What links Cardiovascular-Renal-Metabolic conditions?
Dr Kevin Fernando
Dr Kevin Fernando
GP Partner, North Berwick Health Centre, Specialist Interests in Diabetes/CVRM & Medical Education
Professional writing assistance provided by Nida Khan, LCW Medical Communications
Practice Nurse 2024;54(1):10-13
Cardiovascular, renal and metabolic (CVRM) diseases are inextricably linked so there is a clear need for general practice nurses to move away from considering these conditions as separate entities and focus on management of CVRM holistically
Recognised among the most disruptive public health issues of the current century, chronic kidney disease (CKD), cardiovascular disease (CVD), and type 2 diabetes (T2D) affect the lives of millions of people worldwide.1 In the United Kingdom (UK), around 7.6 million people are living with CVD, around 3.5 million with CKD and an estimated 5 million with diabetes, of which 90% is T2D.2,3 Individually, each of these three conditions are associated with relevant morbidity and mortality.1 In the UK alone, CKD contributes to 40-45,000 premature deaths annually while CVD accounts for 27% of all deaths – that’s one death every 3 minutes.2,3
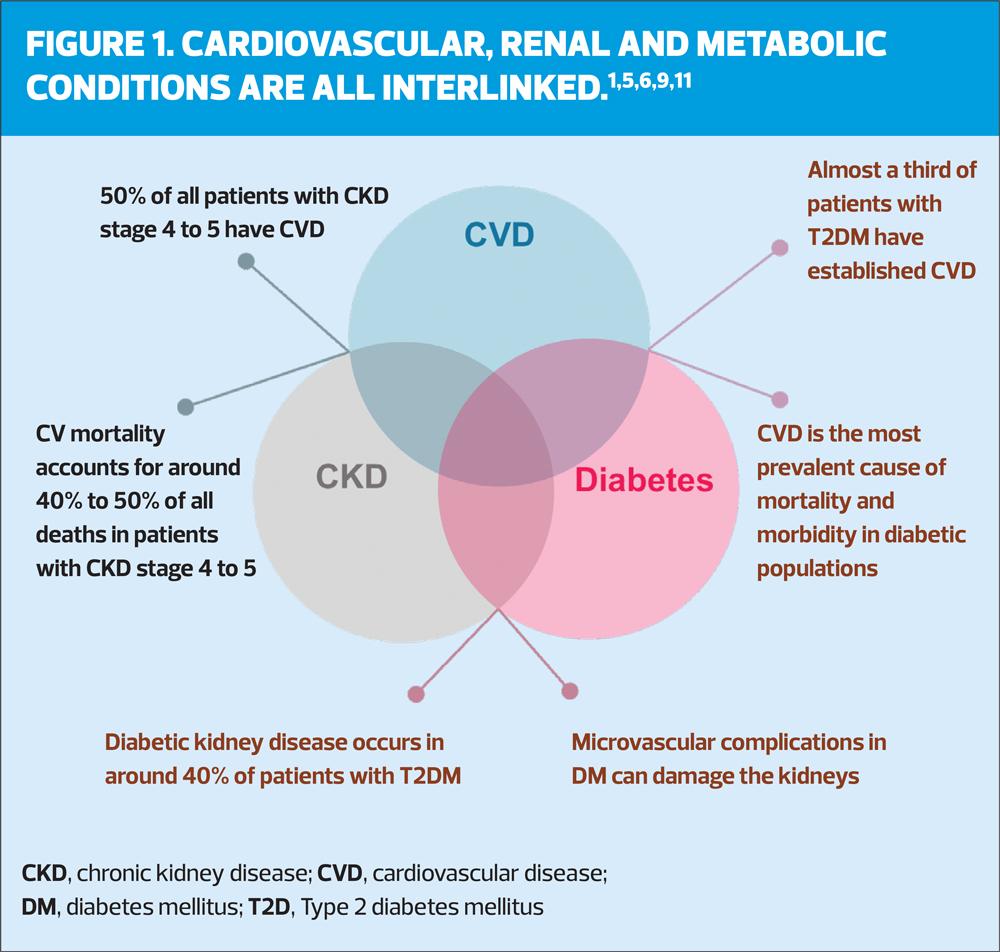
Often cardiovascular, renal, and metabolic (CVRM) conditions coexist in the same patients as they are intricately linked at the epidemiological, pathophysiological and molecular levels.1,4 For instance, half of all patients with CKD stage 4 to 5 have CVD and cardiovascular mortality accounts for around 40% to 50% of all deaths in these patients (Figure 1).5 CVD is also the most prevalent cause of mortality and morbidity in patients with diabetes; one third of adults with diabetes in the UK die from a heart or circulatory disease (Figure 1).2,6 The risk of CVD is 21% higher in optimally managed T2D patients compared with those without diabetes.7 Patients with diabetes alone have a reduction in life, this is further increased with the addition of CVD.8 For example, a 45-year-old female with diabetes dies ~8 years earlier than someone of the same age with no diabetes, but the same patient with diabetes and CVD dies almost 20 years earlier than someone of the same age with neither condition.8 A further complication of T2D is diabetic kidney disease (DKD) which develops in approximately 40% of patients.9 CVD and CKD in the presence of T2D worsen each other, leading to an increase in morbidity and mortality.10
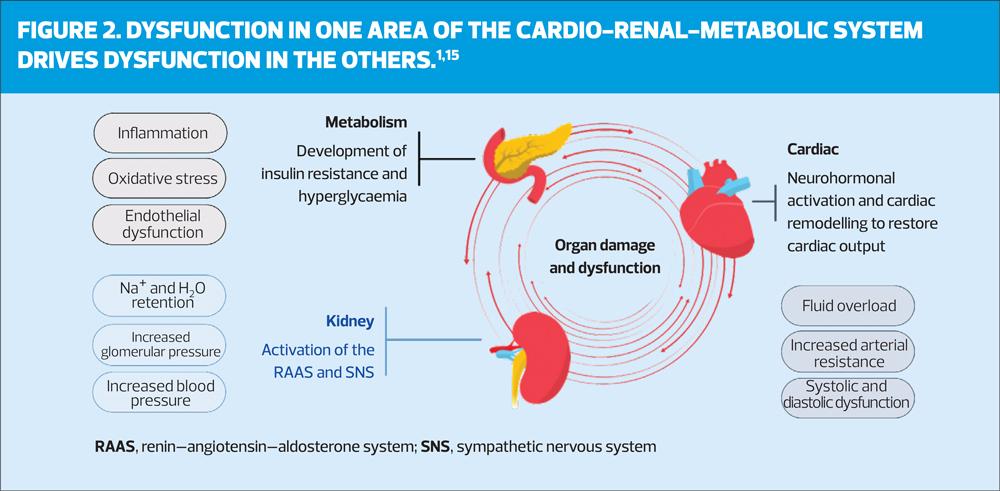
These closely interconnected CVRM conditions are common co-morbidities sharing many of the same risk factors.1,12 Elevated blood pressure and glucose, serum cholesterol, and body mass index are common risk factors of CVD; some of these factors also increase the risk of CKD and diabetes resulting in progression of interconnected disease.12 Dysfunction in one of the CVRM organs contributes to the dysfunction in the others (Figure 2).13,14 For example, increased adipose tissue can result in insulin resistance and eventual hyperglycaemia; this can lead to inflammation and fibrosis in T2D which can cause myocardial dysfunction contributing to heart failure (HF) and vascular damage.14 HF can reduce the kidney’s glomerular filtration rate (GFR) and exacerbate fluid retention leading to kidney dysfunction which drives further dysfunction in the heart and plays a key mediator of the relationship between metabolic risk factors and CVD14 (Figure 2).
