Obesity for general practice nurses
DR GERRY MORROW
DR GERRY MORROW
MB ChB, MRCGP, Dip CBT
Medical Director Clarity Informatics and Editor, Clinical Knowledge Summaries
Practice Nurse 2021;51(1):8-12
Sometimes patients may ask you for advice about their weight, more often the subject will come up during discussions about lifestyle as part of health promotion, cardiovascular disease prevention, or the management of type 2 diabetes – so a thorough knowledge of obesity, its risks and management is essential
Broaching the subject of weight, obesity and weight management is a potentially challenging issue for practice nurses. You should approach the subject of weight carefully because people who are overweight or obese may be sensitive about discussing it or feel that their presenting problem is being overlooked.Ensure there is sufficient time to provide information and answer any questions and encourage the person's partner or spouse to support any weight management programme, as they can influence both the person's decision to seek treatment and their adherence to treatment recommendations or lifestyle changes.
WHAT IS OBESITY?
The terms obesity is used to describe excess body fat.
Different weight classes are defined according to a person's body mass index (BMI)1
- Healthy weight — BMI of 18.5–24.9 kg/m2
- Overweight — BMI of 25–29.9 kg/m2
- Obesity 1 — BMI of 30–34.9 kg/m2
- Obesity 11 — BMI of 35–39.9 kg/m2
- Obesity 111 — BMI of 40 kg/m2 or more
WHAT ARE THE CAUSES AND RISK FACTORS?
Obesity results from an imbalance between energy intake and energy expenditure. This can be influenced by a number of factors, including lifestyle, genetics, medical conditions and medications.
A diet high in sugar and fat has been implicated as a risk factor for obesity.2 Excessive alcohol consumption (more than 2 drinks per day) is also a risk factor for obesity.3 In addition, over the past 50 years, physical activity has declined significantly in the UK.2
Social and psychological factors may also play a part in the development of overweight. Some people with low self-esteem or depression may over-consume foods high in fat, sugar, and calories.
There are also a range of specific genes associated with excess weight.3,4 Obesity-related genes can affect the metabolism of food, fat storage, and a person's behaviour.2,5
Medical conditions, including genetic syndromes associated with hypogonadism, hypothalamic damage, polycystic ovary syndrome, growth hormone deficiency, Cushing's syndrome and hypothyroidism are also associated with obesity.3,4,6
Some medications may cause weight gain, including:
- Pizotifen
- Beta-blockers
- Corticosteroids
- Lithium
- Antipsychotics — especially atypical antipsychotics
- Anticonvulsants — sodium valproate, and gabapentin.5,7,8
Other risk factors include Increasing age, peri-and menopause, previous pregnancies, lower educational attainment, and lower socioeconomic status.3
HOW COMMON IS IT?
Obesity is a growing global health problem.1,9 In the UK, more than 1 in 4 adults is obese, and about 35% of the population are projected to be obese by 2030.10
WHAT ARE THE COMPLICATIONS?
Obesity is one of the leading causes of death and disability worldwide. Overweight and obesity are associated with an increased risk of developing several chronic diseases and conditions, including:
- Type 2 diabetes
- Coronary heart disease
- Hypertension and stroke
- Decreased life expectancy
Life expectancy is reduced by 2–4 years in people with a body mass index (BMI) of 30–35 kg/m2, and by 8–10 years in people with a BMI of 40–50 kg/m2.11
In addition, obesity places significant effects on demands on the health service and the economy,
WHAT IS THE PROGNOSIS?
