Helping women through the perimenopause
Nichola Walker
Nichola Walker
RGN, MSc, MSc
Advanced Nurse Practitioner,
Offender Health & PhD student
Keele University School of Nursing and Midwifery
Jane Jervis
RN, RNT BH (Hons), MSc, PhD
Lecturer of Nursing
Keele University School of Nursing and Midwifery
June Keeling
RGN, RM, BSc (Hons), Med, PhD
Professor of Women’s Health
Keele University School of Nursing and Midwifery
Andrew Finney
RN, RNT, BSc (Hons) PhD
Senior Lecturer of Nursing
Keele University School of Nursing and Midwifery
Practice Nurse 2022;52(2):26-29
Every woman, who lives long enough, will go through menopause and is likely to live a third of her life post-menopausal, and around one in four women experience severe debilitating symptoms. With increased life expectancy, management of the perimenopause and post reproductive health is of growing importance
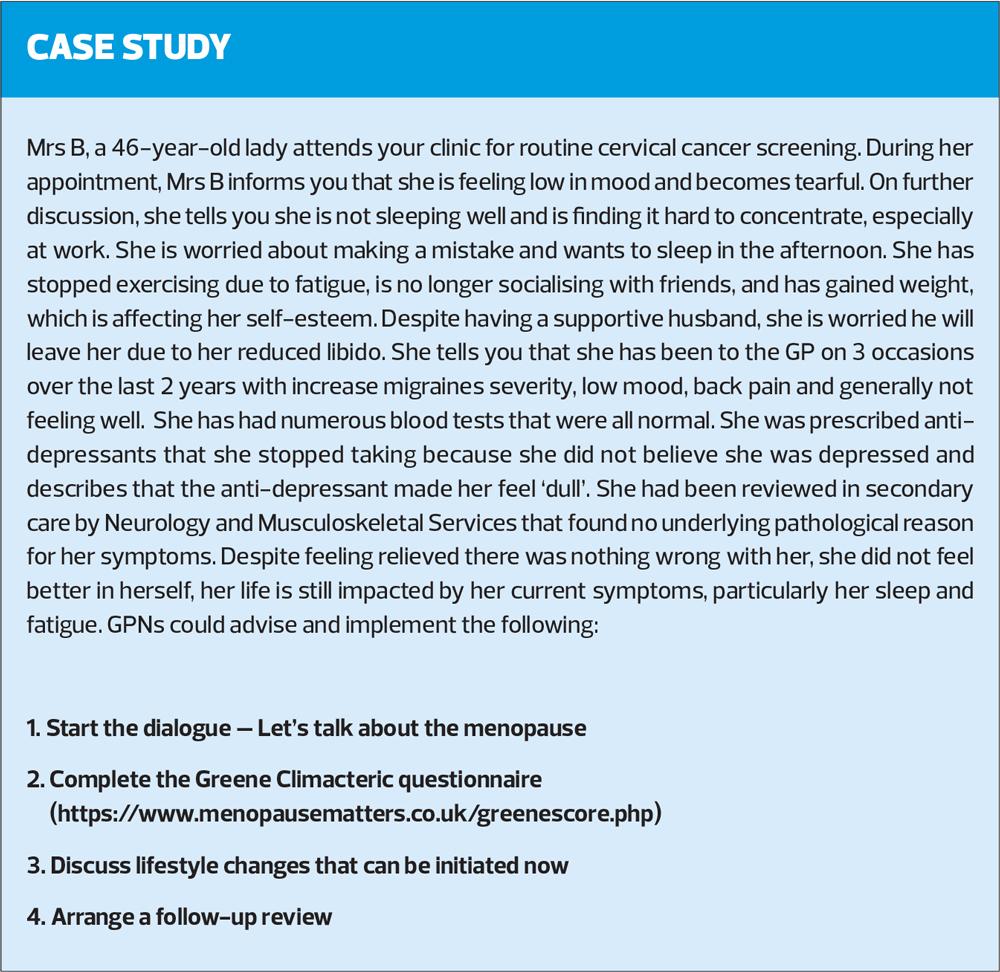
For women ‘of a certain age’ there is a wealth of information around the topic of menopause, but this is less so when focussing on perimenopause and its symptoms. Perimenopause is the period prior to the menopause and can have a significant impact on a woman’s wellbeing and span over several years.1 The perimenopause is the woman’s journey towards menopause and marks the end of her reproductive life.2 This time in a woman’s life may cause intolerable symptoms such as hot flushes, sleep disturbance, mood changes and general feelings of being unwell. During this period woman may seek help regarding possible treatment and wellbeing advice from their GP or GPN. Their decisions to engage in symptom management and possible disease prevention such as heart disease, diabetes and stroke can be positively influenced by their GPN. Instead, tabloid headlines, social media and networking with friends can result in misinformation, scare mongering and undertreatment of insufficient hormones, such as oestrogen.