General practice nurses (GPNs) along with other healthcare professionals (HCPs) can play a vital role in tackling the complexities of CVRM conditions and improving patient outcomes through early detection, treatment/management, prevention, and coordinated care. There is a clear need for GPNs to move away from considering CVRM conditions as separate entities and focus on management of CVRM holistically.
DIABETES
Patients with diabetes have elevated blood sugar levels over a prolonged period, which can cause blood vessel damage. Consequently, diabetes poses as a significant risk factor for CVD.2 It has been reported that patients with T2D have twice the risk of coronary heart disease, stroke and death from other vascular causes as those without diabetes.1,2 Although around 4.3 million adults in the UK have been diagnosed with diabetes, it is estimated that around 850,000 people remain undiagnosed.2 Current trends indicate the global burden of diabetes will continue to rise and it is predicted that by 2035, around 592 million people globally will have diabetes (1 in 10 persons).6 With the rising numbers of patients with diabetes and the issue of undiagnosed patients, early and accurate diagnosis is required to ensure effective management of the condition, its complications and its comorbidities including heart disease, stroke and kidney failure.2,6
Importantly, as CVD is the most prevalent cause of mortality and morbidity in patients with T2D, early and effective treatment is critical to tackle and improve the CV risk of these patients.6 However, this may be challenging as the relationship between diabetes and CVD is a complex one with multiple interconnections, common comorbidities and similar risk factors.1,12 Obesity, for example, is a CV risk factor which is also common in patients with T2D and is linked to high rates of CV morbidity and mortality.1,6 Patients with diabetes who are obese can develop insulin resistance which can lead to inflammation and lipid accumulation that can have harmful effects on blood vessels leading to endothelial dysfunction and the development of CVD.1,6 Weight loss is a key goal for overweight and obese patients with diabetes with treatment guidelines recommending a 5% weight loss over 4 years through lifestyle interventions.6
Nurses can encourage and support lifestyle changes in these patients to underpin all aspects of CVRM management. Although obesity and weight management may be a difficult subject, nurses can play a significant role in tackling this issue by talking to patients about their weight in a sensitive way and supporting them to achieve lifestyle modifications, including diet, weight management, smoking cessation, physical activity, and alcohol consumption.
