Using Flash glucose monitoring in patients with type 2 diabetes
SU DOWN
SU DOWN
RGN, MSc, NMP
Nurse Consultant Diabetes
Editor-in-Chief Journal of Diabetes Nursing
Co-Vice Chair Primary Care Diabetes Society
Su Down received a fee from Abbott to write this educational article. Abbott has reviewed it for accuracy and compliance with regulatory codes of practice.
Job Code: ADC-69999
Date of Preparation: February 2023
Practice Nurse 2023;53(2):10-14
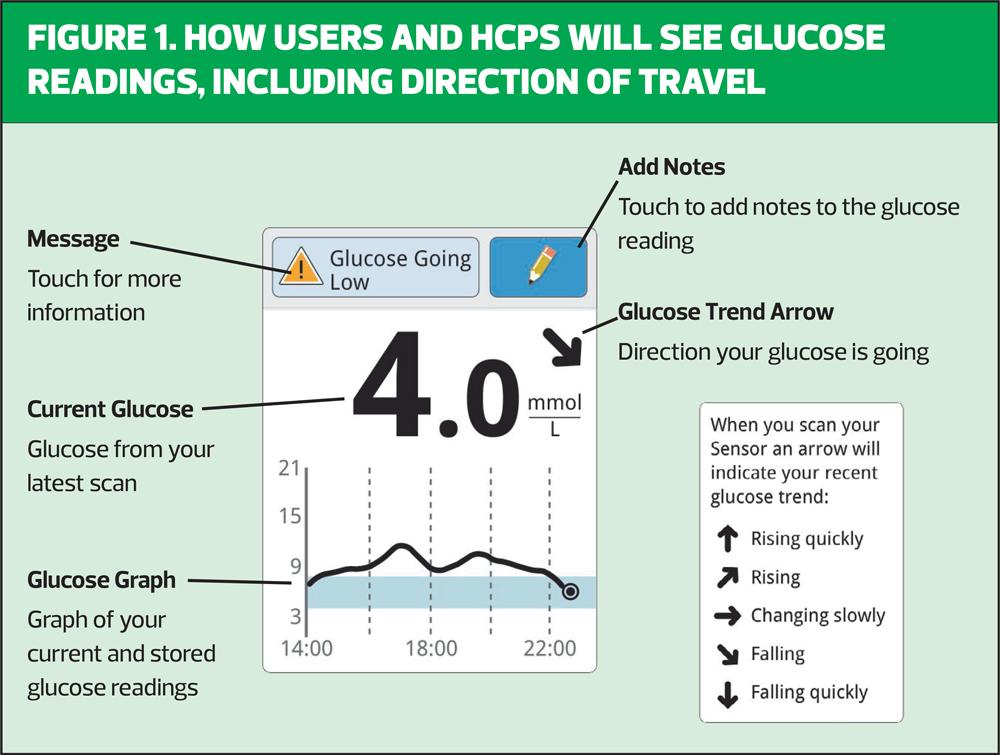
Using intermittently scanned continuous glucose monitoring in patients with type 2 diabetes is a relatively recent addition to practice and represents a major step forward in management: interpreting the data is an important skill for general practice nurses to develop
BACKGROUND
The use of intermittently scanned continuous glucose monitoring (isCGM), commonly known as ‘Flash’, has expanded rapidly and is likely to continue to increase, since NICE extended use to include some patients with type 2 diabetes.1
Patients who can access isCGM now include people living with type 2 diabetes on multiple insulin regimens, defined as those on two or more injections per day, if they also experience any of the following:
- Recurrent or severe hypoglycaemia
- Impaired awareness of hypoglycaemia
- Have a learning disability or cognitive impairment (limiting their ability to self-monitor)
- They would otherwise need to monitor at least 8 times a day
In addition, NICE recommends offering isCGM to adults with insulin-treated type 2 diabetes who would otherwise need help from a care worker or healthcare professional to monitor their blood glucose.1
This guidance clearly widens the use of this technology to a vast population whose diabetes is managed by primary care. As such, general practice nurses need to become confident in the use of this tech, as well the interpretation of the resulting data in order to optimise insulin regimens, or to support patients in the self-management of their diabetes.2
This article is intended to help support those in primary care who may be new to isCGM.
