Setting up a travel health service
Jane Chiodini, MBE
Jane Chiodini, MBE
MSc(TravelMed), RGN, RM, FFTM
RCPS (Glasg), QN
Past Dean, Faculty of Travel Medicine
Practice Nurse 2023;53(01):8-12
Last time, Jane Chiodini provided guidance on delivering travel health services for those new to the field. This time, we look at what is involved in setting up an independent clinic for those who want to take the next step
Travel Medicine services have evolved over time, initially with delivery in general practice; niche provision in the occupational health sector; a few specialist, long-established private travel clinics; to more recently, an expansion in the number of travel clinics set up via specialist companies who saw a potential to expand their chains; multi-national pharmacy chains that set up clinics in their high street stores, and of late, community pharmacies keen to broaden their offering.
The impact of COVID-19 on the travel industry was dramatic with a 74% decline in international tourism, representing a loss of an estimated 1.3 trillion USD in international tourism expenditure. The United Nations World Tourism Organization published a number of interesting reports from the Committee for the Coordination of Statistical Activities and it was predicted that international tourism will take between 2.5 to 4 years to return to the 2019 levels.1 However, 2022 saw a fast recovery with several sub-regions, particularly in Europe, reaching 80% to 90% of their pre pandemic arrivals in January to September in that year and the Middle East exceeding them by 3%.2
Due to the increase in demand, more people are considering setting up a travel service. The specific needs will be very dependent on the nature and location in which such an operation is planned. While all GP surgeries in England must now provide travel advice and the NHS vaccines as an essential service, there is no obligation to provide private travel vaccines.3 However, a private, bespoke service can be developed in general practice, not only for your own patients, but as a service to any other surgeries in the area.
This article aims to highlight some of the key aspects that need to be considered for anyone considering setting up a service. Much research will be required and the following information is written as a general guide, not a blueprint for developing a business.
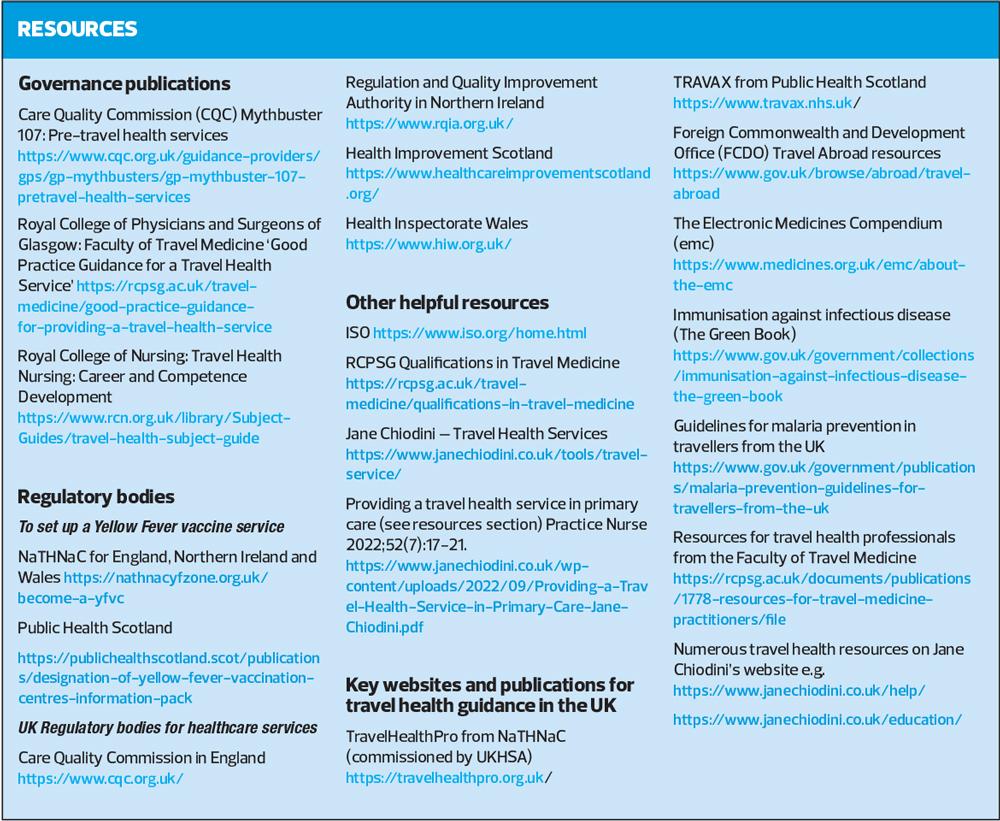
In the UK, travel health can be delivered by registered healthcare practitioners who are adequately trained and evidence competence in this field of practice. This can include doctors, nurses and pharmacists. The most important aspect of delivering travel health care is not which professional group delivers the care, but that each person doing so exceeds the minimum standard of practice and meets the health needs of the individual traveller.4 While anyone can potentially set up a service, and there are no set regulations on how to do so, guidance documents are now available to help support and guide best practice.4–6 These form essential reading for anyone intending to set up a service. See Resources for links to more detailed information on the subject. A travel clinic is subject to governance in terms of provision of yellow fever vaccine and also registration with regulatory bodies for example the Care Quality Commission, the independent regulator of health and social care in England.5
Any travel service – and especially one newly developed without previous customer experience – needs to take these concepts seriously, adapting and planning carefully for potential business demand.