T2D is also linked to kidney disease. On its own T2D can reduce life expectancy, which can be further reduced in those with both T2D and CKD and even further in patient with T2D, CKD and CVD.16,17 Diabetes contributes to CKD through microvascular damage (involving small vessels, such as capillaries) which can lead to complications such as nephropathy, retinopathy, and neuropathy.10 DKD is the leading cause of end-stage renal disease and its prevalence continues to rise as the prevalence of T2D increases. The major burden of DKD results from preceding microvascular and macrovascular (involving large vessels, such as arteries and veins) injury.10
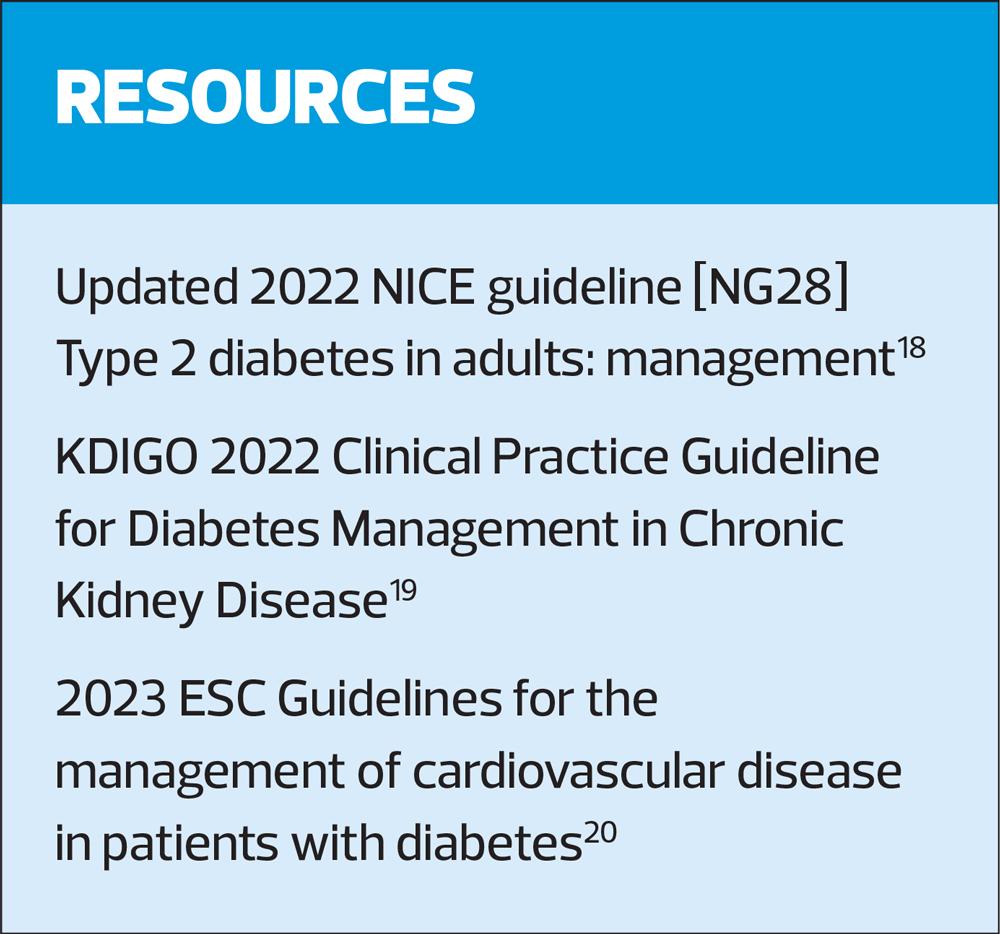
The focus of T2D management has been glycaemic control for decades. However, with the growing evidence supporting the existence of a strong multidirectional relationship among T2D, CVD and CKD, guidelines now also consider CV risk factor management, weight management and cardiorenal protection as important factors to consider in T2D.