WHY UNDERSTANDING CGM IS IMPORTANT
The 2022 update to the NICE guidance for type 2 diabetes saw the greatest step forward for the use of technology to self-monitor diabetes since the advent of capillary blood glucose monitoring. Continuous glucose monitoring (CGM) has been available to some patients with Type 1 diabetes for many years; however, the advent of isCGM has opened this technology to a much wider group of patients.
When this technology was first launched, people could purchase it directly and a significant number of people chose to do so. isCGM first became available on the NHS in 2017. National audit data has demonstrated that use of this technology not only improves glycaemic control but can also improve hypoglycaemia awareness (impaired when repeated episodes of hypoglycaemia lead to reduced perception of symptoms of an impending episode) and decrease levels of diabetes distress (when the person feels overwhelmed by the burden of managing their condition). Consequently, the audit demonstrated a significant reduction in hospital admissions.3
Diabetes UK has been a main driver in a national campaign to widen the availability of this technology.4 By 2019, the target across the UK was to offer isCGM to 20% of the type 1 population, with additional advisory restrictions for this offering. However, based on the improvements seen from the audit data, the NICE guideline for Type 1 diabetes recommended offering this technology to all people with Type 1 diabetes, without any restrictions.5 This is a massive step, but the evidence indicates this should now be considered a core standard of care.
It is not surprising to see these benefits moving into the type 2 population, which represents 90% of the 4.9 million people in the UK living with diabetes.6 The position of NG28 in offering isCGM to those with type 2 diabetes, on two or more insulin injections a day, is likely to be just the starting point, with expansion, in time, to wider groups. Indeed, Wales has taken the step of offering isCGM to all those ‘on insulin’, irrespective of diabetes type.7
HOW FLASH DIFFERS FROM CAPILLARY BLOOD GLUCOSE MONITORING
General practice nurses need to understand the technology and how isCGM differs from capillary blood glucose monitoring. The only currently available isCGM is Abbott’s FreeStyle Libre 2 system. It consists of a sensor worn on the back of the upper arm, which measures the glucose level in the interstitial fluid via a tiny canula (the sensor tip). It takes a reading every minute and the sensor can store up to 8 hours of data.
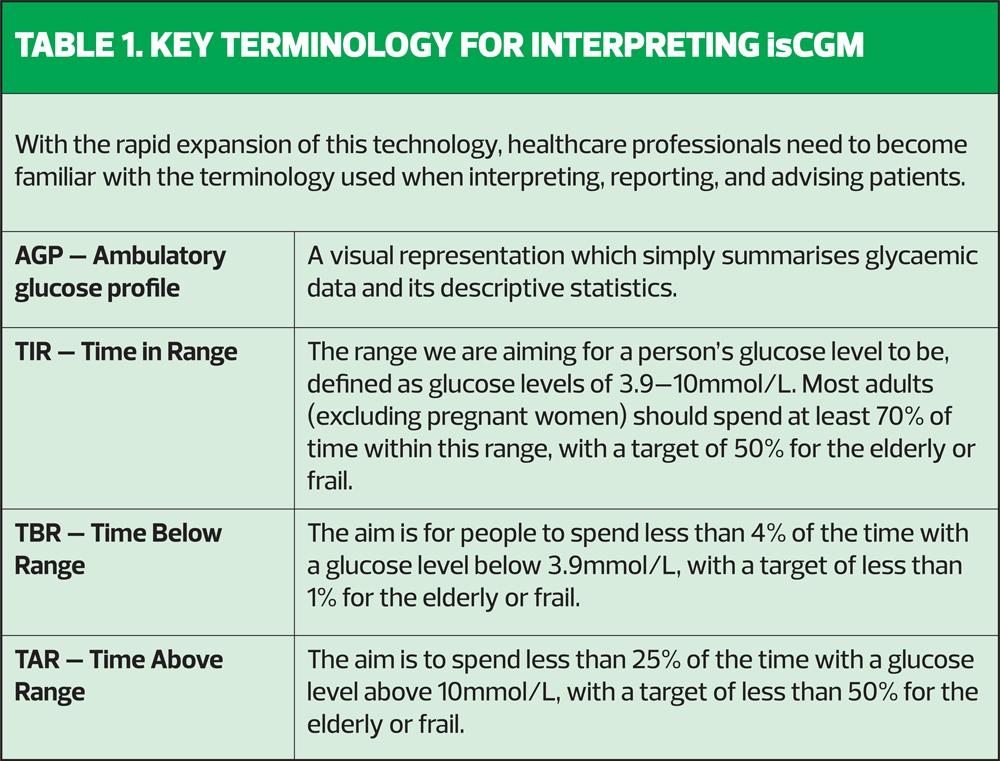
To capture this data, the sensor needs to be swiped with either a compatible smartphone, or a reader. This action retrieves the stored data and offers the person their immediate glucose level, a glucose trend arrow (this informs them if their glucose level is rising, falling, or staying stable), and a graph of glucose readings over the preceding 8 hours.