This article seeks to inform of the need for a clear understanding of terminology around menopause, and an understanding of why it is important to identity, talk to and educate women so they can make informed decisions regarding their health and wellbeing during the perimenopause. GPNs are at the forefront of providing early education particularly during such interventions as cervical cancer screening and national health screening check, which can offer opportunities to address perimenopause signs and symptoms.3 Classifying the various stages throughout the menopause journey is important to guide assessment, treatment, and support for our patients. It should go without saying that treatment options and practical advice should be evidence based.4
SOME DEFINITIONS
It is important to define the later stages of the reproductive years, and to familiarise yourself with the terminology surrounding it.
- Menopause before the age of 40 years is termed premature menopause, or premature ovarian insufficiency5
- Early menopause is the cessation of ovarian function occurring between the ages of 40 and 45 years, in the absence of other causes of secondary amenorrhoea6,7
- The years leading up to the menopause can be termed, variously, perimenopause, menopause transition or climacteric, and may occur as early as the late 30’s8
- While ‘menopause’ is defined as the final menstrual period, a diagnosis cannot be ascertained until the woman has had no menstrual periods for 12 months8
- Post-menopause is diagnosed 1 year after final menstrual period8
NICE refers to ‘menopausal women’ to include perimenopausal and post-menopausal phases.
PERIMENOPAUSE
Menopause is a ‘natural’ biological stage in a woman’s reproductive cycle as a result of the non-pathological decline in oestrogen production with increasing age.9 Despite some variation of menopausal age between different ethnic groups,10 the average age in the UK of ‘natural’ menopause is 51 years of age.8
During the perimenopause, the endocrinological, biological, and clinical features of approaching menopause start.8 For some women this stage may last only a few months or continue up to 10 years.11 The average length of perimenopause is 4 years.11
Why is perimenopause management important?
Every woman, who lives long enough, will go through menopause and is likely to live a third of her life post-menopausal.2
- 13 million women in the UK are either peri- or post-menopausal and are the fastest growing demographic in the workforce.12
- 1 in 4 women are said to be experiencing severe debilitating symptoms that can impact their day-to-day living.13,14