Most of the complications of obesity can be reduced by weight loss.2,5 However, since obesity is a chronic disease, weight management needs to be lifelong.12
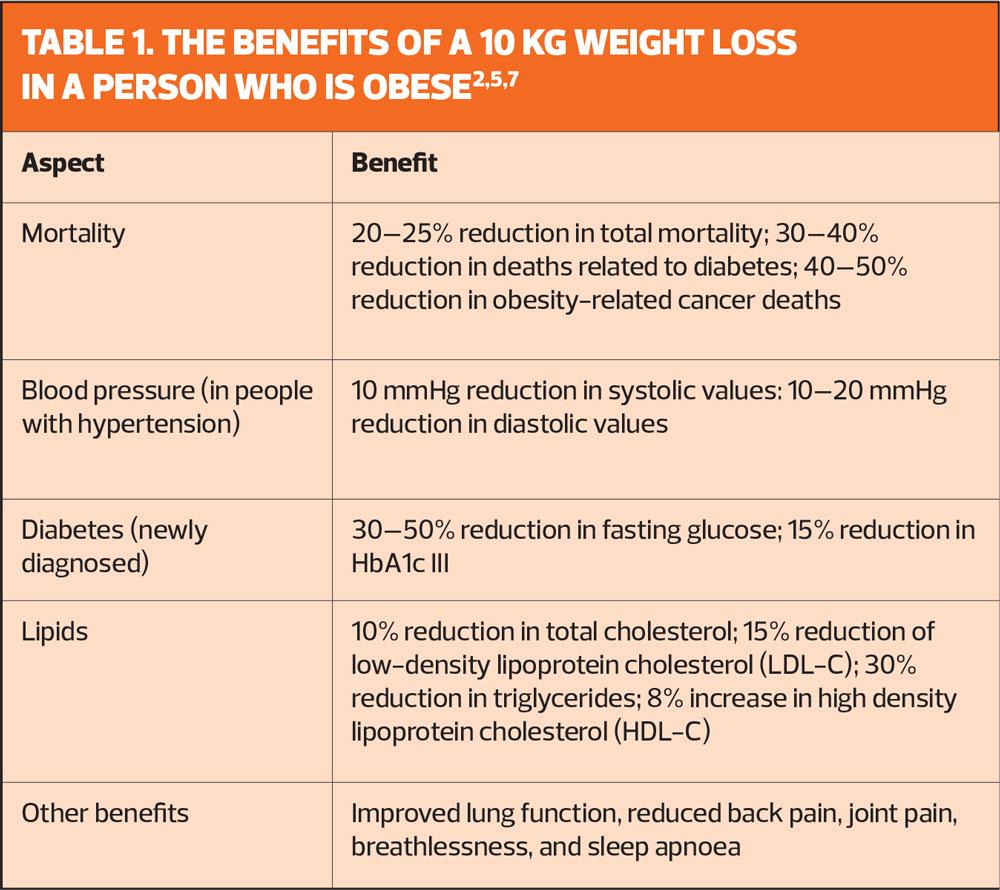
There is good evidence that significant clinical benefits may be achieved even by modest weight loss and lifestyle modification.12 See Table 1 for a summary of the benefits of modest weight loss.
DIAGNOSIS OF OBESITY
Practice nurses should calculate the person's BMI by dividing their weight in kilograms by the square of their height in metres.
It is important to interpret BMI with caution in very muscular adults and in people with atrophy, as it is a less accurate measure of adiposity in these groups.
MANAGEMENT
The Public Health England (PHE) guidance on Adult weight management: a guide to brief interventions13 includes a step-by-step guide to brief interventions with adults, which offers advice on practice nurse consultations with overweight and obese people regarding weight loss. These principles include assessing the person's willingness and motivation to lose weight, their feelings about being overweight and their confidence in making changes.
Assessment should also cover underlying causes and comorbidities, and the person's risk of developing complications of obesity.
Questions which may help to clarify a person's readiness to lose weight include:
- Are you concerned about your weight?
- How important is it for you to lose weight now?
- What would have to change in your life for you to be able to tackle your weight?
- Is your weight affecting your life in any way now?
Barriers to lifestyle change include lack of knowledge about food, diet, and exercise; the cost and availability of healthy foods; lack of time; views of family and community members; low levels of fitness, or disability; and low self-esteem and lack of assertiveness.
You should take a detailed history, including:
- Medical conditions that can contribute to overweight and obesity, or complications, especially unrecognised comorbidities (for example sleep apnoea)
- Management of comorbidities
- Family history (for example family history of obesity and diabetes)
- Medication history
- Social history (for example lifestyle, diet, exercise, alcohol, and smoking)
Examine the person and check their blood pressure, and measure their waist circumference.
