QRISK4: What’s on the horizon in CVD risk assessment
JOANNE HAWS
JOANNE HAWS
RN MSc
Cardiovascular Nurse Specialist
MICHAELA NUTTALL
RGN MSc
Cardiovascular Nurse Specialist
Practice Nurse 2025;55(2):22-25
CVD risk assessment tools are continually evolving and the latest iteration of QRISK includes a number of ‘new’ risk factors that GPNs should be aware of as part of a holistic effort to reduce the burden of cardiovascular disease
Cardiovascular disease (CVD) incorporates a spectrum of disorders of the heart and blood vessels and is the leading cause of death globally.1 In the UK, CVD affects around 7 million people and accounts for almost a quarter of all deaths annually, many of which happen prematurely (in people under the age of 75 years).2 CVD also accounts for the largest gap in health life expectancy and significant health inequalities exist. A variety of conditions or habits, known as cardiovascular risk factors, increase an individual’s risk of developing CVD and key strategies focus on the identification and modification of these through clinical intervention and behaviour changes. Multiple CVD risk prediction tools are in use worldwide and in the UK, NICE recommends assessing people’s 10-year CVD risk using the QRISK tool every 5 years.3 Much of this work is undertaken in primary care and general practice nurses are at the forefront of assessing and communicating CVD risk and supporting individuals to reduce their risk through clinical intervention and lifestyle modification.
CARDIOVASCULAR RISK PREDICTION
The use of a validated CVD risk prediction tool facilitates a personalised estimation of an individual’s chances of having a heart attack or stroke in the next ten years. It also provides evidence for quantifiable thresholds for intervention in clinical guidelines and health policy. The QRISK algorithm has been developed by academics and clinicians working in the NHS. It is based on routine data collected from general practice clinical systems across the UK participating in the QResearch database, and hospital episode statistics (HES) data. It considers both modifiable and non-modifiable risk factors for CVD, and over time new iterations have included additional factors associated with increasing risk of developing CVD. Updating the tool in line with contemporary evidence from UK practice data supports best possible risk prediction across population groups, particularly those from vulnerable groups who might be further disadvantaged without targeted intervention.4
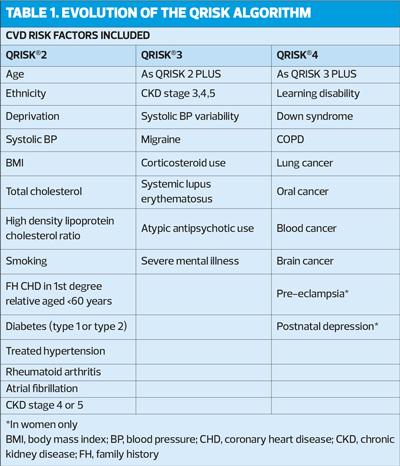
THE EVOLUTION OF QRISK
The QRISK tool was first introduced in 2007, and three years later a new version, QRISK®2, was developed to include lifetime risk, along with the more traditional 10-year absolute risk. The study of the QResearch database has led to many additional factors being incorporated into the tool over the years, with QRISK®3 published in 2017. Each version of the tool has been independently validated and compared favourably with globally recognised tools, particularly for the population of the UK. The evolution of the tool and the risk factors included can be seen in Table 1.
QRISK4?
After almost two decades of work in the field of CVD risk algorithms, a clinical paper detailing the development and validation of QRISK®4 (QR4) was published in April 2024.4 In addition to factors included in previous versions, QR4 takes into account learning disabilities, chronic obstructive pulmonary disease (COPD), many cancers, pre-eclampsia and post-natal depression. This further highlights the relationship between cardiovascular and mental health, along with the increasingly recognised role of inflammation in driving CVD, cancer development and chronic respiratory disease.5,6,7
Why have these factors been included?
The observation of association between the newly included conditions and CVD in the database population was significant enough to warrant their inclusion in the QR4 tool as new independent predictors of CVD risk. In practical terms, their inclusion should facilitate increased identification of higher risk individuals at a younger age, and targeted offers of risk-reducing interventions to these population groups.
Cancer
The findings regarding QR4 for cancer confirmed associations with four cancers – blood, brain, lung and oral cancers. The authors accounted for reduced life expectancy and pointed out that the increased risk, communications and interventions need to be considered in the context of the prognosis of cancers; but given overall increased survival rates there is much to be gained from targeted prevention in this group.4
COPD
An almost 2-fold increased risk of CVD was observed in people with COPD, the strongest association being in women. Given the lack of association between CVD and asthma it further confirms the importance of confirming the diagnosis using spirometry to optimise management of individuals, including CVD risk reduction.
