Lessons in asthma: Improving the management of respiratory conditions in a primary school setting
Dave Edwards
Dave Edwards
BPharm, PGCE, DipEd, SP, IP.
Respiratory Pharmacist,
North and South Pembrokeshire Cluster,
Hywel Dda University Health Board
Practice Nurse 2024;54(3):16-21
Respiratory illness in children represents a burden for the child, the family and the healthcare system. It is a major cause of school absence, unscheduled care appointments and could potentially limit the child’s ability to have a full, unrestricted childhood. There have been repeated calls to improve the way we manage these conditions
Asthma is the most common long-term medical condition in children in the UK, with around 1 in 11 children and young people living with asthma.1 The UK has one of the highest prevalence, emergency admission and death rates for childhood asthma in Europe.2 Outcomes are worse for children and young people living in the most deprived areas.3
In Wales, approximately 58,000 children have been diagnosed with asthma. This equates to 11% of the population and is higher than in other areas of the UK.1 Two-thirds of school-age children with asthma will have an asthma attack in school.4 In the UK as a whole, almost 70 children are admitted to hospital due to asthma every day. In 2020, 10 deaths occurred in children between 0 and 14 years of age.1
The Royal College of Physicians (RCP) report, ‘Why asthma still kills: National Review of Asthma Deaths (2014) (NRAD)’5 found that poor perception of risk of adverse outcome was found to be an important avoidable factor in 70% of the deaths that were looked at, as well as poor prescribing practice, lack of a structured asthma review with a specialist and a lack of a personal asthma action plan. The findings and recommendations in this report are repeated in the NHS England’s 2021 report ‘National Bundle of care for Children and Young People with Asthma’6 and in annual audit reports from Asthma + Lung UK.7
Amongst the NRAD report recommendations were:
- A more structured review
- Training to be given on inhaler technique
- Every patient to have a personal asthma action plan
NRAD also recommended that the parents, children and those who care for or teach them, should be educated about managing asthma, emphasising the ‘how’, ‘why’ and ‘when’ they should use their asthma medications, recognising when asthma is not controlled and knowing when and how to seek emergency advice.
The Asthma + Lung UK Asthma audit 2023, ‘Raising the Bar’,7 highlighted that only 24% of the respondents in Wales reported receiving the basics of asthma care, which should include:
- An annual review,
- An inhaler technique check, and
- Having a written self-management plan.7
In addition to children with an asthma diagnosis or suspected asthma, the new All Wales Paediatrics Asthma Guidelines recommend a trial of preventative inhaled corticosteroid (ICS) for all those aged 3 to 5 suffering from recurrent ‘episodic wheeze’.8
Health has been a devolved matter since the late 1990s. Control over each country's health system has resided with each UK nation for the last 25 years. Each nation has a slightly different approach to very a similar aim to help people stay well and to get the best treatment when they are ill through services working together to help people stay healthy by providing care by the right people, in the right place and at the right time.9-12 A Healthier Wales looks to a person-centred approach to provide services outside of a healthcare setting, using the latest technology and medicines available, to proactively help people to stay well not just treat them when they become ill.12
The project described below addresses the need for change highlighted in the respiratory reports and audits, through a novel approach of conducting educational sessions and respiratory reviews in primary schools in Pembrokeshire.
The challenge of diagnosing and managing a condition with variable symptoms in a population age-group that does not routinely attend the surgery (and when they do are very much children in an adult world) is especially tricky. Relocating this interaction to their primary school, an environment they associate with learning and two-way conversations with adults, changes the power dynamic and makes it a much more productive encounter.