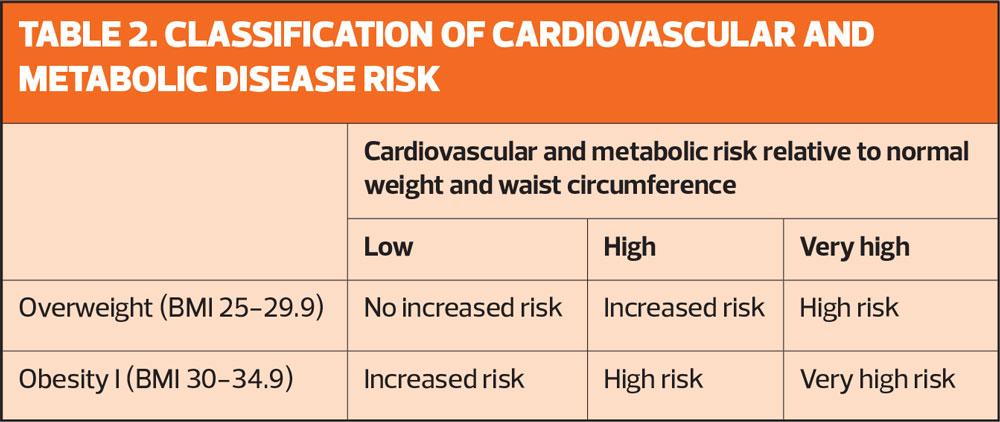
For men, waist circumference less than 94 cm (37 inches) is low, 94–102 cm (37–40 inches is high, and greater than 102 cm (approximately 40 inches) is very high.
For women, waist circumference less than 80 cm (31.5 inches) is low, 80–88 cm (31.5–34.5 inches) is high, and greater than 88 cm (approximately 34.5 inches) is very high.1,7
Arrange appropriate investigations, including blood glucose and lipid profile.
Use the person's BMI, waist circumference, and the information in Table 2 to assess whether the person is at increased risk.
Some population groups (for example Asian people and older people) have comorbidity risk factors that are of concern at different levels of BMI (lower for Asian people and higher for older people). People with BMI of 35 kg/m2 or more are at very high risk, regardless of waist circumference.
HOW SHOULD I MANAGE A PERSON WHO IS OVERWEIGHT OR OBESE?
The general principles of management include offering structured advice regarding physical activity and diet. You should be able to discuss the choice of interventions for weight management with the person, and you may want to consider the use of behavioural interventions.
Ensure weight management programmes include behaviour change strategies to increase people's physical activity levels or decrease inactivity, improve eating behaviour and the quality of the person's diet, and reduce energy intake.
Drug treatment and/or surgery may be required in some cases.
The components of the planned weight management programme should be tailored to the person's preferences, initial fitness, health status, and lifestyle.
- BMI of 25–29.9 kg/m2 (overweight) and low waist circumference (less than 80 cm for women or less than 94 cm for men): offer general advice on healthy weight and lifestyle.
- BMI of 25–29.9 kg/m2 and large waist circumference: offer structured advice regarding physical activity and diet. Consider the use of behavioural interventions.
- Consider the need for drug treatment in overweight people with a BMI of 27 kg/m2 with associated risk factors (such as type 2 diabetes, hypertension, or dyslipidaemia).
- Be aware that drug treatment for people with obesity or overweight should only be considered once dietary and physical activity interventions have been evaluated; and it should form part of an integrated approach to weight management, which should include advice and support on diet and physical activity, and behavioural strategies.
- Consider the need for referral to weight management services (tier 2 services) or specialist obesity services (tier 3 services).
The NICE guideline on Weight management: lifestyle services for overweight or obese adults covers multi-component lifestyle weight management programmes, and recommends:14
- For people with a BMI of 30–34.9 kg/m2 (obesity I):
- Offer structured advice regarding physical activity and diet. Consider the use of behavioural interventions.
- Consider the need for drug treatment in people with associated risk factors (such as type 2 diabetes, hypertension, or dyslipidaemia).
- Consider the need for referral for weight management services (tier 2 services) or specialist obesity services (tier 3 services).
- For people with recent-onset type 2 diabetes (diagnosed within a 10-year time frame) with a BMI of 30–34.9 kg/m2, consider an assessment for bariatric surgery as long as the person is also receiving specialist assessment.
If the person is of Asian family origin, consider referral for an assessment for bariatric surgery for people at a lower BMI than other populations if they are also receiving specialist assessment.