CHRONIC KIDNEY DISEASE
CKD, defined by low eGFR or albuminuria that persists for ≥3 months, is a growing global public health problem.5 Aging populations, increasing prevalence of T2D and hypertension along with a low detection rate are some of the reasons for the increasing prevalence of advanced CKD.5,10
Cardiorenal syndrome (CRS) encapsulates the bidirectional association between the heart and the kidneys where a dysfunction in one of these organs is associated both directly and indirectly with dysfunction in the other.10,13 For example, CKD contributes to CVD through vascular calcification, whereby calcium deposit buildup can cause blockages within blood vessels increasing CV risk.5 Several comorbidities in addition to CKD, including diabetes, contribute to the progression of calcification, further increasing the CV risk.5 In CKD patients, the risk of developing CVD surpasses the risk of reaching end-stage kidney disease.5 As CVD is the primary cause of morbidity and mortality in CKD, with CKD patients 10–20 times more likely to die of cardiovascular causes, early identification and appropriate treatment of CKD is important to reduce CV risk.10
In terms of CKD identification, there are several tools available which nurses can use including The Kidney Failure Risk Equation which is recommended by the National Institute for Health and Care Excellence (NICE) CKD guideline NG203.21 These can be used to identify the risk of kidney failure in a patient and inform clinical management.
In terms of treatment, trials on sodium–glucose cotransporter 2 (SGLT2) inhibitors, glucagon-like peptide-1 (GLP-1) receptor agonists, and selective nonsteroidal mineralocorticoid receptor (MR) antagonists (finerenone) have shown cardiovascular as well as renal protective effects in patients with T2D.5,10 Data from these trials showing benefits across CVRM organ systems further support the notion of multi-organ physiology and pathophysiology of CVRM.
A good understanding of the risks associated with CKD can help nurses to discuss the condition with patients and bring up the topic of CVD and diabetes, which these patients may be at risk of developing. This can aid early diagnosis and provide opportunities to manage the risk of CVD to improve patient outcome and reduce CV mortality.
CARDIOVASCULAR DISEASE
In patients with CVRM disease, CVD is the leading cause of death.5,6 Although the exact cause of CVD is not clear, many risk factors including CKD and diabetes increase the chances of developing CVD.5,6,10 The direct and indirect costs of CVD to the NHS is estimated at £9 billion each year.2 There is also a wider economic impact: it is estimated CVD costs the UK economy £19 billion each year.2 Therefore, it is highly important to focus on better risk factor management and ways to improve CVD outcomes to avoid CVD events.
HOW CAN NURSES USE CVRM INSIGHT TO IMPROVE PATIENT OUTCOMES?
GPNs play an important role in the management of CVRM disease. They are in a position to educate patients on their conditions and provide vital support in terms of management and treatment. Therefore, an understanding of how CVRM conditions are interlinked and keeping up with latest information regarding CVRM disease is necessary to contribute to comprehensive patient care.
As CVRM consists of multiple conditions all related to each other, with common risk factors and pathophysiology, it can be challenging to accurately diagnose patients and plan their treatment. A multidisciplinary treatment approach is needed. GPNs may need to discuss a patient management and treatment plan with other HCPs in the team including diabetologists, cardiologists and pharmacists to ensure optimised patient care.
It is also important that GPNs know and understand the medication that their CVRM patients are taking, to enable them to explain the rationale for each specific medication and its importance. Some patients with CVRM conditions may be on multiple medications at once and may struggle with adherence. If nurses can provide some information on why the drug is prescribed to the patient, how it works and the adverse consequences of not taking them, it may help patients understand the importance of taking their medication. A good understanding of the drugs available for CVRM patients can also help nurses choose a treatment that tackles more than one condition. For example, a patient with CKD and CVD may benefit from SGLT2 inhibitors which can have both cardiac and kidney benefits.5,10 This way nurses can reduce polypharmacy and its related adverse events and possibly increase medication adherence in CVRM patient as they will have less medications to deal with.
Understanding of the relationship of CVRM conditions can be used to help inform patients about their conditions and the possible associated risks. For example, nurses can explain to T2D patients that their risk of developing heart disease and CKD are increased and can provide ways in which to improve the outcomes. They may be able to offer and encourage lifestyle management changes e.g. weight management, healthy eating and regular exercise. GPNs can also offer further testing if they feel a patient may be at risk of another CVRM condition. Measuring blood pressure, screening for blood glucose and cholesterol, and determining proteins in urine are some of the tests GPNs can carry out if they suspect a patient may be at risk of an interconnected CVRM condition.
CONCLUSION
CVD, CKD and T2D have established multidirectional relationships and lead to worse outcomes.10 As the prevalence of these conditions continues to rise, it is clear HCPs need to consider CVRM conditions holistically to achieve early detection and effective management and treatment.
Consider longer duration unified long-term condition reviews in primary care, where all comorbidities are considered, to promote a more proactive, holistic and preventive model of care.
- For any nurses who would like to further explore the latest clinical advances and national guidance surrounding the management of cardiovascular, renal and metabolic disease please register for the first CVRMUK Annual Meeting on Tuesday, 26 March 2024 at the King’s Fund, London: https://cvrmuk.com/events/34/cardiorenalmetabolic_uk_annual_meeting_2024
Related articles
View all Articles