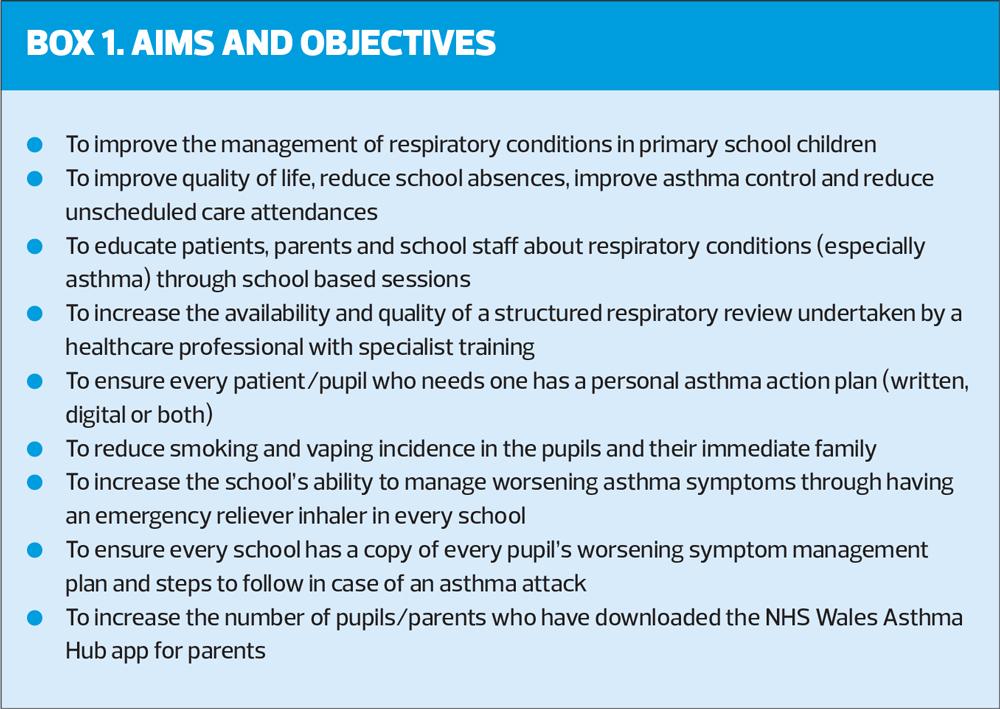
The aims of the project are summed up in Box 1.
DELIVERY
Over two years, the project will run in all 52 primary schools in Pembrokeshire. The schools are naturally grouped into clusters with a ‘parent’ secondary school. In the first term, we saw pupils from the Milford Haven cluster of six primary schools, with approximately 1,800 pupils.
Pupils were invited for a review if they had an asthma diagnosis, a reliever inhaler or were frequently absent due to respiratory issues.
The review took place with the pupil and the parent in the primary school. We had real time read/write access to the surgery system. The project necessitated good links between the surgery and the HCP doing the reviews. We had meetings beforehand (and regular check-ins) to ensure we worked together towards mutually beneficial goals.
At the review, the aims were to confirm a diagnosis; educate the pupil and parent about their condition, emphasising the importance of adherence and inhaler technique; treat according to guidelines (with greener healthcare a consideration) ensuring every pupil seen had an inhaler regime that they could and would use that gave them good control of their condition.
We ran some sessions alongside the respiratory reviews.
1. At the request of the school, we gave a talk on the dangers of smoking and vaping for the Year 5 and Year 6 pupils.
2. Following recommendations in the NRAD report, we held sessions for the school staff and for parents, covering:
a. Common childhood respiratory illnesses
b. Signs and symptoms of asthma
c. Action and use of inhaled therapy
d. Inhaler technique
e. What good asthma control looks like
f. Importance of having a worsening symptom management plan
We worked with the schools to increase their understanding of and ability to manage pupils’ worsening symptoms of asthma, including.
1. Distributing the Asthma + Lung UK poster ‘What to do if a child has an asthma attack’14
2. Encouraging the school to use the Asthma + Lung UK school asthma card for every pupil
3. Encouraging the school to have their own emergency reliever inhaler and giving appropriate spacers for their use
4. Giving the school a written copy of every pupil’s asthma action plan
We have written a policy for the use of an emergency inhaler in the primary schools in Pembrokeshire.
We reviewed 117 pupils with their parents. The majority were seen twice. Outcomes are given in Table 1.