This has enormous benefits over capillary blood glucose testing, which is not only invasive, but also only offers a snapshot in time, with no indication of the direction in which the glucose level is going, or how quickly. In comparison, isCGM displays the actual glucose level at that point in time plus, importantly, an arrow indicating where the glucose levels are heading. It also indicates the speed of change and what the glucose level has been over last 8 hours (Figure 1).
If scanned at least once every 8 hours through the day, it provides a complete 24-hour glucose profile. However, if it is not scanned within an 8-hour window, the glucose profile will be incomplete.*
(*The FreeStyle LibreLink app and the FreeStyle Libre 2 reader do not share data with each other. Users of the system who use both the app and the reader need to scan their sensor once every eight hours on both devices for a full glycaemic picture on each device.)
The sensor stays on the arm for 14 days and can be scanned as often as the person wishes. This allows them to track their readings and where their levels are heading, in order to take any necessary action to avoid a hypoglycaemic event.
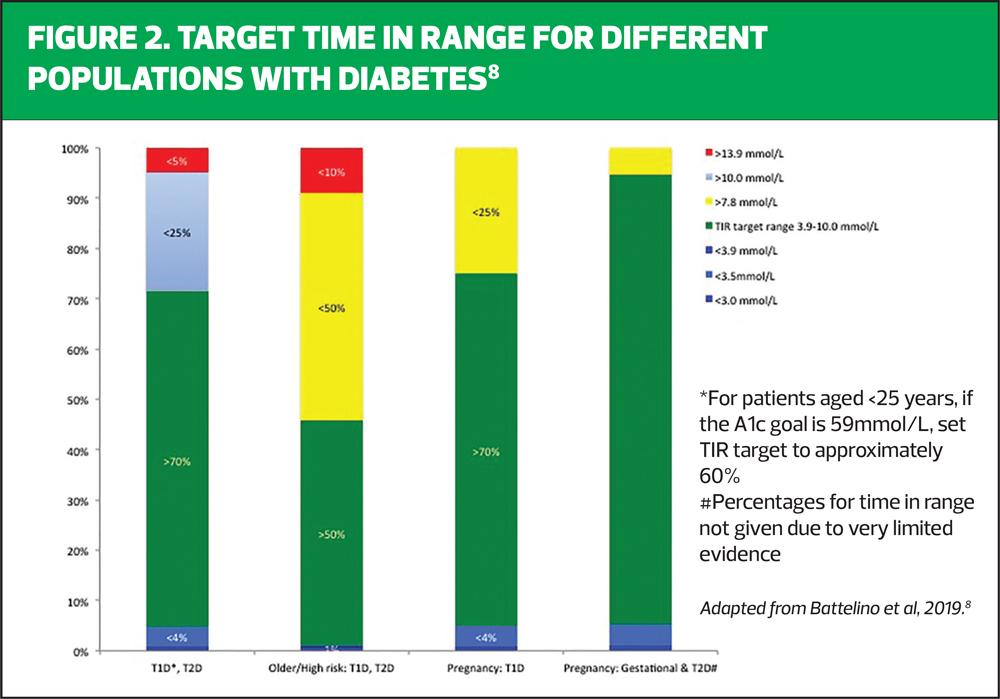
The range of glucose level aimed for is 3.9–10mmol/L, and the percentage of time spent with a glucose level in this range is displayed as the ‘Time in Range’ (TIR). If greater than 70% of the time is achieved in range this equates to an HbA1c of 53mmol/mol.