- For people with a BMI of 35 kg/m2 or more (obesity II and obesity III):
- Consider starting drug treatment.
- Consider the need for bariatric surgery.
Aim for an overall 5–10% reduction in body weight (or higher [for example more than 20%] in people with BMI of more than 35 kg/m2). Weekly weight loss should be no more than 1 kg.
Offer regular follow-up and maintain a record of the agreed goals and actions.
Diets for sustainable weight loss
- A 600 kcal/day deficit diet (that is, they contain 600 kcal less than the person needs to stay the same weight), or
- Reducing calories by lowering the fat content (low-fat diets).
- Low-calorie diets (800–1600 kcal/day) but be aware these are less likely to be nutritionally complete.
Do not routinely use very-low-calorie diets (800 kcal/day or less) to manage obesity, except in consultation with specialists who advise that these may be appropriate in patients who are in a diabetes treatment programme or other specialist settings.
WHAT DO I NEED TO KNOW ABOUT DRUG TREATMENT FOR PEOPLE WHO ARE OBESE?
Drug treatment should:
- Only be considered once dietary and physical activity interventions have been evaluated.
- Form part of an integrated approach to weight management, which should include advice, support, counselling on diet and physical activity, and behavioural strategies.
- Be offered with information, support, and counselling on additional diet, physical activity, and behavioural strategies when drug treatment is prescribed.
Practice nurses should also provide information on patient support programmes, monitor the effect of drug treatment, be aware of the pros and cons of drug treatment options, and reinforce lifestyle advice and adherence through regular review.
Orlistat
The drug orlistat is licensed for adults aged between 18–75 years who meet one of the following criteria: obese with a BMI of 30 kg/m2 or more, or overweight with a BMI of 28 kg/m2 or more with associated risk factors.
Orlistat is a tablet that can be purchased over the counter (as Alli) and does not need a prescription. It blocks the action of gastric and pancreatic lipid enzymes, preventing the digestion of triglycerides and absorption of fats. This can result in the common adverse effects of diarrhoea, bloating, flatulence, and abdominal pain which can cause people to stop taking the drug.
Orlistat should be taken with meals that contain ≤ 30% fat (if a meal is missed, or contains no fat the dose should not be taken). Reducing fat intake can help to reduce the incidence of adverse affects, including fatty smelly stools, oily spotting and urgency.
Liraglutide
The drug liraglutide (as Saxendra) can be prescribed in specialist tier 3 services for people who are not diabetic but have hyperglycaemia and a BMI of at least 35kg/m2 and have a high risk of cardiovascular disease.
Liraglutide is an injectable medication that should be administered subcutaneously. Its mode of action appears to be related to reducing hunger and lowering energy intake and it has an impact on stimulating insulin secretion. Again, the common adverse are gastrointestinal with nausea, diarrhoea and vomiting and constipation being reported commonly.
Both drugs need to be re-evaluated in terms of the weight loss that they are delivering for individuals over time, compared to the possible adverse effects that they cause.
NICE evaluated the use of liraglutide in December 2020 and concluded: ‘Many people decide not to have orlistat or stop taking it because of undesirable side effects. Most people referred to a tier 3 service will have tried and stopped orlistat, so there is a high clinical need for other pharmacological options. The clinical experts explained that liraglutide would only be considered if orlistat or bariatric surgery are not an option for the patient or they do not want to have these treatments. Only around 0.1% of people who are eligible for bariatric surgery have it. The committee concluded that orlistat and bariatric surgery would not be alternatives to liraglutide for most people, and that the appropriate comparator is lifestyle changes without medicines.’17
WHAT DO I NEED TO KNOW ABOUT BARIATRIC SURGERY?
Bariatric surgery is recommended as a treatment option if all the following criteria are fulfilled:
- The person has a BMI of 40 kg/m2 or more, or between 35 kg/m2 and 40 kg/m2 with other significant disease that could be improved if they lost weight, for example type 2 diabetes, hypertension, or severe mobility problems
- All appropriate non-surgical measures have been tried but the person has not achieved or maintained adequate weight loss
- The person has been receiving or will receive intensive management in a tier 3 service.
- The person is fit for anaesthesia and surgery
- The person commits to the need for long-term follow up.