IMPACT
Many of the patients had been seen for acute respiratory illness in the past 2 years, either by the GP or out of hours (OOH) services/A&E.
The parent feedback forms (total number 20) showed that few of the children who attended OOH or A&E were followed up. This lack of intervention is likely to lead to repeated unscheduled care visits and prescribing of rescue medication.
Despite most of the pupils with an asthma or suspected asthma diagnosis having had a respiratory review in the past 12 months, the findings at the initial consultation showed a general lack of understanding of the condition, poor preventer adherence and poor inhaler technique. Very few had a personalised asthma action plan to manage worsening symptoms.
Sixteen pupils were passive smokers. I offered their parents a referral to smoking cessation services, and four agreed to contact them. On follow up, three parents told me they had quit.
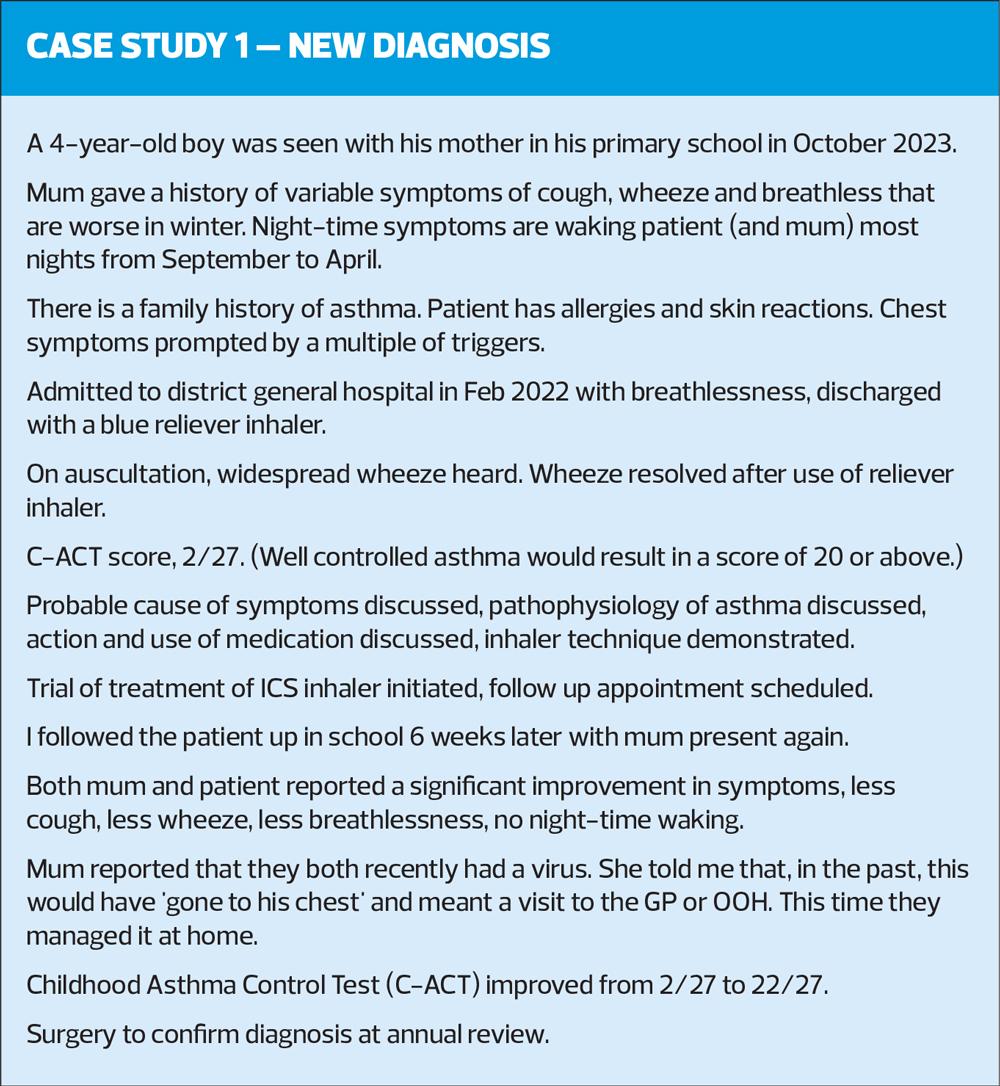
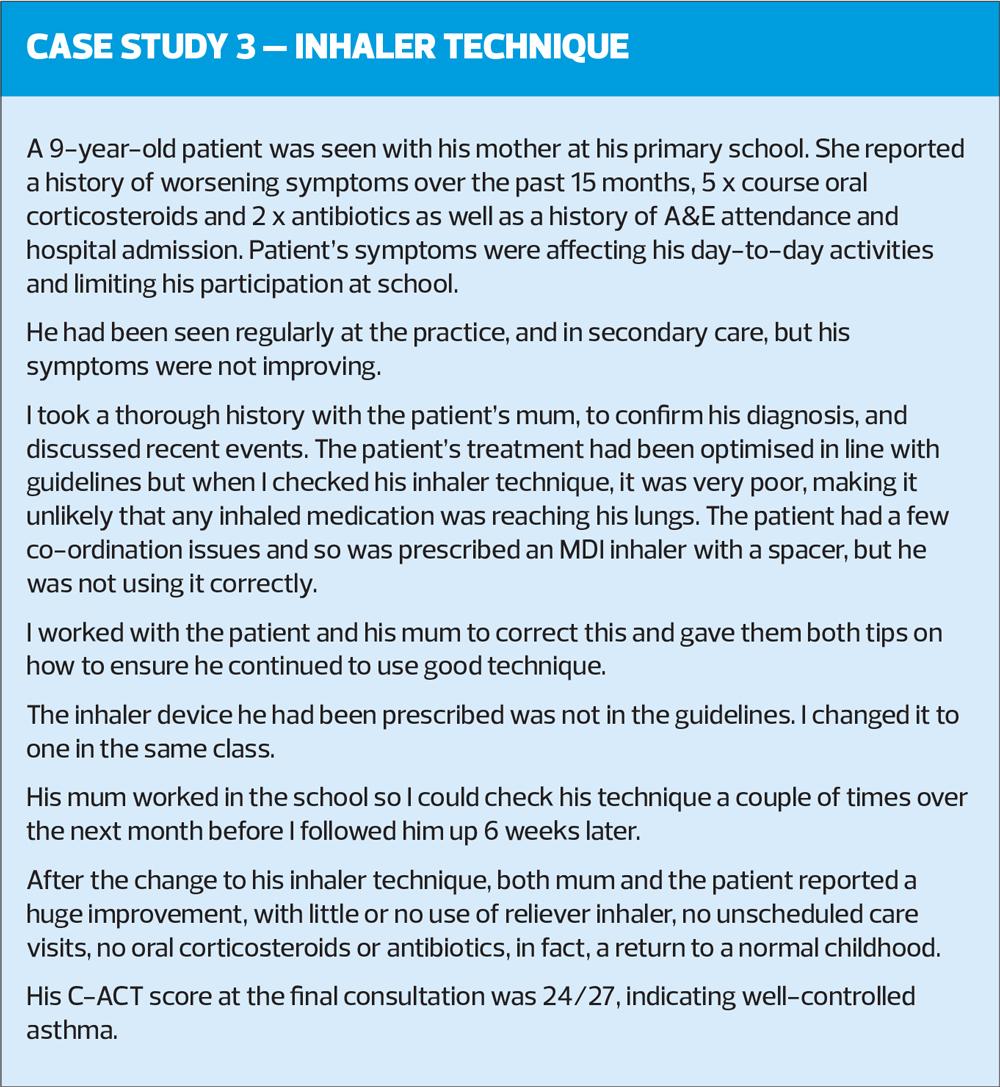
At the review, as well as other measures, I used a validated, quantitative test, the Childhood Asthma Control Test (C-ACT), to assess the patients’ symptoms and asthma control. I saw most pupils at least once and so could compare the C-ACT score at initial review and at follow up.