For some people with diabetes, we aim for a more relaxed HbA1c target. For example, in the frail or elderly population the aim is to maintain their glucose levels across the day at 6-15mmol/L with an HbA1c target of 64-75mmol/mol, depending on their level of frailty. For this population the TIR is set at up to 50%, with an emphasis on prevention of hypoglycaemia, which means the ‘Time Below Range’ (TBR) target is set at less than 1%. Therefore, the different TIR targets reflect current best practice for the achievement of glycaemia in the different cohorts of people with diabetes (Figure 2).8
HOW ARE isCGM DATA DISPLAYED?
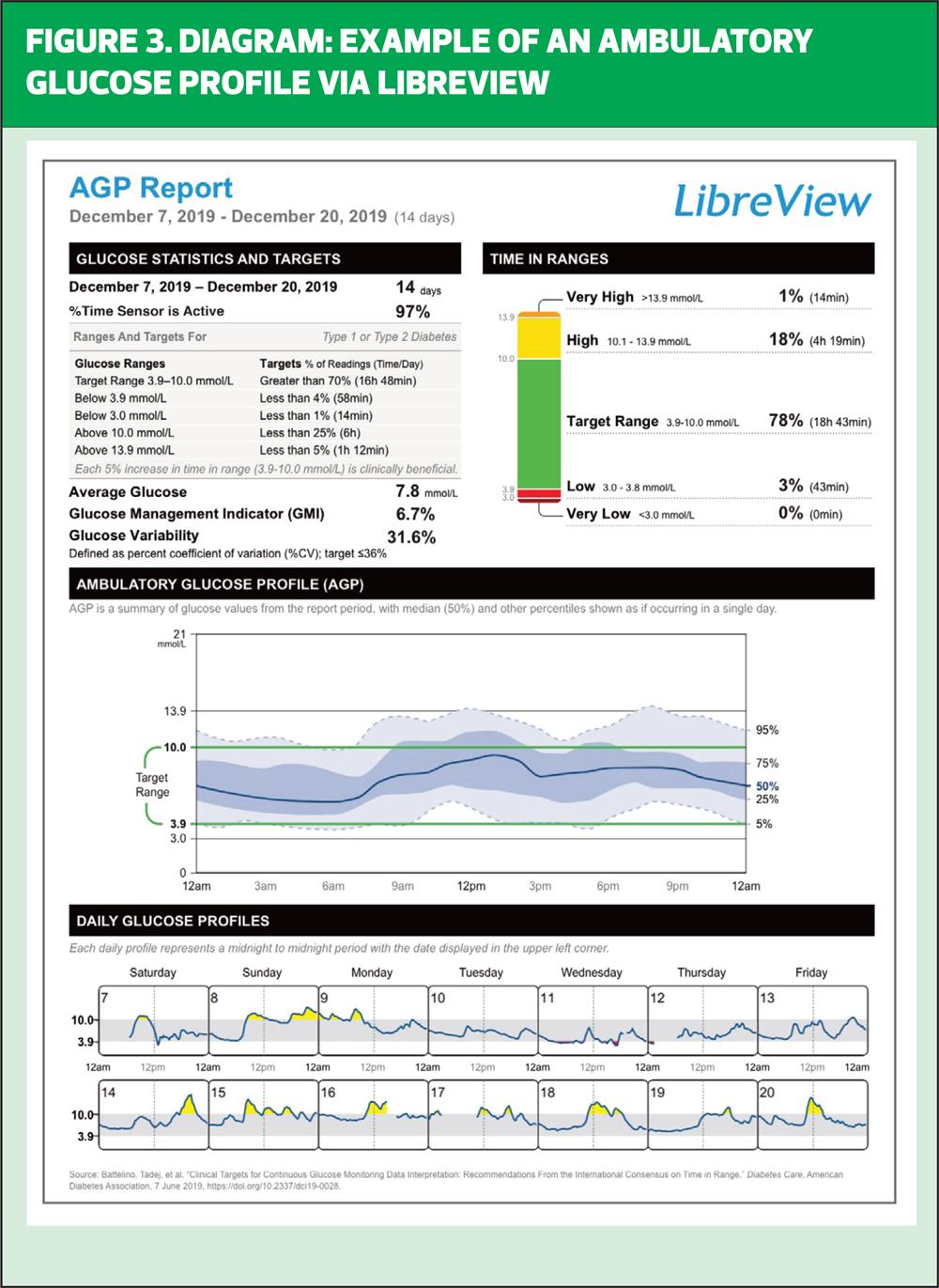
The data from the isCGM glucose monitor are displayed as an ambulatory glucose profile (AGP) report (Figure 3), which can be viewed via the patient’s reader, a smartphone or, if the patient consents to sharing their data, by the secure cloud-based data sharing platform, LibreView.
