Urinary tract infections: assessment and management
DR GERRY MORROW
DR GERRY MORROW
MB ChB, MRCGP, Dip CBT
Medical Director and Editor,
Clarity Informatics Limited
UTIs are one of the most common reasons for women to present in general practice, and for many women – and some men – they are a recurrent misery. Practice nurses are ideally placed to assess possible UTIs and this guide explains what to look out for and how to treat them
Urinary tract infections (UTI) are one of the most common acute reasons for women to present in general practice, and for many women they are a recurrent misery.1 Most people who consult a healthcare professional about a UTI will be prescribed an antibiotic, although of those who have a urine sample sent for culture, only 24-66% have a confirmed bacterial infection.2,3
A UTI is an infection of any part of the urinary tract, usually by bacteria, but more rarely by other micro-organisms such as fungi, viruses, or parasites.
Definitions
- Lower UTI is an infection of the bladder.
- Cystitis is often used as a synonym for lower UTI (particularly for women), although technically it means 'inflammation of the bladder' and there may be rare, non-infectious causes such as radiation and chemical-induced cystitis.
- Upper UTI includes pyelitis (infection of the proximal part of the ureters) and pyelonephritis (infection of the kidneys and the proximal part of the ureters).
- Uncomplicated UTI is infection of the urinary tract by a usual pathogen in a person with a normal urinary tract and normal kidney function.
- Complicated UTI is when one or more risk factors present that predispose the person to persistent infection, recurrent infection, or treatment failure.
- Recurrent UTI is repeated UTI, which may be due to relapse or reinfection, and may be defined as 3 or more UTIs in the last 12 months, or 2 or more episodes of confirmed UTI in the last 6 months.
- Relapse is defined as a recurrent UTI with the same strain of micro-organism. Relapse is the likely cause if infection recurs within a short period after treatment (for example within 2 weeks).
- Reinfection is a recurrent UTI with a different strain or species of micro-organism. Reinfection is the likely cause if UTI recurs more than 2 weeks after treatment.
- Asymptomatic bacteriuria is the presence of significant bacteria in the urine, as a result of colonisation of the urinary tract, without symptoms or signs of infection.4
CAUSES OF UTI
UTI is usually caused by bacteria from the gastrointestinal tract. The spectrum of micro-organisms which cause UTI is similar in men and women. The most common causative micro-organisms are Escherichia coli (80%), Staphylococcus saprophyticus (4%), Klebsiella pneumoniae (4%) and Proteus mirabilis (4%).5,6
UTI results from one of these pathogenic organisms gaining access to the urinary tract and not being effectively eliminated. Entry of bacteria into the urinary tract can be direct, for example, from insertion of a catheter into the bladder, or instrumentation; via the blood stream (more likely in immunocompromised people); or retrograde, ascending through the urethra into the bladder.
UTI is much less common in men than in women, a fact that is attributed to a shorter urethra in women.7
The incidence of UTI increases substantially with, increasing age, co-existing illness, institutional care, and the presence of an indwelling urinary catheter.
UTI is the most common hospital-acquired infection in the UK, accounting for 23% of all infections. The majority of hospital-acquired UTIs are associated with catheter use, and catheter-associated UTIs are the source of 8% of hospital-acquired bacteraemia.8
COMPLICATIONS
Complications of UTIs include renal function impairment – the risk factors for developing renal damage include prostatitis in men, obstruction, the presence of stones, and the presence of indwelling catheters.
At least 50% of men with recurrent UTI and over 90% of men with UTI associated with fever have prostate involvement, which may lead to complications such as prostatic abscess or chronic bacterial prostatitis.
An estimated 75% of people with pyelonephritis will have had a previous UTI.
Sepsis is a less common complication of UTI. Bacteraemia occurs infrequently with UTI, but instrumentation of the urinary tract or the presence of indwelling urinary catheters increases the risk.
Urinary stones are more likely to occur with Proteus mirabilis infection which is associated with stone formation in the renal collecting ducts.