Down syndrome and learning disabilities
While the relationship is not fully understood, a 2-3-fold increased risk of CVD in people with Down Syndrome was observed. Hypotheses include premature ageing associated with the condition along with adverse cardiometabolic profiles as potential underlying causes. Whatever the cause, identification and management of CVD risk should be a key priority of personalised care to support continued improvements in life expectancy for this group.4
The prevalence of congenital heart defects is higher in people with learning disabilities than in the general population, as is obesity and diabetes. Unhealthy lifestyle behaviours including poor diet and physical activity are common, and although individuals known to specialist services are less likely to smoke and drink alcohol than the general population, rates are higher in those with mild learning disabilities.8
Pre-eclampsia
The increased risk of CVD associated with pre-eclampsia declined with age, but a 54% increase was observed at a mean age of 39 years, and this is reported to be consistent with other, related research. Damage to the maternal cardiovascular system has been cited as a potential driver of the development of atheroma and the inclusion of this factor could provide an important opportunity to target this group.
Postnatal Depression
The observation of increased CVD risk in women who have experienced depression after birth is consistent with the findings of the recent studies in this area. Links have been demonstrated with hypertension, ischaemic heart disease and heart failure in this group. Similarly to other emerging risk factors, the underlying pathways are yet to be fully understood but as with CVD, depression and anxiety generally, factors such as inflammation, alterations in the immune system and lifestyle changes may be implicated.9
WHAT DOES THIS MEAN IN PRACTICE?
QRISK is widely used in general practice across the UK as a predictor of CVD risk, both for individuals participating in the NHS Health Checks programme and for those diagnosed with high-risk conditions such as hypertension. The convenience of its availability within practice clinical systems templates has facilitated population of the data fields with information being taken directly from the individual’s clinical record, and the direct transfer of correctly coded results back to the record. It has not, however, been without controversy including regulatory concerns and the subsequent removal from some clinical systems.
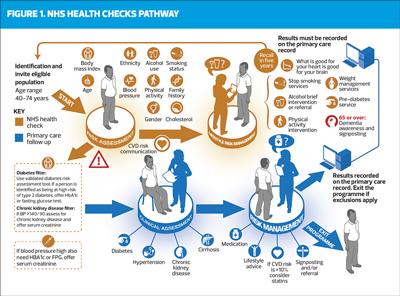
NHS Health Checks
The use of QRISK to estimate 10-year CVD risk has been integral to the NHS Health Checks programme since inception in 2009, when it was launched with the aim of reducing the risk of CVD by assessment of risk factors, raising awareness of risk factors, helping people to adopt healthier behaviours and by referring people to specialist services where appropriate (Figure 1). In 2020, the NHS Health Checks Best Practice Guideline was updated to reflect the transition from QRISK2 to QRISK3 in the web-based tool and provide recommendations for practice. It was noted that where QRISK3 was available this should be used and any increase in risk due to the newly included variables acted upon and communicated to the individual. Where QRISK3 is not available it was deemed appropriate to use QRISK2 and acknowledged that the individual may benefit from having a full QRISK3 score calculated in addition, recognising this would not be part of the original NHS Health Check. It was also noted that a surveillance review of the NICE guidance on 2018 concluded that a partial update of the guidance was warranted to provide advice on the use of QRISK3.10 Although it seems to be suggesting a pragmatic approach of using what is available at the time, it is easy to see how confusion develops!
Practicalities
One of the challenges around the use of the QRISK predictor tools is this issue around the practicalities of access and availability within the clinical systems, and importation of results to individual patient records. Many nurses and other general practice team members report being able to access only QRISK2 within the clinical system and are faced with switching between this and a web-based tool to be able to use QRISK3 and needing to manually input results into the patient’s record. This is not only time consuming and potentially distracting for the clinician and patient but could also potentially increase the risk of mistakes being made with data input.
CASE STUDY
Joy is a 57-year-old Black Caribbean woman recently diagnosed with stage one hypertension. In line with NICE guidance, she was screened for target organ damage (TOD) by checking her renal function, urinary albumin creatinine ratio (uACR), a 12-lead ECG and fundoscopy. Bloods were also taken for HbA1c, to monitor for diabetes, and lipid levels in preparation for a full cardiovascular risk assessment to inform her treatment options. There were no signs of TOD and, using QRISK3, Joy's 10-year risk of CVD was predicted to be 8.6%, placing her in the <10% lower risk category.
While this initial news could provide reassurance for Joy,Rob it does not tell the whole story.On closer examination of the outputs of the QRISK®3 web-based tool it provides both a relative risk score and a Heart Age to expand on her personal results.The relative risk provides a comparison of Joy personal risk to that of a person of the same age, gender and ethnicity as her who does not have her increased risk factors.
