum daily dose of 1.5 g of erythromycin.
Summary
During this module you have learnt how to
- Make an accurate diagnosis of acute otitis media (AOM)
- Prescribe antibiotic and analgesic treatment in primary care, if appropriate
- Admit or refer to secondary care, if appropriate
- Manage people with persistent or recurrent AOM
- Give advice on measures to reduce the risk of recurrent episodes
Audit suggestions Review all cases coded as acute otitis media in the past 6-12 months Review all those prescribed antibiotics:
- Immediately
- Delayed prescription
- After a return appointment
- Is there a different strategy depending on the day of the week?
Review the notes in order to evaluate the antibiotic prescribing strategy in each case Share your findings across the practice Re-audit in 6-12 months
Resources
Atkinson H, Wallis S, Coatesworth AP. Acute otitis media. Postgraduate medicine 2015; 127(4), 386-390.
BMJ Best Practice (2018) Acute otitis media. https://bestpractice.bmj.com/topics/en-gb/39
de Lusignan S, Correa A, Pathirannehelage S, et al. RCGP research and surveillance centre annual report 2014-2015: disparities in presentations to primary care. Brit J Gen Pract 2017;67(654):e29-e40.
Finnikin S, Mitchell-Innes A. (2016) Recurrent otalgia in adults. BMJ 2016;354: i3917.
Kozyrskyj AL, Klassen TP, Moffatt M, et al. Short-course antibiotics for acute otitis media. Cochrane Syst Rev 2010;9:CD001095 https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD001095.pub2/full
Le Saux N, Robinson JL, Canadian Paediatric Society, Infectious Diseases and Immunization Committee. Management of acute otitis media in children six months of age and older. Paediatr Child Health. 2016; 21(1):39-50.
Lieberthal A, Carroll A, Chonmaitree T, et al. (2013) The diagnosis and management of acute otitis media. Pediatrics 2013;131(3):e964-e999.
Monasta L, Ronfani L, Marchetti F, et al. Burden of disease caused by otitis media: systematic review and global estimates. PLoS One 2012;7(4): e36226
Ngo CC, Massa HM, Thornton RB, et al. Predominant bacteria detected from the middle ear fluid of children experiencing otitis media: a systematic review. PLoS One 2016;11(3):e0150949
NICE NG91. Otitis media (acute): antimicrobial prescribing, 2018. https://www.nice.org.uk/guidance/ng91
NICE CG160. Fever in under 5s: assessment and initial management, 2013 (Updated 2017). https://www.nice.org.uk/guidance/cg160
Phillips JS, Yung MW, Burton MJ, et al. Evidence review and ENT-UK consensus report for the use of aminoglycoside-containing ear drops in the presence of an open middle ear. Clin Otolaryngol 2007; 32(5):330-336
Powers JH. Diagnosis and treatment of acute otitis media: evaluating the evidence. Infect Dis Clin North Am 2007;21(2):409-426.
Rosa-Olivares J, Porro A, Rodriguez-Varela M, et al. (2015) Otitis media: to treat, to refer, to do nothing: a review for the practitioner. Pediatr Rev 2015;36(11):480-486
Rosenfeld R, Schwartz S, Pynnonen M, et al. (2013) Clinical practice guideline: Tympanostomy tubes in children. Otolaryngol Head Neck Surg 2013;149(Suppl 1):s1-s35.
Rothman R, Owens T, Simel DL. Does this child have acute otitis media? JAMA 2003; 290(12), 1633-1640.
Schaefer C, Peters P, Miller R. (Eds.) Drugs during pregnancy and lactation: treatment options and risk assessment. London: Academic Press;2015
Schilder AG, Chonmaitree T, Cripps AW, et al Otitis media. Nature reviews. Disease primers. 2016;2:16063.
Shah UK. Advanced therapy of otitis media. In: Alper C, Bluestone C, Casselbrant M, et al. (Eds.) Acute otitis media/otitis media with effusion in craniofacial syndromes. edn. London: B.C. Decker; 2003 University of Michigan Health System.
Otitis media. Guidelines for clinical care, 2013. http://www.med.umich.edu/1info/FHP/practiceguides/om/OM.pdf
Related modules
View all Modules