In pregnant women, UTI is associated with pre-term delivery and low-birthweight.
DIAGNOSIS
You should suspect UTI in anyone presenting with the following typical features:
- Dysuria – discomfort, pain, burning, tingling or stinging associated with urination
- Frequency – passing urine more often than usual
- Urgency – a strong desire to empty the bladder, which may lead to urinary incontinence
- Changes in urine appearance or consistency, colour or odour or frank haematuria
- Nocturia — passing urine more often than usual at night
- Suprapubic discomfort and/or tenderness.9,10
It is important to note that these typical features may be absent, in particular in elderly people with underlying cognitive impairment. Consider UTI if the person presents with generalised non-specific clinical features such as delirium, lethargy, reduced ability to carry out activities of daily living or poor appetite.
In these situations it is clear that we should also consider alternative sources of infection and causes of delirium other than UTI, such as chest infections, which must be excluded before a working diagnosis of UTI is made.9,10
Pyelonephritis should be suspected in people with fever, loin pain or rigors.9,10
Making an assessment
Practice nurses are ideally placed to make an assessment of possible UTI. This assessment should involve a full clinical assessment, history and examination. The important features of this assessment are as follows:
- Symptoms such as vaginal or urethral discharge, irritation or skin rash which may indicate a cause other than UTI.
- Red flags such as haematuria, loin pain, rigors, nausea, vomiting, and altered mental state — consider the possibility of serious illness such as sepsis.
- Family history of urinary tract disease such as polycystic kidney disease.
- Possibly of pregnancy in women of childbearing age — carry out a pregnancy test if unsure.
- Past medical history including risk factors for recurrent UTI such as neurological conditions, diabetes mellitus, immunosuppression, urolithiasis, and bladder catheterisation.
- Medication, including recent antibiotics.
Examination
Check vital signs (temperature, blood pressure, heart rate and respiratory rate), looking for signs of systemic illness or sepsis.
Palpate for flank or suprapubic tenderness and pelvic or abdominal masses.
Consider other diagnoses (for example pyelonephritis, obstruction or malignancy) if the person has significant abdominal pain, flank tenderness or a pelvic or abdominal mass.
Check for blockage if there is a urinary catheter in situ.
Assess other systems depending on suspected cause, for example, genital examination if vulvovaginal atrophy or herpes simplex is a possibility.
Check for all new signs and symptoms of UTI — new onset dysuria alone, or two or more of:
- Temperature 1.5°C above normal twice in the last 12 hours
- New frequency or urgency
- New incontinence
- New or worsening delirium/debility
- New suprapubic pain
- Visible haematuria.
Check for two or more localised signs and symptoms of other infection (respiratory tract, gastrointestinal tract, skin and soft tissue).
Investigations in women with possible UTI
If the woman is under 65 years of age, and does not have risk factors for complicated UTI, urine dipstick can be used as an aid to diagnosis. Dipstick is an unreliable method of assessment in women aged older than 65 years and those who are catheterised.10
There are three possible results of dipstick testing
1. If dipstick is positive for nitrite or leukocytes and red blood cells (RBC) then a UTI is likely.
In this case, a urine sample (morning sample most reliable) for culture and sensitivities should be sent if previous antibiotic treatment has failed or there is a possibility of antibiotic resistance. Sample containers with boric acid preservative should be filled to the marked line.
2. If urine dipstick is negative for nitrite and positive for leukocyte, UTI is equally likely to other diagnosis. In this case you should send urine for culture to confirm the diagnosis.
3. If urine dipstick is negative for all nitrite, leukocyte and RBC, UTI is less likely. In this case there is no need to send sample for urine culture, instead you should consider other diagnoses.
