Chronic wounds
Dr Philip Marazzi
Dr Philip Marazzi
GP, East Horsley, Surrey
Chronic wounds are frequently seen in general practice. Many start with a seemingly insignificant injury but the patient’s underlying medical condition can result in delayed healing. It is estimated that around 4.5% of the adult population will have a wound in any year, of these 12% have no diagnosis, and around 40% of wounds will not have healed within a year. The treatment of chronic wounds involves appropriate dressing selection – but also, and importantly, optimising management of the underlying disease process. Dressing selection should be made after careful clinical assessment of the wound itself, its stage of healing and the patient’s clinical condition.
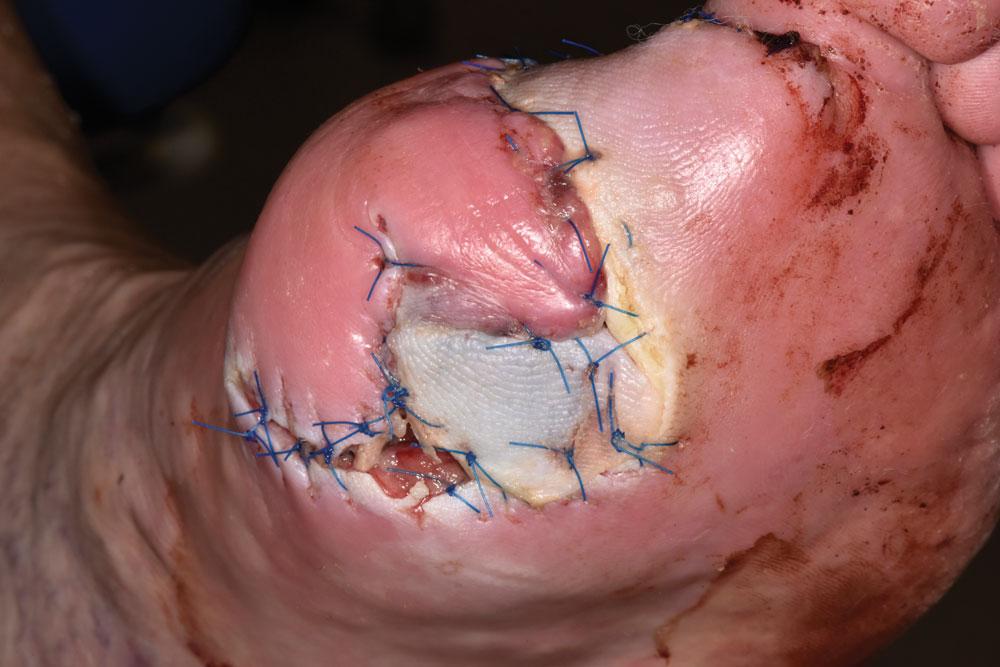
1. PERIPHERAL VASCULAR DISEASE
This 81-year-old man developed an infection around the end of his big toe. He had a significant history of peripheral vascular disease and smoking over 20 cigarettes a day for 60 years. He had no palpable peripheral pulses. The infection started as a very minor issue but in spite of the efforts of the district nurses got progressively worse over several weeks. The wound was swabbed and this showed a combination of MRSA and proteus mirabilis. His condition deteriorated and he underwent amputation of the toe. Problems continued and he had to go back to theatre for further debridement. The wounds finally healed. He continues to smoke!
2. DIABETES MELLITUS
This image shows the knees of a 35-year-old female patient with type 1 diabetes. She had gone through many years of rebellious behaviour associated with poor diabetic control in the past. This had led to renal failure, peripheral vascular disease and quite severe neuropathy. She fell over in her home and could not get up. She dragged herself across the room producing these carpet burns on her knees. The relatively mild grazes got progressively worse over the following two weeks. They were not painful, and she did not seek immediate help. When she finally presented she was immediately admitted to hospital where she was found to be very ill. She was an inpatient for five months before everything settled. Sadly, she died a year later from renal failure.
3. ALLERGY
This 13-year-old girl developed an abscess in her lumbar area. The wound burst and drained spontaneously, and her mother brought her in for wound dressing. The wound was healing well, but there was a problem with a clear allergic reaction to the adhesive used on the dressing. In this particular case, the dressing was Clearpore® although many different dressings may cause problems to different patients. This girl was quite an ‘atopic’ individual and it proved quite difficult to find a dressing that her skin would tolerate. Eventually Biatain® proved to be the answer for her.
4. FLAP LACERATION
One of the commonest type of injury seen in practice nurses rooms are superficial flap lacerations. These commonly occur in elderly patients such as this 85-year-old. She had caught her ankle on the corner of a dishwasher door that had been left open. The injury itself is clearly unpleasant, but is always made worse by factors that increase the fragility of the skin, the most obvious being age with its associated loss of elasticity, strength and subcutaneous tissue. Sometimes factors such as steroid use, varicose veins and poor circulation will aggravate skin fragility. As a result of a combination of luck and good patient adherence to instructions, the wound healed reasonably well.
5. VENOUS ULCER
Another extremely common problem in the treatment room, and a huge consumer of nursing time is the venous or varicose ulcer. These lesions occur in patients with incompetent or varicose veins who generally sustain a very minor injury. Instead of healing within a few days, the skin starts to break down and an ulcer forms. Once this happens, the situation tends to get progressively worse, with increasing oedema, oozing from the open wound, and itching and pain. The wounds often become infected as they are open lesions, and there is invariably considerable pressure to treat the infection with antibiotics. This is rarely helpful however, as long courses may be required, with risks of resistance. The wound will subsequently become ‘infected’ again as soon as antibiotics are stopped. The mainstay of treatment is appropriate dressing with or without compression, along with elevation. Venous ulcers may take many months to heal.
6. KELOID
Most trauma and surgical wounds heal extremely well. Some, however, develop problems like this. Here a 22-year-old man has had a major operation to clear lymph nodes from his neck after he was diagnosed with a malignant melanoma on his head. This was excised and the neck dissection undertaken to assess if there was metastatic spread, and hopefully remove it if present. Keloid scarring is difficult to predict, but it is more likely to affect certain patient types such as younger patients with dark skin and sometimes a possible family history. Certain areas of the body such as the head and neck are also more prone to keloid formation. There are various options available to treat these hypertrophic scars including the use of silicon gel based dressing, intralesional steroid injections and steroid dressings, and even further surgery, though the removal of a keloid scar may lead to the formation of a new one. Radiotherapy has also been used. Eventually, many keloid scars will fade and shrink, but this may take several years.
Related articles
View all Articles