- 1 in 5 women will take time off from work to deal with menopausal symptoms.14 Furthermore 1 in 50 women are on long term sick leave.14
With increased longevity due to improved healthcare systems and lifestyles, management of the perimenopause and post-reproductive health is of growing importance and is high on the parliamentary agenda and that of large workforce employers.1
Although the perimenopause and menopause are a part of a natural aging process the reduction in anti-inflammatory hormones, such as oestrogen, and possible weight gain, can have a negative impact on a woman’s lifestyle and quality of life. This poses many health risks and can contribute to long term conditions such as osteoporosis, diabetes, heart disease and cancers.2,11
SIGNS AND SYMPTOMS OF PERIMENOPAUSE
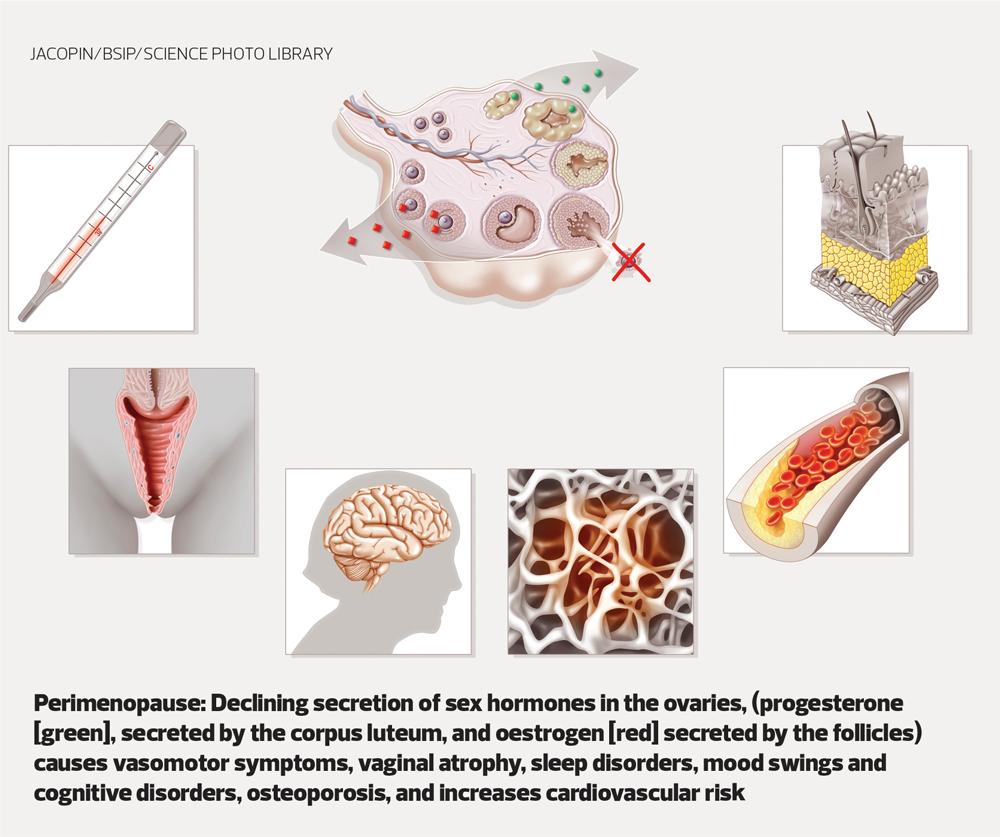
During perimenopause, the body produces less androgen, oestrogen, testosterone, and progesterone, causing hormonal fluctuations.15 These fluctuations in hormone levels can cause vasomotor, urogenital and psychogenic symptoms.
- Approximately 75% of women experience vasomotor symptoms, hot flushes, sweating, menstrual changes and pre-menstrual syndrome. These may be worsened by alcohol, eating high sugar foods, emotional stress, and exertion. Migraines may change in intensity and severity.7
- Approximately 60% of women experience urogenital symptoms and urinary urgency. These symptoms include genitourinary syndrome of menopause (GSM), which includes vaginal atrophy16 urethral atrophy, and sexual dysfunction (i.e., a decline in libido). GSM results in dryness, itching/irritation, and dyspareunia (painful intercourse). Urethral atrophy can result in stress incontinence, frequency, urgency, and dysuria.7
- Approximately 45% of women experience psychogenic symptoms that can include anger/irritability, anxiety/ tension, depression, sleep disturbance, loss of concentration (brain fog), and loss of self-esteem/confidence.7
A less well known perimenopausal symptom is dry skin,17 and approximately 61% of perimenopausal and menopausal women are affected by dry eyes.18
These symptoms can be fleeting or become part of a woman’s daily life for many years and can be mild one day but severe the next. However, an alteration in menstrual pattern is often the first change that the woman herself may recognise.
ASSESSMENT AND DIAGNOSIS
Managing perimenopause can be a challenge to healthcare professionals. Some women may present with mild symptoms, while for others, their symptoms will be truly debilitating, affecting all aspects of their lives and general wellbeing. Hormone levels do not decline steadily during the perimenopause but are often erratic, and symptoms may also fluctuate.
