Cervical screening – giving patients more choice
BRIDGETTE LOVE
BRIDGETTE LOVE
NZRCN
Practice nurse in Box, Wiltshire
A simple change – offering a choice of position for cervical screening – could help increase the number of women coming forward for screening
Over recent years the Government, charities and women’s magazines have all been trying to suggest ways to increase the cervical screening uptake in the UK. As a New Zealand Practice Nurse working here for the last 10 years, I believe I can suggest a small practical change to help increase these numbers.
A survey of women I have screened confirms that offering a choice of position for the screening test could help to encourage more women to come forward for screening and not to delay having it done. This choice may also help women who have been sexually assaulted and who fear having the screening test.
In August 2018, Public Health England published advice on cervical screening and ideas for improving access and uptake. This guidance included issues around improving the National Cervical Screening Programme for women with disabilities and specific needs, and suggested that practice-based awareness campaigns could be useful. The guidance also discusses informed consent and the importance of positive experiences – how ‘fear and embarrassment are some of the main influencing factors for women who choose not to have screening’.1
According to Jo’s Cervical Cancer Trust cervical screening more than one in four women are not attending for a Cervical Screening test when invited, and attendance is currently at its lowest for the last 19 years in England.2 A survey completed by Jo’s Trust in 2017 stated that one in three women between the ages of 25-29 years did not attend for their first screening test when invited. Of the women surveyed, 52% said this was due to worry about embarrassment or painfulness of the procedure. Around 80% of women said their last screening test was either painful or embarrassing.3
Jo’s Trust also surveyed women over the age of 50 years, and this research showed one in three delayed their cervical screening tests overall; 32% said this was because they found the procedure embarrassing, and 14% were worried about it being painful.
ALTERNATIVE POSITION
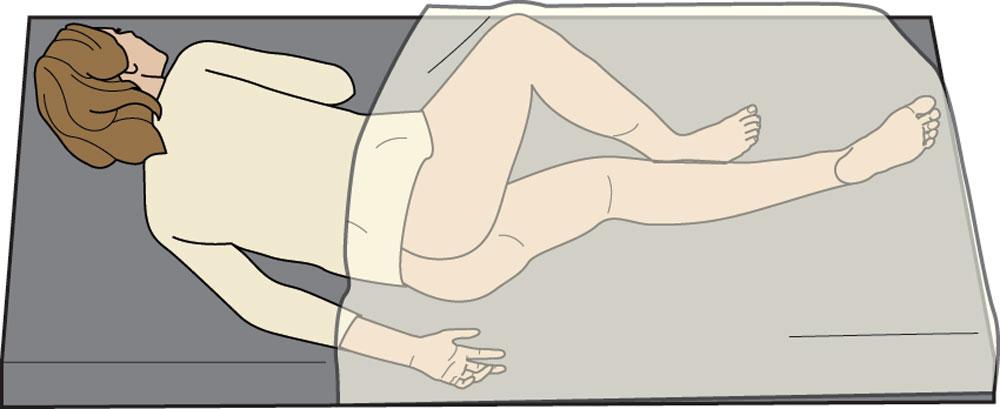
My cervical screening training took place in New Zealand, over 20 years ago, and I was taught both the dorsal (patient lying on her back) and the left lateral (lying on her left side) positions, according to the New Zealand Competencies for cervical screening education and training.5 Competency 8 states a competent sample taker ‘shall be able to demonstrate procedures for exposing the cervix and identifying the transformation zone, including dorsal and left lateral positioning.’5 The New Zealand National Cervical Screening Programme National Policy and Quality Standards for Cervical Screening, most recently updated in April 2017, states that a choice of position for the test, either dorsal or left lateral should be provided by the sample taker.6 In New Zealand, The Gynaecology Teaching Associates Information Booklet for Medical Students (2016) states ‘the practitioner observes the woman’s right to information by… providing a rationale as to why dorsal or left lateral positions are required, and if not specifically required, allowing the woman to choose the position’.7 In the UK, according to the RCN Human Papillomavirus, Cervical Screening and Cervical Cancer Guidelines June 2018, under the Examination section it states ‘Instruct the woman into the prone position (most common) or left lateral position, to assist in comfort and visualisation of the cervix’.8 According to the RCN both positions are professionally acceptable and yet only the dorsal position is taught and practised in the UK.