In Joy's case she has an increased blood pressure, raised LDL cholesterol, is overweight and has a family history of premature cardiovascular disease.This equated to a relative risk of 2.6, meaning Joy is over two and a half times more likely to have a heart attack or stroke in the next ten years than her ‘healthy’ counterpart. Furthermore, Joy's heart age was estimated to be 69 years, which is 12 years older than her chronological age.This tells a rather different story to the initial ‘lower risk’ result and may influence Joy's motivation to adopt lifestyle changes as well as any decision making in relation to clinical interventions to reduce her risk.
Doing ‘nothing’ is an option for Joy, as it is for any of us, but as her risk will only increase with advancing age and it’s only a matter of time before she crosses the threshold to the magic >10% without increasing any behaviour-related risk; the communication of her risk using all available information could be pivotal. Ultimately, regardless of the numbers generated by a risk prediction tool, most of us could do more to reduce our risk of CVD and a position in the lower risk category should not give us any false sense of security around unhealthy lifestyle choices.
Limitations
While the use of CVD risk prediction tools facilitates quantification of risk and thresholds for intervention on a population level, risk is on a continuum and focusing purely on numbers and categories can be counterproductive. First, it is acknowledged that risk may be underestimated in some population groups including women and in younger age groups. It also must be noted that not all established risk factors are included such as physical activity, salt intake, alcohol consumption and other dietary factors so a personalised approach and effective communication is essential to facilitate a meaningful patient experience and improved outcomes. The case study gives a good example of why this is the case.
CONCLUSION AND RECOMMENDATIONS
Keeping up with clinical updates of algorithms and guidance is a continuous challenge for all healthcare professionals, and even more so in a generalist setting where the constant flow of papers to read, digest and implement on a broad range of topics seems never ending.
While the opportunity of identifying increased CVD risk in additional groups is absolutely welcomed, particularly where there is potential for reducing health inequalities, the challenge of systems and guidance keeping up with the latest version of clinical tools remains a concern.
Having a good understanding of cardiovascular risk, including the development of atheroma, the concept of risk, evidence-based interventions and the impact of lifestyle will provide a solid foundation to all general practice nurses undertaking CVD risk assessment. Risk prediction tools will continually be updated; what is critical is the ability to communicate the risk calculated in a way that patients understand. The development of skills to facilitate the communication of individual risk and techniques to support behavioural change, such as motivational interviewing, will make a difference to the experience and outcomes of our patients and population. While the numbers are important, and the use of the most up to date tools are preferred, let’s not allow it to distract from the task in hand.
REFERENCES
1. World Health Organization. Cardiovascular Diseases. https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
2. NHS England. The NHS Long Term Plan; 2019. https://www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf
3. NICE Clinical Knowledge Summaries (CKS). CVD risk assessment and management; 2024. https://cks.nice.org.uk/topics/cvd-risk-assessment-management/
4. Hippisley-Cox J, Coupland CAC, Bafadhel M, et al. Development and validation of a new algorithm for improved cardiovascular risk prediction. Nat Med 2024;30:1440–1447. https://doi.org/10.1038/s41591-024-02905-y
5. Michal M, Beutel M. Mental disorders and cardiovascular disease: what should we be looking out for? Heart 2021;107:1756-1761.
6. Cuomo A, Mercurio V, Tocchetti CG. Inflammation at the crossroad between cancer and heart failure. Eur J Prev Cardiol 2024; 31(11): 1408–1409. https://doi.org/10.1093/eurjpc/zwae166
7. Rabe KF, Hurst JR, Suissa S. Cardiovascular disease and COPD: dangerous liaisons? Eur Respir Rev 2018;27(149):180057
8. Public Health England. Fingertips. Health inequalities: Cardiovascular Disease. https://www.google.com/url?sa=t&source=web&rct=j&opi=89978449&url=https://fingertips.phe.org.uk/documents/Health_inequalities_cardiovascular_disease.pdf&ved=2ahUKEwjp0vaoqM2LAxUNWUEAHb-QBhcQFnoECBQQAQ&usg=
AOvVaw3tfd3DgKZJla2BeQFpQPx0
9. Lu D, Valdimarsdóttir UA, Wei D, et al. Perinatal depression and risk of maternal cardiovascular disease: a Swedish nationwide study. Eur Heart J 2024;45(31): 2865-2875
10. Public Health England. NHS Health Checks. Best Practice Guidance for Commissioners and Providers. 2019 https://www.healthcheck.nhs.uk/commissioners-and-providers/national-guidance/
Related articles
View all Articles