Ambulatory Glucose Profile (AGP) Graph
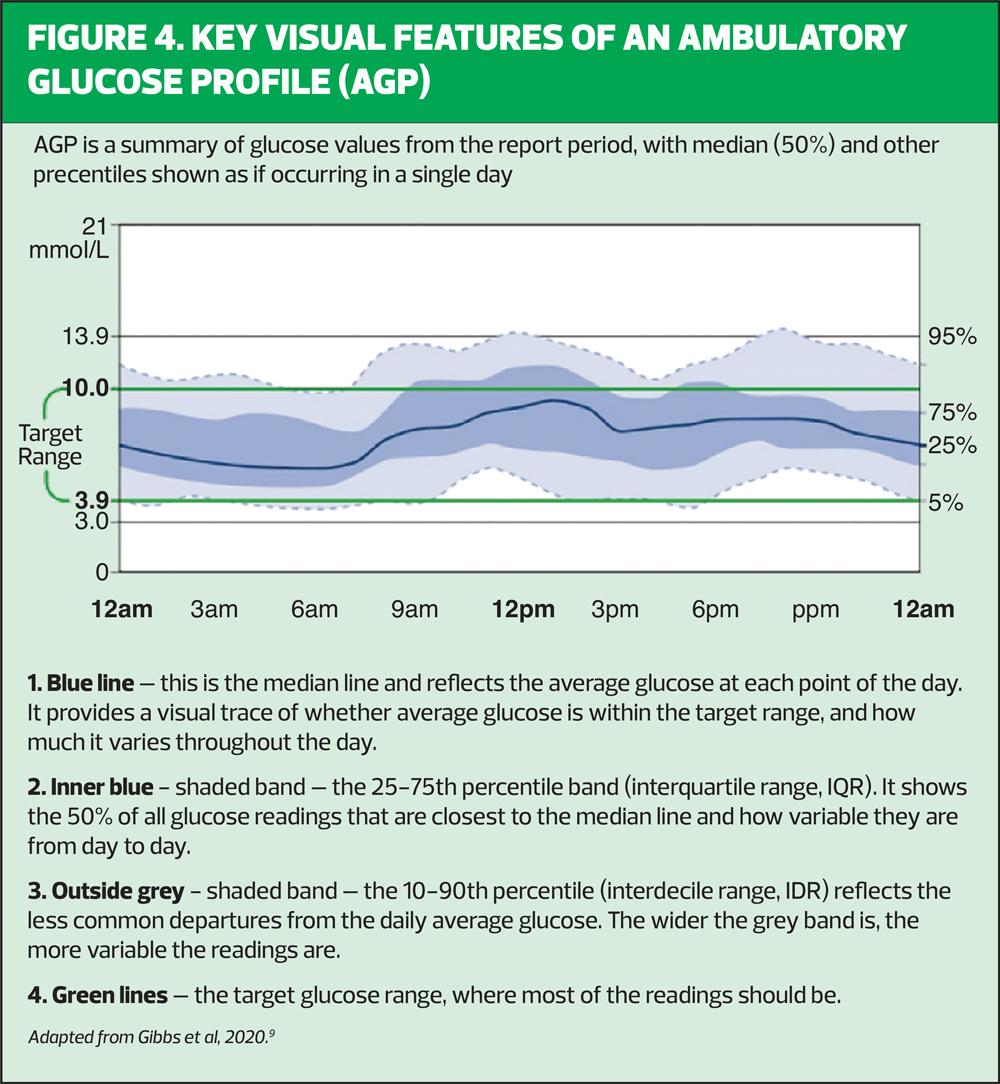
The AGP takes 14 days’ worth of data and displays it as one 24-hour graph (Figure 4). The AGP also provides other important data such as a graph of each individual day that has made up the 14-day profile, the percentage of time the sensor has been active, the average glucose reading across the 14 days, the glucose variability, and the predicted HbA1c result.