A sample should be sent for urine culture in all women with suspected lower UTI who:
- Are pregnant
- Are older than 65 years
- Have symptoms that are persistent or do not resolve with antibiotic treatment
- Have recurrent UTI (two episodes in 6 months or three in 12 months)
- Have a urinary catheter in situ or have recently been catheterised
- If the catheter has been changed the sample should be collected from the newly placed catheter – using aseptic technique drain a few millilitres of residual urine from the tubing, then collect a fresh sample from catheter sampling port
- Ensure the microbiology request form states that this is a suspected catheter-associated infection and details of any antibiotic prescribed
- Have risk factors for resistance or complicated UTI such as abnormalities of genitourinary tract, renal impairment, residence in a long-term care facility, hospitalisation for more than 7 days in the last 6 months, recent travel to a country with increased resistance or previous resistant UTI
- Have atypical symptoms
- Have visible or non-visible (on urine dipstick) haematuria.10
Investigations in men with possible UTI
In men with symptoms suggestive of a UTI, confirm the diagnosis by urine culture and sensitivity, by arranging collection of a mid-steam urine (MSU) or catheter specimen of urine (CSU), to determine the infecting micro-organism. Obtain a urine sample for culture before starting empirical drug treatment. Only send a urine sample for culture in a man with an indwelling catheter if there are features of systemic infection.10
Do not use urine dipstick tests or microscopy to diagnose UTI in men:
- Who are not catheterised. In this case dipsticks are poor at ruling out infection. However, they may be helpful in some clinical situations to decide if a working diagnosis of UTI should be made.
If the dipstick test is negative for nitrites and leukocyte esterase, UTI is less likely, especially if symptoms are mild. However, the presence of these markers does not rule in UTI, although positive nitrite makes UTI more likely.10
- With an indwelling catheter. In this case, make a working diagnosis based on your clinical judgement.
- Aged over 65 years. As with women, dipsticks become more unreliable with increasing age over 65 years.
MANAGEMENT OF PEOPLE WITH UTI
