Guidelines in a nutshell: Long COVID
Practice Nurse 2021;51(9):11-13
Practice Nurse 2021;51(9):11-13
Nurek M, Rayner C,Freyer A, et al. Recommendations for the recognition, diagnosis, and management of long COVID: a Delphi study. Br J Gen Pract 2021 Oct 28;71(712):e815-825
With an estimated 10% of the UK population living with ‘long COVID’ and an absence of research into therapies and care pathways, guidance based on emerging experience has been developed by a panel of experts across a number of specialties.
Long COVID, otherwise known as ‘post COVID-19 condition’, is an umbrella term for a complex, multisystem illness that follows on from an acute COVID-19 infection, irrespective of severity, immediately or some time after apparent recovery.
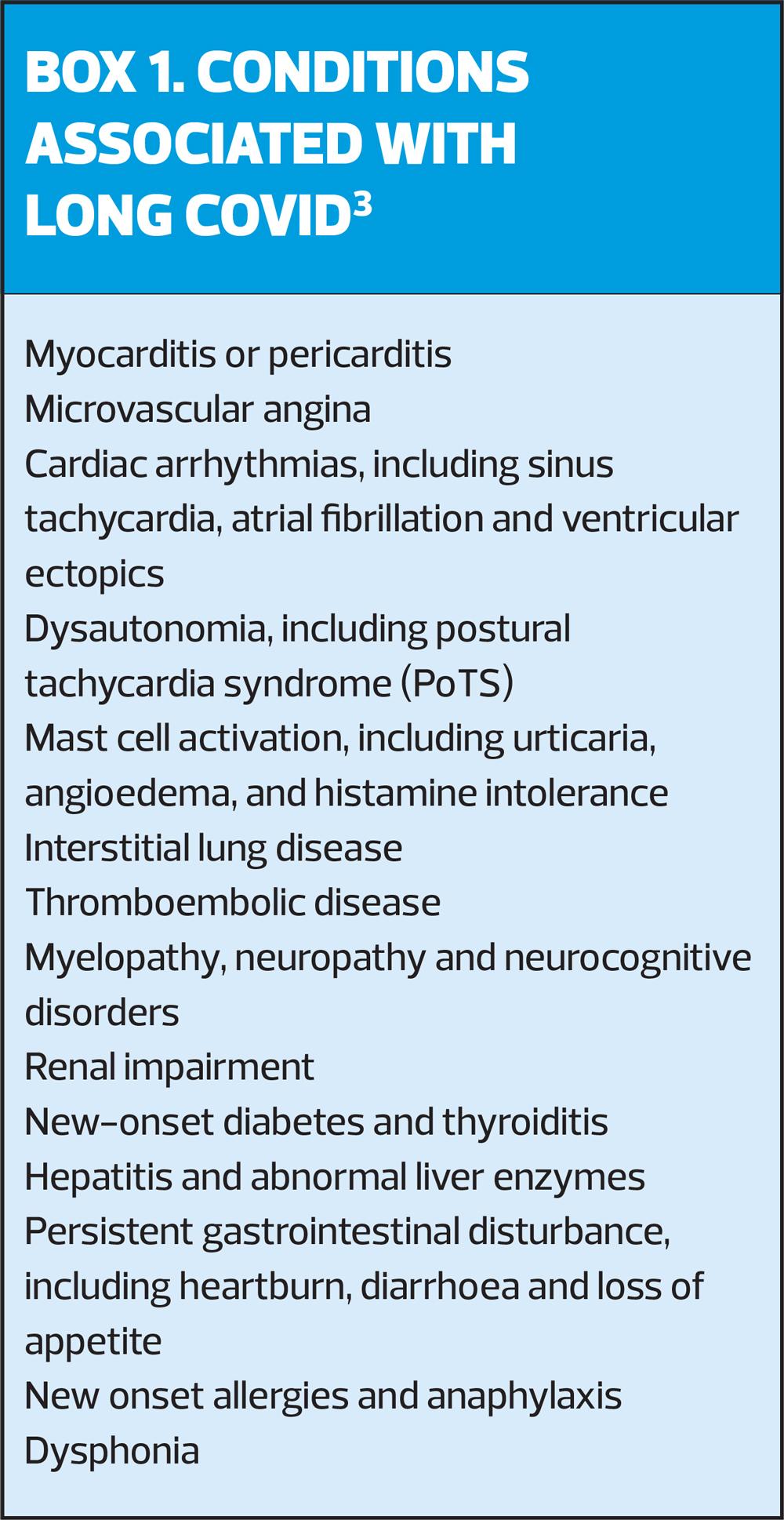
It is estimated that long COVID affects over 1 million people in the UK.1 The illness commonly has an unpredictable, relapsing-remitting pattern, with significant associated conditions appearing weeks to months into the disease course. These may include cardiac conditions and arrhythmias, interstitial lung disease, renal impairment, and new onset diabetes or thyroiditis (Box 1).2
A high index of suspicion and a low threshold for referral to secondary care specialists or clinics with diagnostic capabilities is therefore recommended in new guidance, published last month (October 2021) in the British Journal of General Practice.