There may be multiple reasons for wanting to set up a travel service and these could include:
- A passion for the subject and vision to be the master in charge of one’s own work environment and goals
- A desire to run a bespoke service to the highest of standards
- A need for a service if the location in which one is based is under-served
- A commercial goal to provide a good income-generating business
There is limited published information on setting up a travel service, particularly within the private healthcare sector – and probably for good reasons. The business will be competitive and so there will be limited desire to openly provide details for a competitor to come along and threaten the impact and potential of one’s own service. It may be that some individuals will provide a consultancy service to help develop a plan, but this would normally include a financial cost. It is very important to get the strategy correct, not least because setting up a bespoke service means confirming that a provider has specific expertise. Some factors to consider include:
- Training
- Governance
- Market considerations and financial implications
- Premises, equipment and consumables
- Documentation and additional services
TRAINING
It is strongly recommended that all healthcare professionals delivering travel health have a minimum of 15 hours of initial training and subsequent mentorship to ensure clinical competence.4,5 Full details of a suggested curriculum can be found in the Good Practice Guidance for Delivering a Travel Health Service publication (pages 15-17).4 The subject of travel medicine is vast and this minimum recommendation is just a starting point. It would be desirable that at least one person leading the clinical aspects has further training and preferably a post-graduate qualification. Courses are available at Professional Development Certificate, Diploma and Masters levels of study.7 This training will take considerable time, effort and funding, but sets the highest of standards in the delivery of care and the ability to supervise other clinical staff to a satisfactory level. Other clinic staff such as reception personnel would also benefit from introductory training so that they understand the complexity of travel health,2 making them a valuable asset as the initial customer-facing contact.
The provision of yellow fever (YF) vaccine is the exception to the rule: any clinic in England, Wales or Northern Ireland providing YF vaccination must be registered with NaTHNaC,8 and in Scotland, with Public Health Scotland.9 All those administering YF vaccine must also complete training and successfully complete an exit test every two years. These government bodies provide excellent information and training, but this is an additional requirement that must be considered and budgeted for.
As part of the professional revalidation process, in addition to travel health knowledge, other training is required such as general immunisation skills including injection techniques (which may require specialist intradermal technique depending on which vaccines are to be offered), cardiopulmonary resuscitation (CPR), anaphylaxis and safe-guarding (which must be taken to level three if seeing children).4,5 Annual training is mandatory for some of these areas, so it is important to identify good trainers and instigate a regular programme for all clinical staff.
Of interest, some companies offer a complete package including brief staff training, and software designed to guide the process of assessment and advice, and the vaccines required for their customers. They will also provide Patient Group Directions, for the administration of travel vaccines to their subscribers.
Once a clinic is established, there will always be a need for ongoing training in all aspects of clinical and administrative knowledge, to ensure staff are up to date and competent. This should also be included in annual appraisal and continuing professional development.4
GOVERNANCE
The individual delivering travel health care is governed by their registration body – the General Medical Council for doctors, the Nursing and Midwifery Council for nurses, and the General Pharmaceutical Council for pharmacists. Our codes of professional conduct are crucial to the safe standards we demonstrate in our work and care of patients. It is therefore important for anyone deciding to develop a travel service to understand the scope of practice involved in travel medicine.