There are a range of management options depending on the person’s clinical presentation, gender, presence or absence of urinary catheter and their previous history.
Women with an uncomplicated UTI (no catheter, no haematuria, not pregnant)
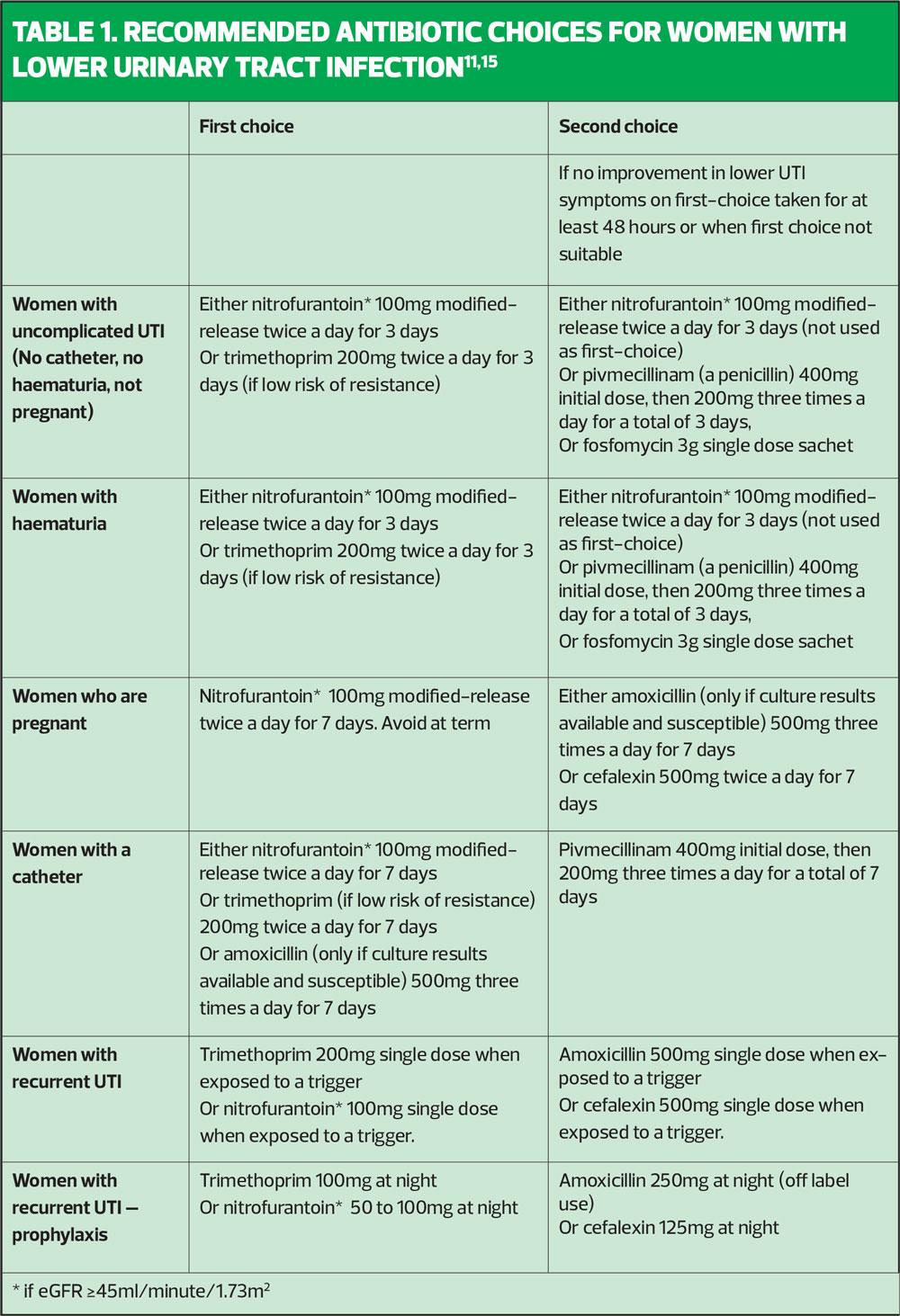
Consider the need for antibiotics depending on severity of symptoms, risk of complications, and previous urine culture results and antibiotic use. Recommended antibiotic choices are shown in Table 1.11
If prescribing an immediate antibiotic, then you should treat according to sensitivities from recent urine culture (if available), otherwise treat empirically taking account of local antimicrobial resistance patterns.11
Women with haematuria
Once more you should manage the acute UTI depending on specific clinical situation (ensuring that a urine culture has been sent prior to starting antibiotics). Consider prescribing an antibiotic as outlined above. Re-test urine after completing treatment with an appropriate antibiotic, if haematuria is persistent consider possible underlying causes.11
If a urological or gynaecological cancer is suspected, arrange an urgent 2-week wait referral.
If chronic kidney disease is suspected, arrange further investigations and consider the need for referral to secondary care.
If the underlying cause is unclear, discuss the need for further investigations/referral with urology.
UTI in pregnancy
Arrange urgent assessment in secondary care if there are any features of serious or systemic illness such as sepsis or pyelonephritis. Seek urgent specialist advice on further management of pregnant women:
- With recurrent lower UTI
- With catheter associated UTI
- If culture reveals an atypical bacterium
- With an underlying structural or functional abnormality or co-morbidity which increases the risk of complications or treatment failure
- With suspected underlying malignancy or renal disease
For an uncomplicated first lower UTI in a pregnant woman, you should give advice on self-care measures, including simple analgesia such as paracetamol for pain relief, and encourage intake of enough fluids to avoid dehydration. Send a midstream urine sample for culture and sensitivities before antibiotics are taken.11
Offer an immediate antibiotic prescription (Table 1) taking account of previous urine culture and susceptibility results, previous antibiotic use (which may have led to resistant bacteria) and local resistance patterns.