A C-ACT score of less than 20 indicates poor control of asthma, and the minimal clinical importance difference is 2 points.15
Results after the second consultation were positive. Over 60% of pupils reported a clinically important difference in their symptom control.
The number of critical errors in inhaler technique was also greatly reduced at follow up, but five patients still made one or more critical error. This illustrates the importance of checking technique at every opportunity.
Over 60% of patients had their treatment changed in line with the All Wales Guidelines. In general, prescribing for these patients was good. My most frequent changes to regime in line with guidelines were to change from 2 puffs of ICS twice daily to 1 puff twice daily of a higher strength ICS, or to try the patient on a dry powder inhaler (DPI) rather than a metered dose inhaler (MDI, over 6’s only). Both switches will reduce the carbon footprint of our prescribing.
Studies have shown us that patients who have a personalised asthma action plan (PAAP) are four times less likely to attend A&E than those without one.16 Only a minority of pupils had a PAAP but I issued a written NHS Wales pre-school wheeze and asthma management plan to every patient who was prescribed inhalers, and gave a copy of each plan to the school.
I encouraged every patient to download the NHS Wales AsthmaHub for Parents app, which contains educational material and a digital asthma management plan.
The quantitative outcomes (C-ACT scores, adherence, inhaler technique, treatment according to guidelines, percentage of DPIs prescribed, number of patients with a PAAP) all showed improvements after the interventions.
The qualitative outcomes (parental feedback, school feedback, surgery feedback) were positive. The parents reported a greater understanding of the condition, the action and use of inhalers and how to manage worsening symptoms. This should lead to improved adherence, better inhaler technique, better control and reduced unscheduled care and A&E attendances.
The schools reported an increased awareness of worsening symptoms and have seen an improvement in attendance in some pupils.
CONCLUSIONS
This project addresses a need that has been repeatedly identified by national audits and reports. The same reports tell us that the management of respiratory conditions is not improving. If anything, it is getting worse. The methods we are currently using are not working, so this project aims to improve outcomes by changing how we approach the problems.
The project aligns with the ambitions in the Welsh Government strategy outlined in ‘A Healthier Wales’ and the methods used fall within the structure of Accelerated Cluster Development and are scalable.
By any measure, the project could be classed as a success.
1.The target population engaged
The surgery feedback tells us that this age group does not regularly attend the surgery for reviews. I saw 117 pupils, which was 6.5% of the school population. Not all who were invited made an appointment, not all who made an appointment attended both consultations. The engagement and attendance rates are higher in the second cluster of schools.
2.The quantitative outcomes were positive
C-ACT scores improved by more than the minimal important clinical difference in 65% of the pupils. This indicates an improvement in asthma control and quality of life.
Inhaler technique of pupils improved after the intervention. Improved technique will lead to greater lung deposition of medication and improved asthma control.
More patients were being treated according to guidelines, which will improve their asthma control. The guidelines are also aligned with the NHS Wales Decarbonisation Strategic Delivery Plan,17 and increased guidelines adherence will mean a reduction in prescriptions of inhalers with high global warming potential.
Every patient with a respiratory diagnosis now has a written PAAP to manage worsening symptoms and has been given the link for the NHS Wales Asthma Hub for Parents app, which contains a digital version. The school also has a copy of this plan for every pupil. This is expected to mean that pupils with asthma are less likely to attend A&E.
3.The qualitative outcomes were positive
The feedback from parents was very positive. All reported that their knowledge and understanding of asthma, the action and use of medication, inhaler technique and, crucially, their understanding of how to manage any worsening symptoms, had increased, almost all reported that their child’s asthma control and quality of life had improved since the review.
The schools reported an increased awareness and increased confidence managing pupils with worsening symptoms and have seen an improvement in attendance in some pupils.
The practices reported that they thought it was a successful and worthwhile project capturing patients who do not regularly attend practice reviews.