Although NICE produced a ‘rapid guideline’ in December 2020,3 members of an online community of doctors with long COVID, identified a gap between best clinical practice and the ‘cautious, evidence-based approach’ adopted by NICE – which in turn was limited by the limited availability of evidence for the investigation and treatment of this new condition.
A pool of 33 experts, many of whom had long COVID themselves, set about capturing the knowledge gained through personal experience and developing consensus recommendations to guide generalists, including those working in community-based long COVID clinics.
RECOMMENDATIONS
In all, the panel reached consensus on 35 recommendations, most of which related to diagnosis and management.
Long COVID should be considered in patients with a clinical diagnosis of COVID-19 or positive test history, who present with new or fluctuating symptoms occurring beyond 4 weeks of the initial infection, including but not limited to:
- Breathlessness
- Chest pain
- Palpitations
- Inappropriate tachycardia
- Wheeze
- Stridor
- Urticaria
- Abdominal pain
- Diarrhoea
- Arthralgia
- Neuralgia
- Dysphonia
- Fatigue
- Cognitive impairment
- Prolonged pyrexia
- Neuropathy
It cannot therefore be assumed that patients are suffering from a self-limiting post-viral fatigue and that rehabilitation is sufficient. Patients require a holistic clinical approach that prioritises investigation of potential physical pathology.
In people with long COVID, non-COVID-19 related issues should be referred and investigated: the diagnosis of long COVID cannot be confirmed unless other causes have been excluded.
There is a considerable risk to patient safety if appropriate investigation of common symptoms of long COVID (such as chest pain, breathlessness, palpitations, abdominal pain, fatigue) that have wide differential diagnoses is not undertaken. Serious conditions, related to severe acute respiratory distress syndrome coronavirus 2 (SARS-CoV-2) infection or not, must be adequately excluded.
Assessment should be carried out (face-to-face) and include a thorough history and examination. A full panel of blood tests should include full blood count, renal function, C-reactive protein, liver function, thyroid function, HbA1c, vitamin D, magnesium (if available), B12, folate and ferritin. Bone studies should also be considered.
Respiratory symptoms
In people with respiratory symptoms, consider a chest X-ray early on, although a normal appearance does not exclude respiratory disease. Spirometry may also be normal, but patients may have diffusion defects, indicative of scarring, pulmonary emboli or microthrombi. Referral to a respiratory specialist for full lung function tests may be warranted.
The guidance also uses the term ‘breathing pattern disorder’ to describe the experience of patients that is not strictly ‘breathlessness’. These patients may benefit from specialist physiotherapy, available through long COVID clinics, although may turn to alternative therapy such as pranayama breathing. The NHS also promotes meditation or mindfulness as an effective therapy for anxiety and the sensation of breathlessness.
Consider cardiac causes of breathlessness. Normal D-dimer results may not exclude thromboembolism, and referral for investigation is indicated if there is a clinical suspicion of pulmonary embolism.
Cardiovascular complications
There is increasing evidence of cardiovascular complications with COVID-19. Patients with long COVID (of all ages) have been diagnosed with arrhythmias, autonomic dysfunction, myocarditis, pericarditis, and microvascular ischaemia.
Patients with tachycardia and/or chest pain should also be referred – they may need an MRI to rule out myopericarditis and microvascular angina, even if an echocardiogram is normal. Patients with cardiac symptoms should be advised to limit their heart rate to 60% of maximum (usually around 100–110 beats per minute) and investigated with at least electrocardiogram and echocardiogram before taking up exercise.
Autonomic dysfunction
Autonomic dysfunction, especially manifesting as postural orthostatic tachycardia syndrome (PoTS), occurs commonly post COVID-19. There is a need to consider a differential for tachycardia and palpitations that, in long COVID, includes pulmonary embolus, cardiac, and respiratory causes. The expert panel noted that autonomic dysfunction should also be suspected in patients with light-headedness, chest pain, and nausea, and the association of autonomic dysfunction with mast cell disorders should be considered.
A reasonable first line approach to autonomic dysfunction would be to consider increasing fluids, electrolytes, the use of compression hosiery, and specific rehabilitation. If PoTS is confirmed, and the patient does not respond, or has an inadequate response to non-pharmacological therapy, it would be appropriate to consider prescribing a beta-blocker, ivabradine, or fludrocortisone (with blood pressure and response monitoring).
Mast cell disorder
In patients with urticaria, conjunctivitis, wheeze, shortness of breath, abdominal cramps or bloating, sleep disturbance or neurocognitive fatigue, consider mast cell disorder. In patients with possible mast cell disorder, consider a 1-month trial of initial medical treatment and dietary advice. Higher than standard dose of antihistamines (two- to four-times higher) are commonly used for this indication. If this has a partial effect, consider adding second-level treatment such as montelukast, as well as referral to an allergy or immunology specialist. Be aware that adverse drug reactions are more common in patients with mast cell disorder, for example, to beta-lactam antibiotics, non-steroidal anti-inflammatory drugs (NSAIDs), codeine, morphine, or buprenorphine.