Advise the woman to seek urgent review if symptoms worsen at any time or fail to improve within 48 hours of starting antibiotics. Consider the possibility of alternative or serious diagnoses such as pyelonephritis or sepsis. Arrange follow up, which should include a review of choice of antibiotic when culture results are available. Change the antibiotic according to susceptibility results if bacteria are resistant.11
You should also send urine for culture once treatment is completed to ensure clearance of infection.11
Women with a catheter
Arrange urgent assessment in secondary care if there are any features of serious or systemic illness such as sepsis, pyelonephritis or if the woman is dehydrated or unable to tolerate oral fluids and drugs.12
Refer or seek specialist advice if the woman:
- Has a higher risk of developing complications (for example has structural or functional abnormalities or a comorbid condition such as immunosuppression)
- Has recurrent catheter associated-UTI (CAUTI)
- Has an infection caused by atypical or resistant bacterium.12
Advise the woman on self-care measures, such as simple analgesia and encourage intake of enough fluids to avoid dehydration. Do not recommend cranberry products or urine alkalinising agents in the treatment of lower UTI as these are not of proven benefit.12
If the catheter has been in place for more than 7 days, check for blockage and consider removing the catheter or, if this cannot be done, change it as soon as possible. Offer antibiotics, but before the first dose is taken, send a sample from mid-stream urine if the catheter has been removed or from the new catheter if changed — ensure the laboratory are aware of previous antibiotic use and that this is a suspected CAUTI.12
Advise all women to seek urgent medical review if their symptoms worsen rapidly or significantly at any time, or fail to improve within 48 hours of starting antibiotics. Consider the possibility of alternative or serious diagnoses such as pyelonephritis or sepsis. Send a urine sample for culture and susceptibility testing (if this has not already been done) and consider treatment with another agent (as described above) while awaiting sensitivities.12
Follow up urine culture and susceptibility results to review the choice of antibiotic when results are available. Change the antibiotic according to susceptibility results if bacteria are resistant, using narrow-spectrum antibiotics if possible. Do not routinely treat catheter-associated asymptomatic bacteriuria.12
Women with recurrent UTI
First, discuss potential issues that could be causing recurrence, which include behavioural and personal hygiene measures, and advise the woman to:
- Avoid douching and occlusive underwear.
- Wipe from front to back after defaecation.
- Avoid delay of habitual and post-coital urination.
- Maintain adequate hydration.13
