NICE NG136. Hypertension in adults: diagnosis and management
NICE NG136, August 2019 (updated August 2109)
NICE NG136, August 2019
The 2023 update to NICE guidance on the management of hypertension aims to reduce the risk of cardiovascular problems such as heart attacks and strokes by helping healthcare professionals to diagnose hypertension accurately and treat it effectively
DIAGNOSING HYPERTENSION
Ambulatory blood pressure monitoring (ABPM) remains the gold standard for the accurate measurement of BP in primary care, and has therefore been retained as the preferred method for the diagnosis of hypertension, and should be used to confirm a diagnosis following clinic BP measurement.
When considering a diagnosis, measure BP in both arms:
- If the difference in readings between arms is more than 15 mmHg (updated from 20 mmHg), repeat the measurements, and if it is still more than 15 mmHg on the second reading, measure subsequent blood pressures in the arm with the higher reading.
This reflects recent evidence that even a small difference in arm blood pressure is associated with an increased risk of cardiovascular events, possibly due to vascular damage.
If clinic BP is ≥140/90 mmHg:
- Take a second measurement during the consultation
- If the second measurement is substantially different from the first, take a third
- Record the lower of the last 2 measurements as the ‘clinic BP’.
If clinic blood pressure is between 140/90 mmHg and 180/120 mmHg, offer ABPM to confirm the diagnosis
The recommendation to use ABPM has been in place since 2011 but implementation has been ‘challenging’ and there is still variation in practice. A change in practice and additional resources and training will be needed in areas where there is currently no access to ABPM. However, ABPM is considered the most cost-effective method of diagnosis, as avoiding over-diagnosis and unnecessary treatment will outweigh initial costs.
Postural hypotension
In people with symptoms of postural hypotension, including falls or postural dizziness:
- Measure BP with the person lying on their back (or seated if this is more convenient), then
- Measure BP again after the person has been standing for at least 1 minute.
If the person's systolic BP falls my 20 mmHg or more, or their diastolic BP falls by 10 mmHg or more, consider likely causes including reviewing current medication, offering advice on falls prevention, and consider referral to specialist care if symptoms persist despite addressing likely causes.
While waiting for confirmation of a diagnosis, carry out
- Investigations for target organ damage
- Formal assessment of cardiovascular risk – use the QRISK3 (or QRISK2 if QRISK3 is unavailable in your practice system) risk assessment tool
Confirm diagnosis of hypertension in people with:
- A clinic BP of ≥140/90 mmHg
- ABPM daytime average or HPBM average of ≥135/85 mmHg
ASSESSING CARDIOVASCULAR RISK AND TARGET ORGAN DAMAGE
Estimate cardiovascular risk using QRISK3. (If unavailable in your practice system, use QRISK2). Use clinic BP measurements to calculate risk.
For all people with hypertension, offer to:
- Test for the presence of protein in urine by sending a sample for estimation of albumin: creatinine ratio and test for haematuria using a reagent strip
- Take a blood sample to measure HbA1c, electrolytes, creatinine, estimated glomerular filtration rate, total cholesterol and HDL cholesterol
- Examine the fundi for the presence of hypertensive retinopathy
- Arrange for (or perform) a 12-lead ECG
TREATING AND MONITORING HYPERTENSION
In addition to usual advice on lifestyle (diet, exercise, smoking, reducing salt and caffeine consumption) ask about alcohol consumption and encourage reduced intake if they drink excessively because this can reduce BP and has broader benefits. See NICE guideline on alcohol-use disorders https://www.nice.org.uk/guidance/ph24/chapter/1-Recommendations#recommendations-for-practice
Offer antihypertensive drug treatment in addition to lifestyle advice to adults of any age with persistent stage 2 hypertension. Use clinical judgement for people of any age with frailty or multimorbidity
Discuss starting antihypertensive drug treatment in addition to lifestyle advice with adults aged under 80 with persistent stage 1 hypertension who have 1 or more of the following:
- Target organ damage
- Established cardiovascular disease
- Renal disease
- Diabetes
- An estimated 10-year risk of cardiovascular disease of 10% or more
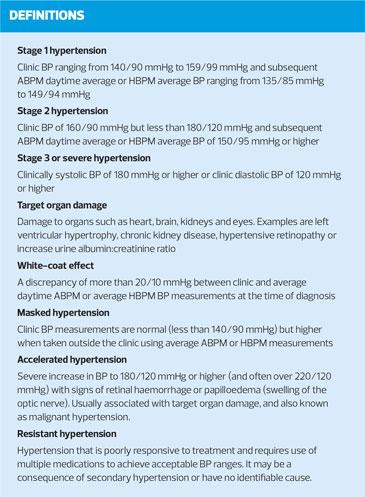
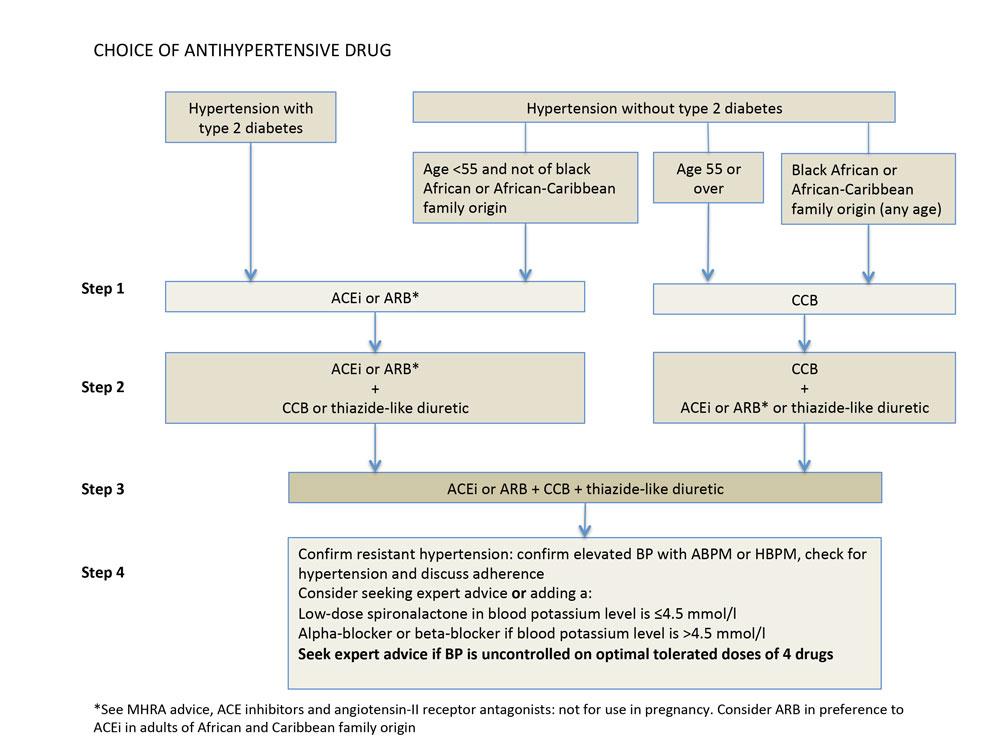
Discuss with the person their individual CVD risk and preferences for treatment, including no treatment. (Figure 1 – Choice of antihypertensive drugs)