In addition to the criteria listed above, bariatric surgery is the option of choice for adults with a BMI of more than 50 kg/m2 when other interventions have been ineffective.
Bariatric surgery is the most effective treatment for morbid obesity in terms of long-term weight loss, improvements of comorbidities and quality of life, and decreasing overall mortality.3,12,15,16
WHEN SHOULD I CONSIDER REFERRAL?
Consider referral for lifestyle weight management services (tier 2 services) for people with a BMI of 30 kg/m2 or more, although the threshold should be lower (27.5kg/m2 or more) for people of black African, African-Caribbean, and Asian family origin, as they are at increased risk of complications at a lower BMI.
Consider referral to a specialist obesity service (tier 3 services) if:
- The underlying causes of overweight and obesity need to be assessed
- The person has complex disease states or needs that cannot be managed adequately in tier 2 (for example, the additional support needs of people with learning disabilities)
- Conventional treatment has failed in primary or secondary care
- Drug treatment is being considered for a person with a BMI of more than 50 kg/m2
- Specialist interventions (such as a very-low-calorie diet) may be needed
- Surgery is being considered.
CONCLUSION
Practice nurses are acutely aware of the increasing burden of obesity in primary care. As you are regularly managing your population of patients with obesity and associated long-term conditions you are ideally placed to assess, advise, monitor, and support patients with their potential weight loss strategies. The professional interactions that practice nurses bring to these consultations is enormously important and potential benefits of weight loss for patients who are overweight are significant both for the individual's short-term and long-term health.
REFERENCES
1. NICE CG189. Obesity: identification, assessment, and management; 2014. https://www.nice.org.uk/guidance/cg189
2. National Heart Forum, Faculty of Public Health. Healthy weight, Healthy lives: a toolkit for developing local strategies. https://www.heartforum.org.uk/Publications_NHFreports_HealthyWeightHealthyLives.aspx
3. BMJ Best Practice. Obesity in adults. January 2020 https://bestpractice.bmj.com/topics/en-gb/211
4. Maffeis C. Aetiology of overweight and obesity in children and adolescents. European Journal of Pediatrics 2000;159(Suppl 1):S35-S44.
5. Farooqi IS. Obesity. In: Warrell DA, Cox TM, Firth JD. (Eds.) Oxford textbook of medicine. 5th edn. 2010; Oxford: Oxford University Press, 1527-1534.
6. Pinkney J. Obesity and disease: hormones and obesity. In: Kopelman PG, Caterson ID Dietz WH. (Eds.) Clinical obesity in adults and children. 2005; Oxford: Blackwell Publishing, 198-212.
7. Scottish Intercollegiate Guideline Network. SIGN 115. Management of obesity; 2010 https://www.sign.ac.uk/assets/sign115.pdf
8. Apovian CM, Aronne LJ, Bessesen DH, et al. Pharmacological management of obesity: an endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2015;100(2), 342-362.
9. McGowan BM. A Practical Guide to Engaging Individuals with Obesity. Obesity Facts 2016;9(3):182-192.
10. Organisation for Economic Co-operation and Development (OECD). Obesity Update 2017.. https://www.oecd.org/els/health-systems/Obesity-Update-2017.pdf
11. NICE NG7. Preventing excess weight gain; 2015. https://www.nice.org.uk/guidance/ng7
12. Yumuk V, Tsigos C, Fried M, et al. European Guidelines for Obesity Management in Adults. Obesity Facts 2015;8(6):402-424.
13. Public Health England. Let's talk about weight: A step-by-step guide to brief interventions for health and care professionals; 2017. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/649095/child_weight_management_lets_talk_about_weight.pdf
14. NICE QS111. Obesity in adults: prevention and lifestyle weight management programmes; 2016. https://www.nice.org.uk/guidance/qs111
15. Bray GA, Frühbeck G, Ryan DH, et al. Management of obesity. Lancet 2016;387(10031):1947-1956.
16. Erlandson M, Ivey LC, Seikel K. Update on Office-Based Strategies for the Management of Obesity. Am Fam Phys 2016;94(5), 361-368.
17. NICE TA664. Liraglutide for managing overweight and obesity Technology appraisal guidance; 2020 https://www.nice.org.uk/guidance/ta664/chapter/3-Committee-discussion
Related articles
View all Articles