Cognitive effects
If patients experience cognitive difficulties sufficient to interfere with work or social functioning, neurocognitive assessment may be needed. In patients expressing distress, significant low mood, anxiety, or symptoms of post-traumatic stress disorder, consider referring for a mental health assessment.
Joint pain and swelling
Joint swelling and arthralgia may indicate new connective tissue disease or reactive arthritis, and patients with these symptoms should also be referred appropriately. Clinicians should include long COVID in a differential diagnosis once other known autoimmune causes have been excluded.
PRACTICAL SUPPORT
Many patients experience post-exertional symptom relapse. Physical or cognitive activity beyond the patient’s ‘energy envelope’ may exacerbate symptoms such as fatigue, fever, myalgia and breathlessness. Sometimes these exacerbations occur immediately, but in other cases, a day or two later – and they may last for weeks.
For patients with fatigue or worsening symptoms following an activity, emphasise the need for an initial phase of convalescence, followed by careful pacing and rest. Direct patients to appropriate resources to help with the management of post-exertional symptom exacerbation, activity pacing and diagnosis-specific management.
You may need to help patients adjust their mental timeline for recovery to reflect the likely prolonged course of long COVID, and a return to work may need to phased, possibly over a long period. Patients may need signposting to social prescribing, help with sickness certification and financial advice.
Prolonged illness following COVID-19 infection is characterised by different symptoms at different times. Although NICE states that new symptoms after 3 months are unlikely to be because of COVID, this is not borne out by research or experience. Clinicians need to provide patient safety-netting advice and guidance on expected patterns of illness, and patients should also be encouraged to report new symptoms, and to expect a waxing-wane course for current symptoms.
Vitamin and mineral supplementation
Patients with long COVID often self medicate with vitamin and mineral supplements – a practice known as ‘taking the stack’ – including high dose vitamin C and D, niacin (nicotinic acid), quercitin, zinc, selenium and magnesium. It is not known how helpful or otherwise supplementation may be, but supplements are associated with a range of drug interactions:
- Niacin + selective serotonin reuptake inhibitors (SSRIs) or NSAIDs increases the risk of bleeding events.
- Niacin + statins increases the risk of rhabdomyolosis
- Quercetin both inhibits and induces various cytochrome P450 enzymes, and may cause unwanted effects with, for example, quinolone antibiotics, warfarin, antihypertensive agents, medications for diabetes, NSAIDs and statins.
Research
The panel agreed that research was important and this should include quantifying the burden of disease. From a public health perspective, counting days lost to sickness and lost income due to long COVID is essential. It is therefore important that ‘fit notes’ should include a medically recognised diagnosis – NICE recommends ‘ongoing symptomatic COVID-19’ for symptoms lasting 4-12 weeks, and ‘Post COVID-19 syndrome’ for 12+ weeks. For NHS staff to receive ‘COVID pay’ during absence, the fit note must state ‘COVID’.
You may want to contribute patient data to research on long COVID, using the WHO Case Report Form4 – although the consensus group warns that it is a lengthy form. Patients should also be made aware of research studies – taking part could ‘add meaning to what is often a very negative experience’.
CONCLUSION
Long COVID is a new condition that has an impact on many aspects of life. It needs to be managed holistically, to address the physical, psychological and social aspects of the condition.
As well as ensuring that patients are appropriately referred, general practice nurses need to be able to give practical advice to patients, especially given the simple nature of many treatments – for example, compression stocking, fluids and electrolytes for PoTS; over the counter antihistamines for mast cell disorders, and respiratory physiotherapy for breathing pattern disorder.
They also need to be aware of the waxing and waning nature of symptoms, which may take a considerable time to resolve completely, and be prepared to provide patients with advice about the importance of pacing, to support them through the complexity of specialist investigations, and signpost patients to social prescribing, sickness certification and financial advice.
REFERENCES
1. Office for National Statistics. Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK: 1 April 2021 https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/1april2021
2. Gorna R, MacDermott N, Rayner C, et al. Long COVID guidelines need to reflect lived experience. Lancet 2021;397(10273):455–457.
3. NICE NG188. COVID-19 rapid guideline: managing the long-term effects of COVID-19; 2020 https://www.nice.org.uk/guidance/ng188
4. World Health Organization. Global COVID-19 clinical platform Case Report Form (CRF) for Post COVID condition (Post COVID-19 CRF); 2021 https://www.who.int/publications/i/item/global-covid-19-clinical-platform-casereport-form-(crf)-for-post-covid-conditions-(post-covid-19-crf-)
Related guidelines
View all Guidelines