Consider antibiotic prophylaxis if the underlying cause has been investigated and behavioural and personal hygiene measures (and vaginal oestrogen in postmenopausal women) are ineffective or inappropriate. Take account of severity and frequency of symptoms, risk of complications, previous urine culture and susceptibility results, previous antibiotic use and the woman’s preference.
Discuss the risks of long-term antibiotics including resistance and possible adverse effects.
If there is no improvement after single-dose antibiotic prophylaxis or there are no identifiable triggers, ensure that any current UTI has been adequately treated then consider a trial of daily antibiotic prophylaxis (Table 1).13
Arrange follow-up within 3–6 months and advise the woman to seek urgent review if symptoms of acute UTI develop — different antibiotics should be used for prophylaxis and treatment of acute UTI. At follow-up, check effectiveness of prophylaxis, discuss discontinuation or changing to an alternative and reinforce behavioural and personal hygiene measures.13
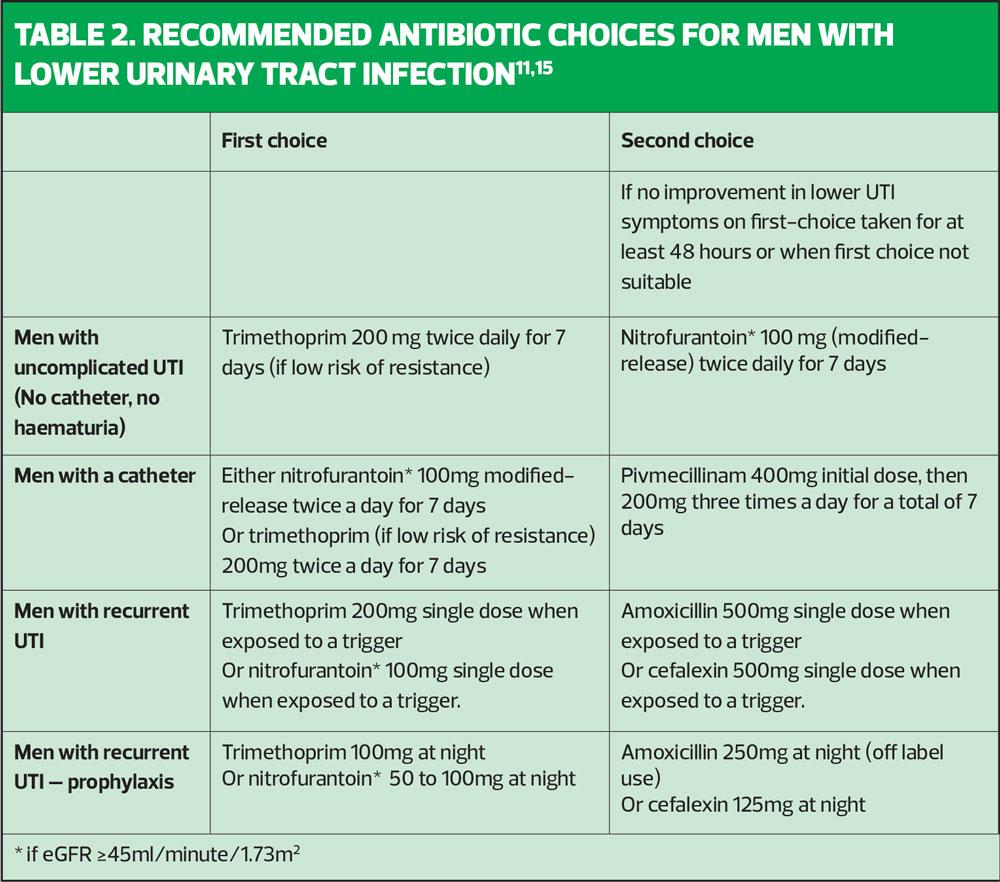
MEN WITH UNCOMPLICATED UTI
Arrange emergency admission to hospital if the man is severely unwell with symptoms or signs suggestive of urosepsis (for example, nausea and vomiting, confusion, tachypnoea, tachycardia, or hypotension). If hospital admission is not needed, offer an antibiotic, taking into account previous urine culture and susceptibility results and any previous antibiotic use, which may have led to resistant bacteria.11,14
Start empirical antibiotic drug treatment with trimethoprim or nitrofurantoin (if eGFR ≥ 45ml/minute/1.73m2), taking into account local antimicrobial resistance data (Table 2).11
Arrange follow up, for example after 48 hours, depending on clinical judgement, to check the man's response to treatment and the urine culture results. Change the antibiotic according to susceptibility results. If the bacteria are resistant and symptoms are not already improving, use a narrow-spectrum antibiotic wherever possible.11
Reassess if symptoms worsen rapidly or significantly at any time, or do not start to improve within 48 hours of starting antibiotic treatment, and consider other possible diagnoses including any symptoms or signs suggesting a more serious illness or condition, such as pyelonephritis.11,14
Men with a catheter
Check that the catheter is correctly positioned, drains correctly and is not blocked. Consider removing it, or, if this cannot be done, changing the catheter as soon as possible if it has been in place for more than 7 days. Do not allow catheter removal or change to delay antibiotic treatment.9,13
Men with recurrent UTI
If a man presents with recurrent episodes of lower urinary tract infection (UTI), for example, two or more episodes in the last 6 months, you should treat each episode as for acute lower UTI and ensure urine culture is arranged on each occasion.13
Advise the man about behavioural and personal hygiene measures and self-care treatments that may help to reduce the risk of UTI, for example, drinking enough fluids to avoid dehydration and not delaying habitual and post-coital urination.