Following primary ovarian failure (when oestrogen levels are too low to trigger ovulation), production of follicle stimulating hormone (FSH) increases. However, while routine measurement of FSH is not recommended in women aged over 45 years, in women aged 40 to 45 with menopausal symptoms, an FSH test may be considered to aid diagnosis.19
Woman who are considered otherwise healthy and are over the age of 45 can be diagnosed as perimenopausal based on their symptoms. This should involve a good patient history to include symptoms (vasomotor) and altered menstruation
GPNs can use the ‘Greene Climacteric Scale’ (https://www.menopausematters.co.uk/greenescore.php) to assess menopausal symptoms and aid diagnosis.20 The scale, which can be used at any time during the perimenopause, can be used to assess changes in different symptoms, particularly before and after treatment. It measures three main symptom groups: psychological, physical, and vasomotor. It is scored from 0 (no symptoms) to 3 (severe), and can also be used to identify women who are clinically anxious or clinically depressed.
The organisation, Menopause Matters, also provides a checklist (http://www.menopausematters.co.uk/pdf/VAchecklist.pdf) that patients can use to report symptoms associated with vaginal atrophy, which they may feel too embarrassed to volunteer.
RULING OUT RED FLAGS
Early detection of red flags is vital for patients’ health, prevention of life-threatening diseases and to improve patient outcomes. This can be achieved by breaking down the symptoms and excluding other causes such as disease, trauma, infections, drugs, alcohol, or psychomotor conditions.21 It is therefore of great importance that GPNs can identify clinical features unrelated to perimenopause or menopause. These may include endometrial polyps; uterine fibroids; adenomyosis; endometrial hyperplasia or cancer; and vulval, vaginal, or cervical lesions.21,22
Referral to appropriate services should be considered for amenorrhoea, hot flushes (if ovarian failure is uncertain), vaginal atrophy and urinary incontinence.21
Urgent referral is recommended for women with postmenopausal bleeding (PMB) not taking HRT, and unexplained PMB in women who have stopped taking HRT or are receiving hormonal treatment for breast cancer.22
TREATMENT OPTIONS
Approximately two thirds of women say there is a general lack of support and understanding regarding perimenopause.23 Some woman report receiving great menopause care, but others do not. There are several possible reasons for this, which may include whether the presenting symptoms are menopause-related or not, can they be managed with medications, the medication efficacy in controlling presenting symptoms, the safety of prescribed medication, i.e. HRT. The patient’s own lifestyle may also impact on treatment options.
During perimenopause, symptoms may change and initially improve with treatment but treatment may become less effective as time goes by. Treatment options need to be adapted to suit current need, and – for example – the dose of HRT may need to be increased. GPNs should always revisit potential red flags if symptoms change, worsen, or don’t improve.
If treatment is commenced, a 3-month follow-up to assess efficacy and tolerability should be arranged. Once treatment efficacy is established then regular yearly follow-ups should be undertaken. Patient counselling should include when to arrange for further consultation to discuss potential treatment ineffectiveness, side effects or adverse events.