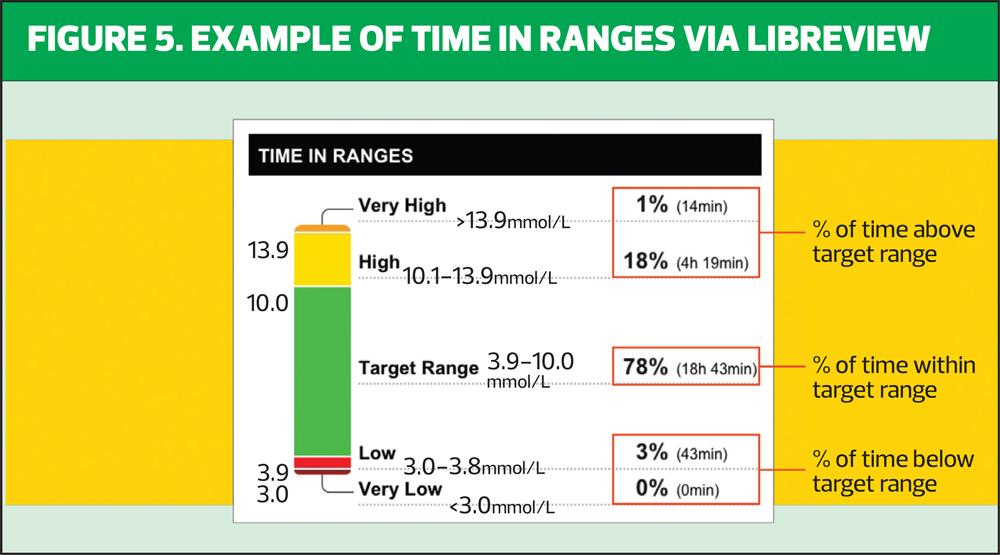
Time in Range ‘Thermometer’
The ‘thermometer’ display (Figure 5) provides the percentage time in range achieved along with the percentage of time spent above or below the target range of 3.9 to 10mmol/L, colour-coded to interpret how much Time in Range is being achieved.
MEANINGFUL CONVERSATIONS DRIVEN BY DATA
As this technology provides a 24-hour graph of the glucose profile, the healthcare professional needs to think differently about how to interpret the data to support people to achieve the greatest Time in Range possible, with minimal time spent in hypoglycaemia or prolonged periods of Time Above Range.
Having access to this amount of data can at first appear daunting for both the person with diabetes and the healthcare professional, with the perception that consultations may take much longer. However, in practice, once familiar and confident with the data presentation, consultations can be far more rewarding and meaningful for both parties.
Often people with diabetes report that, after using isCGM, their diabetes ‘finally makes sense’. For the first time, they can see directly and immediately the effects that food, exercise, alcohol, timing of injections and multiple other factors can have on their glucose control. The impact of seeing the direction of glucose travel allows the person to take pre-emptive action to prevent a hypo by responding to a downward arrow if it is indicating that hypoglycaemic levels may be reached very soon. Optional alarms can also alert the person to an impending hypo if they have not scanned the device, or alert them to a glucose level rising above their target level.
The basis of the healthcare professional’s role to improve glucose control, whether looking at monitoring diaries, capillary blood glucose monitoring or the AGP, has always been to identify a regular pattern emerging from the glucose data, identify the potential cause of those patterns and to offer advice and guidance to improve the glucose profile and increase the time in target range.