This project started as a pilot in one primary school, seeing patients registered at one practice. It has already been revised and improved many times, and we are constantly learning and improving it. We have shown that the project can be scaled up to include many more practices and primary schools. These results are from the Milford Haven cluster (six primary schools). At present, we are working with the eight primary schools in the Fishguard cluster, and have seen patients from eight of the 13 practices in the North and South Pembrokeshire Clusters. At the end of two years, we will have run it in all 52 primary schools in Pembrokeshire and have seen patients in all 13 practices. It has huge potential to be adopted and spread more broadly.
ACKNOWLEDGEMENTS
This project would not be possible without the support, backing and encouragement of the North and South Pembrokeshire Clusters, Robert Street, Barlow House, Neyland and Johnston Surgeries and the primary schools in the Milford Haven cluster. The project is a Bevan Exemplar (Cohort 8) and is funded via the South and North Pembrokeshire Clusters within Hywel Dda University Health Board. The professional lead is Dr Helen Wang (South Pembrokeshire Locality Lead) and the project lead is Lucie-Jane Whelan Hughes (Primary Care Service Manager).
REFERENCES
1. Asthma + Lung UK, What is Asthma? 2024. https://www.asthmaandlung.org.uk/conditions/asthma/what-asthma
2. NHS England, NHS warning to parents as ‘asthma season’ hits. 2019 https://www.england.nhs.uk/2019/09/nhs-warning-to-parents-as-asthma-season-hits/
3. RPCPH, State of Child Health in the UK, 2020. https://stateofchildhealth.rcpch.ac.uk/
4. First Aid for Life, Asthma, swerve the September surge, 2024 https://firstaidforlife.org.uk/asthma-swerve-the-september-surge/
5. Royal College of Physicians, Why asthma still kills: the National Review of Asthma Deaths (NRAD) Confidential Enquiry report. 2014
6. NHS England, National Bundle of Care for Children and Young People with Asthma, 2021. https://www.england.nhs.uk/2021/national-bundle-of-care-for-children-and-young-people-with-asthma
7. Asthma + Lung UK, Raising the Bar, 2023. https://www.asthmaandlung.org.uk/raising-bar-improving-asthma-care-wales
8. All Wales Therapeutics and Toxicology Centre. All Wales paediatric asthma management and prescribing guideline; 2023. https://awttc.nhs.wales/medicines-optimisation-and-safety/medicines-optimisation-guidance-resources-and-data/prescribing-guidance/all-wales-paediatric-asthma-management-and-prescribing-guidelines/
9. Department of Health Northern Ireland, Health and Wellbeing 2026: Delivering Together, 2016. https://www.health-ni.gov.uk/topics/transformation-programme
10. Scottish Government, NHS Recovery Plan, 2021. https://www.gov.scot/publications/nhs-recovery-plan/
11. NHS England, NHS Long term Plan, 2018 https://www.england.nhs.uk/long-term-plan/
12. Welsh Government, A Healthier Wales, 2018 https://www.gov.wales/healthier-wales-long-term-plan-health-and-social-care
13. NHS Wales, Accelerated Cluster Development Toolkit, 2024 https://primarycareone.nhs.wales/tools/accelerated-cluster-development-toolkit/
14. Asthma + Lung UK, Asthma at school campaign, 2023 https://shop.asthmaandlung.org.uk/collections/asthma-at-school-campaign-poster
15. Bonini M, Di Paolo M, Bagnasco D, et al. Minimal clinically important difference for asthma endpoints: an expert consensus report. Eur Respir Rev 2020;29(156):19037
16. Adams RJ, Smith BJ, Ruffin RE. Factors associated with hospital admissions and repeat emergency department visits for adults with asthma. Thorax 2000;55(7):566-73
17. NHS Wales. Decarbonisation Strategic Delivery Plan; 2021. https://www.gov.wales/sites/default/files/publications/2021-03/nhs-wales-decarbonisation-strategic-delivery-plan-2021-2030-summary.pdf
Related articles
View all Articles