GPNs should consider referral to specialised menopause services if treatments do not improve the patient’s perimenopausal symptoms, or she has ongoing troublesome side effects, contraindications to HRT or uncertainty about the most suitable treatment options.24 However, it is worth mentioning that currently there are only 29 NHS menopause clinics in the UK, with waiting times for appointments of up to 6 months.14
Some women may decide not to take prescribed medications and may seek alternative therapies during perimenopause and menopause, about which they may seek the GPN’s advice, for example, about isoflavones or black cohosh to relieve vasomotor symptoms. They should be made aware that the safety, quality, purity and constituents of the different preparations on the market is often uncertain, and information about potential drug interactions (e.g. with tamoxifen, anticoagulants, and anticonvulsants6) may not be available.24
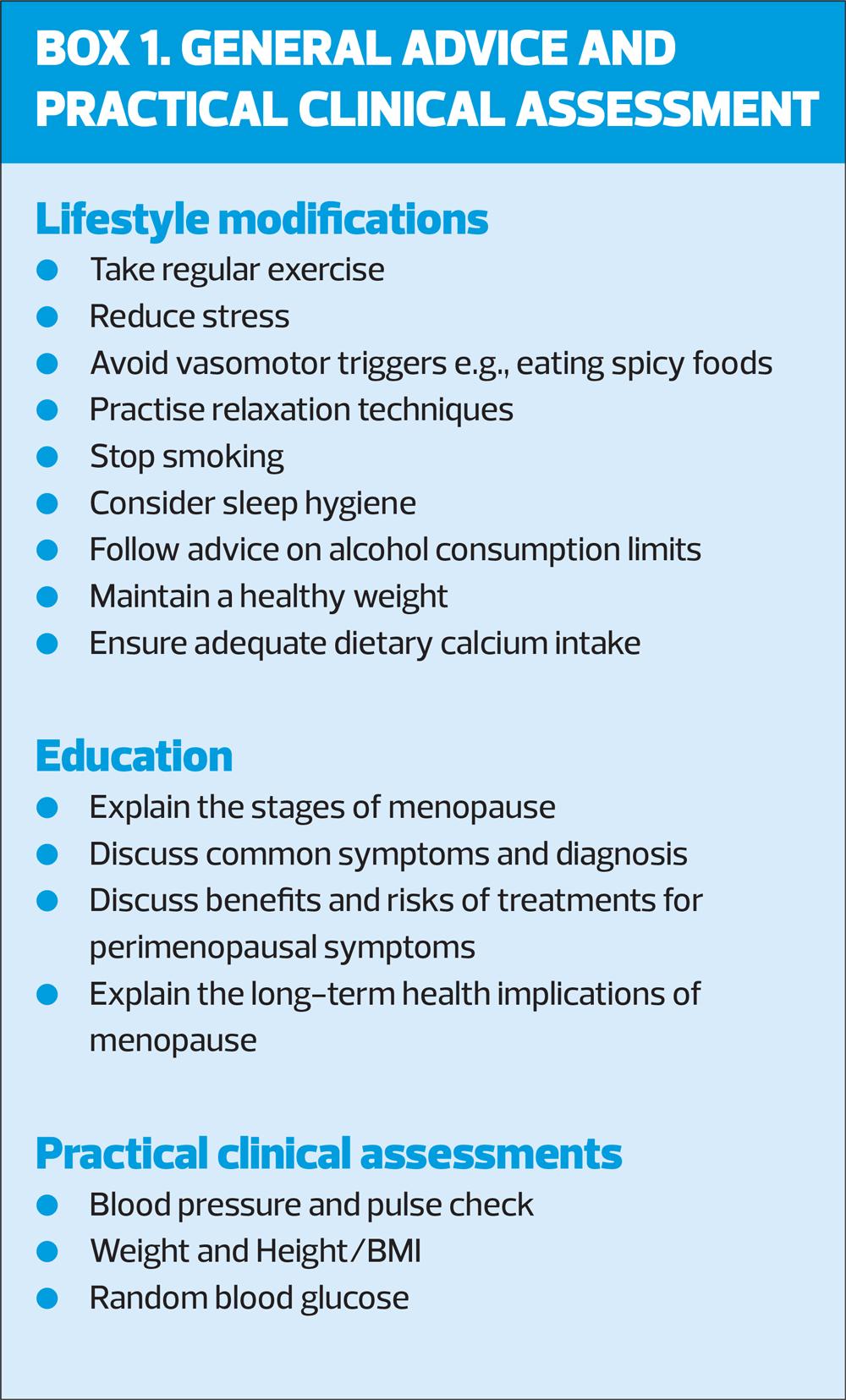
General advice for women during the perimenopause should include lifestyle modifications where indicated, and education on general health and wellbeing (Box 1).
Woman should also be encouraged to keep up to date with nationally recommended health screening.24
CONCLUSION
The lack of awareness around perimenopause can lead to unidentified signs and symptoms which may therefore go undiagnosed. As a result, this could delay valuable patient education and treatment. Due to hormonal fluctuations, diagnosis of perimenopause can be difficult, but this article has attempted to provide GPNs with useful resources to support and provide the necessary care during the perimenopause. GPNs are in position to lead on future care provision for this group of patients.