In the last 10 years of working in five different practices, I have offered all my patients the option of trying the left lateral position – also known as the Sims position – for their cervical screening test. I explain to each patient that I was trained in New Zealand where I was taught an alternative position of left lateral, and offer her the opportunity to try it. Some women have declined and I have completed the procedure in the dorsal position as requested, but I have found the majority have been willing to try the left lateral position. Some women prefer the dorsal position and have continued to be screened in this way, but a lot of women over the years have preferred the left lateral position. Most of my verbal feedback from women after the left lateral procedure has been that it is more comfortable, less painful, and less invasive than lying in the dorsal position. Some women have spoken to their friends and family about the left lateral position, and this positive feedback has encouraged more women to request this position for their cervical screening tests.
The more positive feedback I got from women about the left lateral position, the more encouraged and driven I became to try to inform both women and medical practitioners about offering this choice to other women. I have discussed the option of the left lateral with several UK colleagues over the years, both doctors and nurses, and while attending cervical screening update courses. Some medical practitioners have not heard of it, others have shown little interest in learning a new technique or in offering it to women.
As someone who can use both positions when screening, personally I find the left lateral position easier as the women’s legs do not needed to be manoeuvred while trying to insert the speculum: I aim for the spine each time and generally have no problem in locating the cervix. If a woman has a tilted cervix, either anterior or posterior, I find the left lateral position makes it easier to locate the cervix, and there is more freedom to manipulate the speculum because the handle is not pressing against the pubis. There is no need for women to sit on their fists to help locate a posterior cervix, which is often the way with the dorsal position. I find I can still converse with the woman and monitor their body language while using the left lateral position.
I am not suggesting that the left lateral position should be offered instead of the dorsal position for testing, but alongside as another option. I strongly believe women should be offered the choice, leaving the decision up to them, and ultimately empowering them with control over their own bodies and health.
QUESTIONNAIRE
Late last year I compiled a questionnaire for women to fill out anonymously (identifying their age only). The survey compared the level of comfort, level of invasiveness, and level of pain with sampling both in the dorsal and left lateral position, using a scale of 0 to 5 – with 5 being the most comfortable, least invasive, and least painful response. It asked for preferred position for future testing, and if a women had a tilted cervix, which position they found more efficient in locating the cervix. There was space at the end to comment if they felt inclined to do so.
In January this year I sent out 200 surveys to women who had had cervical screening tests done in both the dorsal and left lateral position only, and sent out a further 200 questionnaires in March.
RESULTS
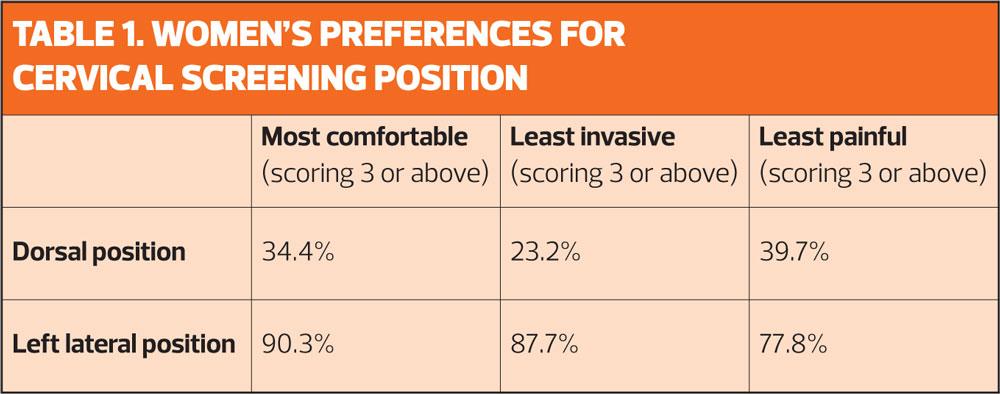
By the end of July I had received 202 completed surveys. The main results are shown in Table 1.
The overall preference for positions for future testing showed 77.8% would prefer the left lateral position, 8.4% were in favour of the dorsal position, and 13.8% said they would have either position again. Of the 34.2% of women who knew they had a tilted cervix, 92.7% said they found the left lateral position more efficient in locating their tilted cervix.
Of the 202 surveys returned, 81 women commented on their experiences and preferences, of whom only three preferred the dorsal position due to discomfort and pain and 76 expressed preference for the left lateral position.
I believe the preference was due to the increased level of comfort: the left lateral position is similar to the recovery position, and is how many women lie in bed. Lower levels of pain may be because, if the woman is more relaxed, her vaginal muscles will be less tense during the procedure.
Most women find the left lateral position less invasive because they are not directly exposing their genital area, and yet it does not compromise accessibility for the procedure.