Seek specialist advice on further investigation and management or refer to urology.
Ensure that any current UTI has been adequately treated then consider a trial of daily antibiotic prophylaxis if behavioural and personal hygiene measures alone are not effective or not appropriate. Take into account:
- The severity and frequency of previous symptoms
- The risks of long-term antibiotic use
- The risk of developing complications
- Previous antibiotic use, urine culture and susceptibility results.
Refer urgently using a suspected cancer pathway referral for an appointment within 2 weeks if a urological cancer is suspected.
Consider non-urgent referral for bladder cancer in men aged 60 years and over with recurrent or persistent unexplained UTI.11
Think about prophylaxis for men with recurrent UTI (Table 2).
Conclusion
Urinary tract infection is a common presentation in primary care. Most patients will present with uncomplicated infections and classic symptoms. However, practice nurses are uniquely placed to deal with atypical presentations and the full range of complexity of patients, male and female, young and old, pregnant* and those at high risk of complications.
* See Prescribing in pregnancy: the role of independent and supplementary nurse prescribers at: https://www.rcn.org.uk/clinical-topics/medicines-management/prescribing-in-pregnancy
REFERENCES
1. Butler C, Hawking M, Quigley A, McNulty C. Incidence, severity, help seeking, and management of uncomplicated urinary tract infection: a population-based survey. Br J Gen Pract 2015;65(639):e702-707
2. Little P, Moore M, Turner S, et al. Effectiveness of five different approaches in the management of urinary tract infection: randomised controlled trial. BMJ 2010;340:c199
3. Butler C, Francis N, Thomas-Jones E, et al. Variations in presentation, management, and patient outcomes of urinary tract infection: a prospective four-country primary care observational cohort study. Br J Gen Pract 2017;67(665):e830-e841
4. NICE Clinical Knowledge Summaries. Urinary Traction Infection https://cks.nice.org.uk/
5. Dason S, Dason JT, Kapoor A. (2011) Guidelines for the diagnosis and management of recurrent urinary tract infection in women. Canadian Urological Association Journal 2011;5(5):316-322.
6. EAU. Urological infections. European Association of Urology; 2018 https://uroweb.org/
7. Lee U. (2018) Urinary tract infections in women. BMJ Best Practice 2018. https://bestpractice.bmj.com/topics/en-gb/77
8. NICE QS90. Urinary tract infections in adults (QS90); 2015 https://www.nice.org.uk/guidance/qs90
9. Milo G, Katchman EA, Paul M, et al. Duration of antibacterial treatment for uncomplicated urinary tract infection in women. Cochrane Database Syst Rev 2005;(2):CD004682
10. NICE CG139. Healthcare-associated infections: prevention and control in primary and community care; 2012 (Updated February 2017). https://www.nice.org.uk/guidance/cg139
11. NICE NG109. Urinary tract infection (lower): antimicrobial prescribing; 2018 https://www.nice.org.uk/guidance/ng109
12. NICE NG113. Urinary tract infection (catheter-associated): antimicrobial prescribing. https://www.nice.org.uk/guidance/ng113
13. NICE NG112. Urinary tract infection (recurrent): antimicrobial prescribing. https://www.nice.org.uk/guidance/ng112
14. Public Health England. Diagnosis of urinary tract infections: quick reference tool for primary care; 2018. https://www.gov.uk/government/publications/urinary-tract-infection-diagnosis
15. Scottish Intercollegiate Guidelines Network. SIGN 88. Management of suspected bacterial urinary tract infection in adults: a national clinical guideline; 2018. https://www.sign.ac.uk/assets/sign88.pdf
16. Wound, Ostomy, and Continence Nurses Society (WOCNS). Care and management of patients with urinary catheters: a clinical resource guide; 2016. https://cdn.ymaws.com/www.wocn.org/resource/resmgr/publications/Care_&_Mgmt_Pts_w_Urinary_Ca.pdf
Related articles
View all Articles