Using a company as described above does not remove inherent professional obligations or accountability. It is the responsibility of each professional to practise only within their own competence and professional code of conduct. The healthcare professional consulting with the traveller remains accountable for their own practice and must be fully trained and competent to undertake such tasks.4,5
The legal framework for understanding the prescribing of travel vaccines must be addressed and suitable processes put in place. If the person performing the pre-travel risk assessment is not an independent prescriber, PGDs will be needed to support a smooth running service. Their development will take time and require a minimum involvement of a doctor and pharmacist.10,11 On occasion, patient specific directions may be of use and again, a full understanding of their purpose is required.11
In this private setting, additional services such as prescribing malaria chemoprophylaxis, medication to help prevent altitude illness12 and/or jet lag,13 should be considered, and suitable processes put in place. If your clinic wishes to sell medications online then extra regulation applies and further details can be found on the Medicines and Healthcare products Regulatory Agency website.14
Depending on the location in the UK, registration with a regulator will be required. The largest of these is the Care Quality Commission in England. The regulator for Scotland is Health Improvement Scotland, for Wales, Health Inspectorate Wales and for Northern Ireland, the Regulation and Quality Improvement Authority (see Resources). Their requirements are extensive and there is significant work to do to register so exploring the appropriate website before applying, identifying the required standards that would need to be met is a significant step forward. An example for the CQC can be found at https://www.cqc.org.uk/guidance-providers/registration/register-new-provider. Be aware that just preparing to apply can take several weeks’ work. Again there are companies that can help achieve registration – at a cost – and these options could be explored.
MARKET CONSIDERATIONS AND FINANCIAL IMPLICATIONS
Even before considering setting up a service and applying to a regulator, you need to carry out research in the area to find what other services may be present, the demographics of the locality and potential needs (e.g. a large population of travellers who may go away to visit friends and family, an affluent population taking exotic holidays, students/younger people taking adventure or gap year-type travel).
As part of the application process, the regulator will also require evidence of financial viability.15 Setting up a service, ensuring premises meet the standard, purchasing equipment (both clinical and administrative), developing marketing materials, website creation and ongoing maintenance, use of a software system to operate and document all aspects of the service from booking appointments to documentation of the consultation, patient literature etc. comes at considerable cost which must be planned. Insurance covering professional indemnity, premises, equipment and supplies needs to be taken out. You also need to consider other factors such as popular times for opening and the range of services it would be best to offer.
PREMISES, EQUIPMENT AND CONSUMABLES
The clinic premises need to be fit for purpose, including use of a lift if not situated on the ground floor. A minimally acceptable standard travel health service should include a consultation room which is in a confidential area, set aside from the general public, accessible to disabled individuals and large enough to hold the equipment described below.
Equipment outlay includes the provision of:
- Hand washing facilities with a water supply to meet infection control standards;
- Specialised vaccine fridges and additional temperature monitoring devices;
- Reclining clinical chair or clinical couch;
- Resuscitation equipment (minimum of anaphylaxis kit);
- Desk and chairs in the consultation room;
- Office and waiting room furniture
A company needs to be engaged to supply, collect and dispose of clinical waste and ‘sharps’. Ideally the clinical room should be air conditioned to maintain a comfortable ambient room temperature, important particularly in hot weather.
Consumables also need to be obtained so that there is a plentiful supply of syringes, appropriate sized needles, swabs, dressings, spot plasters etc. Products to enhance the service to travellers such as mosquito nets, insect repellents, a range of sunscreens, water purification bottles etc. can generate a reasonable profit, and you should explore the options from a number of travel product wholesalers.
Contracts for vaccine supply will need to be set up. There are many options for obtaining vaccines from wholesalers to direct business with the vaccine manufacturers. The impact of COVID and the decline in demand for travel vaccines has been problematic as a greater than expected need of new supplies has resulted in global vaccine shortages.16 Vaccines take a considerable length of time to manufacture and if you have a standing order from a manufacturer, you are more likely to get preferential access to new supply over those who do not commit to purchasing stock on a regular basis. Again, this takes planning and opening of accounts can take time. Always ensure that wherever you get your vaccines from, the delivery method maintains the cold chain at all times.17
DOCUMENTATION AND ADDITIONAL SERVICES
Documentation and record keeping is part of good governance and professional standards.4,5 The regulatory bodies will have their own requirements for many policies that will need to be developed, and guidance is provided for topics such as premises and equipment, good governance, employment, staffing, receiving and acting on complaints.18 Other considerations could include:
- Job descriptions and job plans
- Polices for health and safety, and infection control
- Equipment monitoring and maintenance
- Business recovery plan
- Confidentiality
- Audit of service
Clinical documents in the form of Standard Operating Procedures (SOPs) will also be required which provide a step by step guide e.g administering an injection, suspicion that a traveller is being taken abroad for the purpose of female genital mutilation (FGM), Duty of Candour if for example, an error was made administering an out of date vaccine to a patient.19
The International Organization for Standardization (ISO) is a body that brings together experts to share knowledge and develop voluntary, consensus-based, market relevant International Standards. They produce standards relating to documentation that can help a clinic. These detail the best way of laying out and indexing documentation.20 Examples of policies and SOPs can sometimes be found by searching on the internet.