Comments included:
‘I much prefer the lateral position. It was a revelation in how much more comfortable it was and felt much less intrusive. I really hope it becomes a permanent option.’
(Aged 47yrs)
‘Extraordinary difference! Having lived in fear of the next cervical smears for years, left lateral made it completely straightforward. Would highly recommend its adoption.’
(Aged 62yrs)
‘I had a cervical smear test in 2017 by the left lateral method, aged 64 years. It was the easiest, most comfortable that I have ever experienced. Previously I’d had the dorsal method and I was always very apprehensive beforehand as I found it to be painful and intrusive. If only I had known about [it] sooner I could have avoided years of anxiety and discomfort. For the benefit of other patients, I urge you to make them aware of the left lateral method and give them the choice. For me it was far less invasive and much more dignified that the dorsal experience, very little discomfort.’
(Aged 65yrs)
SEXUAL ASSAULT
Cervical screening can be particularly difficult for survivors of sexual assault, many of whom are deterred from attending because the test raises issues of intimacy and invasiveness.9
This issue was mentioned by one of the survey respondents, who said: ‘I cannot really put in to words how different the experience was. I have been a victim of rape and so find smear tests very traumatic. In the past when I have had smears (always dorsal position) I have been lying half naked on the examination bed for up to half an hour while other professionals have been called in to “have a go”. Not only is this humiliating and emotionally difficult, it is (has been) extremely painful. I felt almost no discomfort and a lot less vulnerable in the left lateral position. Unless someone can perform the smear test in the left lateral position I don’t want it done.
‘It is absurd that UK nurses are not trained to do so. This has to change!’
(Aged 34)
If the left lateral position was more widely available as a choice for survivors of sexual assault it might encourage them to feel more comfortable about having a cervical screen test, and to help them take back the power over their own bodies.
Offering an alternative choice of position for screening may be a practical way to help women overcome the issues of embarrassment and fear of screening tests. The left lateral position should not be offered exclusively over the dorsal position, but it is worth considering as an option to offer women. It is a small change that we as practitioners can make with a little training and practice, that could make a big difference to a lot of women in the UK, and increase the uptake of cervical screening. If the RCN guidelines advise the use of the left lateral position to assist in the comfort of the screening procedure then surely we should be able to use the technique in order to offer it as an option.
- As Practice Nurse went to press, Imogen Pinnell, Health Information Manager at Jo’s Trust informed us: ‘We’re updating our cervical screening information, and are including the left lateral positions in our pages on what happens during the appointment and tips to make the test better. We agree that it’s important people are given all the information to make the right choice for them, so are pleased to be able to flag this!’
REFERENCES
1. Public Health England. Cervical Screening: ideas for improving access and uptake, August 2018. https://www.gov.uk/government/publications/cervical-screening-coverage-and-data/cervical-screening-ideas-for-improving-access-and-uptake
2. Jo’s Cervical Cancer Trust. Increasing Cervical Screening Attendance, 2018. https://www.jostrust.org.uk/increasing-screening-attendance
3. Jo’s Cervical Cancer Trust. Barriers to Cervical Screening among 25-29yr olds, 2017. https://www.jostrust.org.uk/about-us/our-research-and-policy-work/our-research/barriers-cervical-screening-among-25-29-year-olds
4. Jo’s Cervical Cancer Trust. Further Understanding of the Perception of Cervical Screening among women over 50, 2017. https://www.jostrust.org.uk/about-us/our-research/further-understanding-perception-cervical-screening-among-women-over-50
5. New Zealand Ministry of Health. Competencies for Cervical Screening Education and Training, April 2017 https://www.nsu.govt.nz/system/files/page/competencies-for-cervical-screening-education-and-training.pdf
6. New Zealand Ministry of Health. National Cervical Screening Programme: National Policy and Quality Standards for Cervical Screening, 2017. https://www.nsu.govt.nz/system/files/page/ncsp_standards_1.pdf
7. Roberts H. Gynaecology Teaching Associates: Information Booklet for Medical Students. University of Auckland, New Zealand, 2016. https://flexiblelearning.auckland.ac.nz/webgyn5yr/11/files/gta_booklet_2017.pdf
8. Royal College of Nursing. HPV, Cervical Screening and Cervical Cancer Guidelines, 2018. https://www.rcn.org.uk/professional-development/publications/pdf-006903
9. Harvey-Jenner C. Why Survivors of Sexual Assault aren’t going for smear tests –Cosmopolitan, September 2018. https://www.cosmopolitan.com/uk/body/health/a22992357/survivors-sexual-assault-not-having-smear-tests/
Related articles
View all Articles