This fundamental has not changed whether monitoring diaries or capillary blood glucose readings, but the additional data afforded by an AGP allow for greater clarity in recommendations and advice offered, therefore helping the person achieve their optimal time in range.
The foremost limiting factor for achieving tight glycaemic control is hypoglycaemia, or fear of hypoglycaemia.10 In addition, the knowledge that longstanding hyperglycaemia increases the risk of long-term diabetes complications,11,12 and the emerging evidence that large swings in daily glucose control, referred to as glycaemic variability, is an independent factor for increasing cardiovascular risk.13
Given this evidence, the main aim to improving glycaemic control using the data from isCGM is to approach it in a three-step manner.
1. Firstly, to address any existing hypoglycaemia and any areas of risk of hypoglycaemia
2. Second, address any prolonged periods spent above target in hyperglycaemia
3. Finally, to reduce glycaemic variability
SUMMARY
Access to isCGM technology, or Flash glucose monitoring, is rapidly expanding to even more people with diabetes, many of whom will be solely managed in primary care. There is clear evidence that the use of isCGM can improve diabetes control and reduce the risk of hypoglycaemia, so this is a great step forward. The expansion of access to this technology means general practice nurses now need to increase understanding of the way these technologies present the data and how to interpret it.
By building familiarity and confidence with interpreting isCGM data, as outlined in this article, we can ensure that patients using this technology can be optimally supported their primary health care team.
REFERENCES
1. NICE NG28. Type 2 diabetes in adults: management; 2022 https://www.nice.org.uk/guidance/ng28
2. Millson V, Hammond P. How to analyse CGM data: A structured and practical approach. Journal of Diabetes Nursing 2020;24:JDN135
3. Deshmukh H, et al. Effect of Flash Glucose Monitoring on Glycemic Control, Hypoglycemia, Diabetes-Related Distress, and Resource Utilization in the Association of British Clinical Diabetologists (ABCD) Nationwide Audit. Diabetes Care. 2020 Sep; 43(9): 2153–2160.
4. Diabetes UK. NICE guidelines recommend wider use for flash and CGM: press release; 2022. https://www.diabetes.org.uk/about_us/news/nice-guidelines-recommend-wider-use-for-flash-and-cgm
5. NICE NG17. Type 1 diabetes in adults: diagnosis and management; 2022 https://www.nice.org.uk/guidance/ng17
6. Diabetes UK. Diabetes diagnoses double in last 15 years: press release; 2021. https://www.diabetes.org.uk/about_us/news/diabetes-diagnoses-doubled-prevalence-2021
7. Health Technology Wales. Freestyle Libre flash glucose monitoring; 2021. https://healthtechnology.wales/reports-guidance/freestyle-libre-flash-glucose-monitoring/
8. Battelino T, Danne T, Bergenstal R, et al. Clinical Targets for Continuous Glucose Monitoring Data Interpretation: Recommendations from the International Consensus on Time in Range. Diabetes Care 2019;42(8):1593-1603.
9. Gibb F, Jennings P, Leelarathna L, Wilmott E. AGP in daily clinical practice: a guide for use with the FreeStyle Libre flash glucose monitoring system. British Jounal of Diabetes 2020; 20:32-40. doi.org/10.15277/bjd.2020.240
10. American Diabetes Association (2019). Glycemic targets: standards of medical care in diabetes—2019. Diabetes Care 2019;42:S6170. https://dx.doi.org/10.2337/dc19-S006
11. Nathan DM,Genuth S, Lachin J, et al, for the Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. New Engl J Med 1993;329:97786
12. Stratton IM, Adler AI, Neil AH, et al. Association of glycaemia with macrovascular and microvascular complications of Type 2 diabetes (UKPDS 35): prospective observational study. BMJ 2000;321:40512. https://dx.doi.org/10.1136/bmj.321.7258.405
13. Ceriello A, Monnier L, Owens D. Glycaemic variability in diabetes: clinical and therapeutic implications. Lancet Diabetes Endocrinol 2018;7:221–30. https://dx.doi.org/10.1016/S2213-8587(18)30136-0
Related articles
View all Articles