CONCLUSION
Developing and running a travel service is very complex, challenging, demanding and a difficult pathway to take. Yet its rewards can be extremely satisfying especially for someone who wants to be involved in preventative healthcare of generally well patients attending, and enjoys the subject of travel medicine. For those who might consider it a lucrative business model, it is vitally important that they undertake a thorough review of all the aspects in this article and read extensively around the subject. Protecting the health of the traveller needs to be the first priority, but with careful preparation and planning, high standards can be achieved to deliver the care required. A webpage of further resources can be found at https://www.janechiodini.co.uk/tools/travel-service/.
REFERENCES
1. United Nations World Tourism Organization 2020. Impact of COVID-19 on International Tourism 20202. https://www.unwto.org/covid-19-and-tourism-2020 .
2. UNWTO Tourism Recovery Tracker 2022 https://www.unwto.org/tourism-data/unwto-tourism-recovery-tracker
3. Chiodini J. Providing a travel health service in primary care. Practice Nurse 2022;52(7):17-21
4. Chiodini JH, Taylor F, Geary K, et al. Good Practice Guidance for Providing a Travel Health Service; 2020. Faculty of Travel Medicine of the Royal College of Physicians and Surgeons of Glasgow. https://rcpsg.ac.uk/travel-medicine/good-practice-guidance-for-providing-a-travel-health-service
5. Royal College of Nursing. Competencies: travel health nursing: career and competence development; 2023 https://www.rcn.org.uk/professional-development/publications/pdf-006506
6. Care Quality Commission. GP mythbuster 107: Pre-travel health services; 2022 https://www.cqc.org.uk/guidance-providers/gps/gp-mythbusters/gp-mythbuster-107-pretravel-health-service
7. Royal College of Physicians and Surgeons of Glasgow. 2023. Qualifications in Travel Medicine https://rcpsg.ac.uk/travel-medicine/qualifications-in-travel-medicine
8. NaTHNaC Becoming a Yellow Fever Vaccination Centre (YFVC) in England, Wales and Northern Ireland (EWNI) https://nathnacyfzone.org.uk/become-a-yfvc
9. Public Health Scotland. Yellow fever vaccination centres https://www.hps.scot.nhs.uk/a-to-z-of-topics/yellow-fever-vaccination-centres/
10. NHS Specialist Pharmacy Service 2020. An introduction to PGDs: definitions and examples of use. https://www.sps.nhs.uk/articles/what-is-a-patient-group-direction-pgd/
11. Jane Chiodini. FAQ 1, Prescribing for Travel. 2022. https://www.janechiodini.co.uk/help/faqs/faq-1-prescribing-travel/
12. NaTHNaC 2021. Factsheet: Altitude Illness https://travelhealthpro.org.uk/factsheet/26/altitude-illness
13. Electronic Medicines Compendium. 2021. Melatonin 3 mg film-coated tablets https://www.medicines.org.uk/emc/product/10405/smpc#INDICATIONS
14. GOV.UK 2020. Guidance: Register for the Distance Selling logo. https://www.gov.uk/guidance/register-for-the-distance-selling-logo
15. Care Quality Commission. 2022. References and financial viability. https://www.cqc.org.uk/guidance-providers/registration/register-new-provider/references
16. NaTHNaC 2022. Vaccines and medicines: availability, supply, shortages and use of unlicensed medicines https://travelhealthpro.org.uk/factsheet/67/vaccine-supply-shortages-and-use-of-unlicensed-medicines
17. UK Health Security Agency. 2013 Storage, distribution and disposal of vaccines: the green book, chapter 3 https://www.gov.uk/government/publications/storage-distribution-and-disposal-of-vaccines-the-green-book-chapter-3
18. Care Quality Commission. 2022. Regulations for service providers and managers: related legislation https://www.cqc.org.uk/guidance-providers/regulations-enforcement/regulations-service-providers-managers-related
19. GOV.UK 2020. Guidance: Duty of Candour. https://www.gov.uk/government/publications/nhs-screening-programmes-duty-of-candour/duty-of-candour#when-to-apply-duty-of-candour
20. International Organization for Standardization (ISO) https://www.iso.org/standards.html
21. The United Kingdom Accreditation Service (UKAS) How to get UKAS Accreditation https://www.ukas.com/accreditation/about/how-to-get-ukas-accreditation/
Related articles
View all Articles