Consider antihypertensive drug treatment in addition to lifestyle advice for adults under 60 years with stage 1 hypertension and an estimate 10-year risk below 10%. Remember 10-year cardiovascular risk may underestimate the lifetime probability of developing CVD.
Consider antihypertensive drug treatment in addition to lifestyle advice for people over 80 years with a clinic BP of over 150/90 mmHg. Use clinical judgement for people with frailty or multimorbidity.
For adults under 40 years with hypertension, consider seeking specialist evaluation of secondary causes of hypertension and a more detailed assessment of long term benefits and risks of treatment.
Monitoring
Use clinic blood pressure measurements to monitor the response to lifestyle changes or drug treatment. Measure standing as well as seated blood pressure in people with hypertension and:
- Type 2 diabetes
- Symptoms of postural hypotension, or who are
- Aged 80 and over
In people with significant postural drop or symptoms of postural hypotension, treat to a BP target based on standing blood pressure.
Advise people who choose to self-monitor their BP to use HBPM, and provide advice on their use and information on what to do if they are not achieving their target BP.
Provide an annual review for adults with hypertension to monitor BP, provide support, and discuss their lifestyle, symptoms and medication.
BP targets
In adults under 80 years, with or without type 2 diabetes, type 1 diabetes or chronic kidney disease, reduce and maintain clinic BP to below 140/90 mmHg (when using ABPM or HBPM, to below 135/85 mmHg)
In adults over 80 years, reduce and maintain clinic BP to below 150/90 mmHg (when using ABPM or HBPM, to below 145/85 mmHg). Use clinical judgement for people with frailty or multimorbidity.
The same targets should be used with and without cardiovascular disease.
The GDC considered evidence that showed benefits and harms associated with a lower clinic systolic BP target (120 mmHg) in people with hypertension without type 2 diabetes, but although the lower target was associated with reduced mortality and cardiovascular events, it was also associated with greater risk of harms, such as injury from falls and acute kidney injury.
The recommendations emphasise maintaining BP consistently below the BP target, which could lead to higher use of antihypertensive drugs and an increase in consultations. However, for people with type 2 diabetes and target organ damage, the slightly higher target BP, compared to that previously recommended, may reduce adverse events, lead to fewer consultations and reduced drug use.
In people with postural hypotensive, treat to a BP target based on standing BP.
Choosing antihypertensive drug treatment
Recommendations for drug treatment remain much the same as in previous editions of the guideline, (See Figure 1) with the exception of use of beta-blockers in certain groups of younger patients. The GDC agreed that beta-blockers are rarely used in current practice, and there is no established relationship between their use in primary hypertension and a reduction in cardiovascular events.
The recommendations replace the section on BP management in NICE’s guideline on type 2 diabetes.
Choice of initial treatment between ACE inhibitors and ARBs has been broadened as they are now cost- and clinically-equivalent.
Unlike more recent European guidelines, NICE does not recommend initial dual therapy, because the GDC considered there was insufficient evidence to determine the potential benefits or harms from this approach, but has recommended this as an area for further research.
There was no new evidence for step 2 or step 3 treatment for hypertension that would determine the best sequence for use of these drugs, therefore the recommendations remain unchanged. The recommendation to confirm resistant hypertension before initiating step 4 treatment aims to prevent overtreatment. The recommendation for using high-dose thiazide diuretics as step 4 therapy, although not commonly used, has been removed.
WHO TO REFER FOR SAME-DAY SPECIALIST REVIEW
Refer people for specialist assessment, to be carried out on the same day, if they have clinic BP of 180/120 mmHg and higher, with:
- Signs of retinal haemorrhage or papilloedema (accelerated hypertension) OR
- Life-threatening symptoms such as new onset confusion, chest pain, signs of heart failure, or acute injury
Refer for same-day specialist assessment if they have suspected phaeochromcytoma (e.g. labile or postural hypotension, headache, palpitations, pallor, abdominal pain or diaphoresis)
NICE NG136. Hypertension in adults: diagnosis and management; August 2019, updated November 2023.
Related guidelines
View all Guidelines