REFERENCES
1. Castro N. Birkhauser M. Samsioe M. Lambrinou-daki G. I EMAS position statement: the ten-point guide to the integral management of menopausal health, 2015 https://cursos.aapec.org/images/maturitas_(emas)10_points_guide.pdf
2. Menopause matters. Menopause: What and when is menopause, 2021 https://www.menopause matters.co.uk/menopause/index.php
3. Bostock-Cox B. Focus on women’s health: The menopause. Practice Nurse 2015;45(5):10-14. https://www.practicenurse.
co.uk/index.php?p1=articles&p2=1139
4. NICE guideline NG197. Shared decision making; 2021 https://www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/nice-guidelines/shared-decision-making
5. NICE NG23. Premature menopause: premature ovarian insufficiency; 2019 https://www.nice.org.uk/guidance/ng23/ifp/chapter/premature-menopause-premature-ovarian-insufficiency
6. Stuenkel CA, Davis SR, Gompel A, et al. Treatment of Symptoms of the Menopause: An Endocrine Society Clinical Practice Guideline. J Clin EndocrinolMetab 2015;100(1):3975-4011
7. Armeni E, Lambrinoudaki I, Ceausu L, et al. Maintaining postreproductive health: A care pathway from the European Menopause and Andropause Society (EMAS). Maturitas 2016;89:63-72 https://pubmed.ncbi.nlm.nih.gov/27180162/
8. NICE NG23. Menopause: diagnosis and management; 2019 www.nice.org.uk/guidance/ng23
9. Peacock K, Ketvertis KM. Menopause. StatPearls 2021; https://www.ncbi.nlm.nih.gov/books/nbk507826/
10. Study of Women’s Health Across the Nation (SWAN). Investigating Health for Midlife and Older Women, 2021 https://www.swanstudy.org
11. British Menopause Society. Information for health professionals; 2021 https://www.thebms.org.uk
12. Brewis J. Menopause transition: effects on women’s economic participation; 2017 https://www.gov.uk/government/publications/menopauses-transition-effects-on- womens-economic-participation
13. Local Government Association. Menopause factfile: Important things for employers to know about the menopause and how it affects women in the workplace; 2020 https://www.local.gov.uk/our-support/workforce-and-hr-support/wellbeing/menopause/menopause-factfile
14. NHS Employers. Menopause and the workplace: Information on how menopause can affect people at work, and practical guidance for employers on how to improve workplace environments for them; 2021 https://www.nhsemployers.org/articles/menopause-and-workplace
15. Menopause Now. Androgens and Menopause (Testosterone and Others); 2019 https://www.menopausenow.com/androgens-and-menopause
16. Mayo Clinic. Vaginal atrophy; 2021 https://www.mayoclinic.org/disease-conditions/vaginal-atrophy/symptoms-causes/sync-20352288
17. Kraft S. Dry Skin and Menopause; 2018 https://www.healthywomen.org/your-health/menopause-aging-well/dry-skin-and-menopause
18. The North American Menopause Society, Menopause and eye health, 2021 https://www.menopause.org/for-women/menopauseflashes/women’s-health-and-menopause/menopause-and-eye-health
19. NICE CKS. Menopause: When should I suspect a diagnosis of menopause or perimenopause? 2020 https://cks.nice.org.uk/topics/menopause/diagnosis/diagnosis-of-menopause-perimenopause/
20. Menopause Matters. Menopause Symptoms: The Greene Climacteric Scale; 2021 https://www.menopausematters.co.uk/greenescore.php
21. NICE CKS. Menopause, 2020 https://cks.nice.org.uk/topics/menopause/
22. NICE NG12. Suspected cancer: recognition and referral; 2015 (updated 2021) https://www.nice.org.uk/guidelines/ng12
23. Nuffield Health. One person in four with menopause symptoms is concerned about their ability to cope with life, 2016 https://www.nuffieldhealth.com/article/one-in-four-with-menopause-symptoms-concerned-about-ability-to-cope-with-life
24. NHS. Menopause; 2018 https://www.nhs.uk/conditions/menopause/
Related articles
View all Articles