Self care: could it help ease pressures in general practice?
Mandy Galloway
Mandy Galloway
Editor, Practice Nurse
The benefits of self care are well established but while it is desirable, much more needs to be done to embed it in public consciousness. However, the need for patients to take more responsibility for their own health and to use services more appropriately has never been more acute
Many common conditions like coughs, colds and sore throats don’t need to be treated by a health professional, and self care may be the most appropriate solution in many cases.
But despite campaigns from organisations such as the Self Care Forum it doesn’t seem to be happening in the real world.
One reason why patients fail to embrace self care may be that health literacy levels in England are low. It is estimated that between 43% of English working age adults routinely do not understand key information related to their own health, rising to 61% when numeracy is also required for comprehension.1 This lack of understanding can have damning impacts, not just on patient health outcomes, but on stretched NHS services and capabilities, as well as contributing to health inequalities. People from more disadvantaged socioeconomic groups have been identified as having levels of health literacy that are disproportionately low or inadequate.
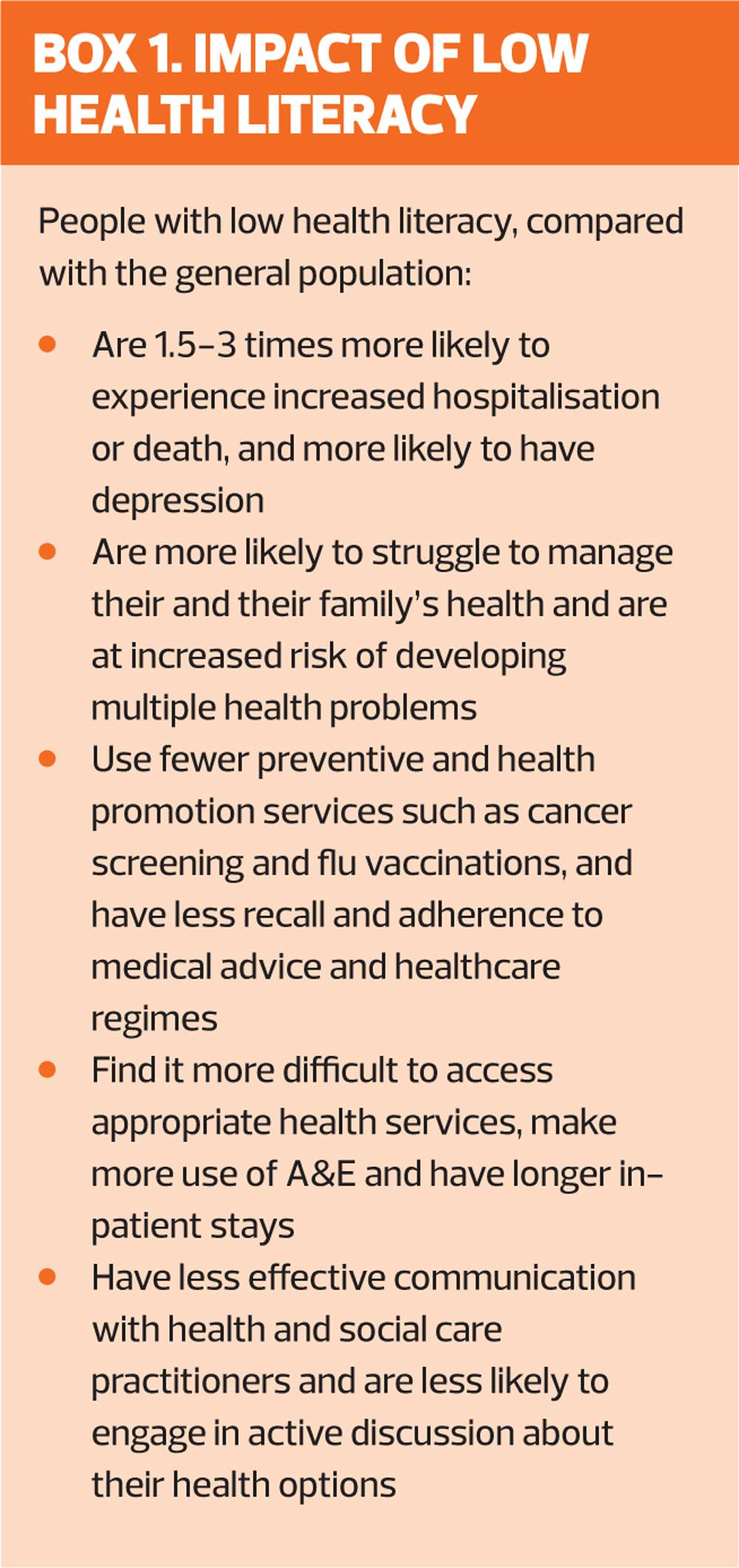
Low health literacy has a direct impact on the NHS and contributes to the strain the health service is currently under. Misunderstanding health advice and information increases the likelihood that people will misuse NHS services and be less able to participate in self care (Box 1).
Workload in general practice is estimated to have increased by 16% between 2007 and 2014. An ageing population with increasing incidence of multi-morbidity, a rising administrative burden from regulatory and statutory pressures, and inadequate resources all contribute to unsustainable pressures on GP workload.2
The General Practice Forward View, followed up by NHS England’s 10 High Impact Actions,3 aimed to address some of the challenges facing primary care.
But many of the ideas that have been put forward to free up time for GPs have been met with concerns that they will actually increase workload, especially in the short term.2
When the RCGP surveyed GPs about their response to the 10 point plan, GPs were sceptical and questioned the evidence base for some of the actions. But ‘supporting self care’ was viewed more positively.
Overall, 67% of GPs responding to the survey thought that supporting self-care would decrease workload. One third (32%) thought this would be by a lot, more than any other initiative. Even so, 9% of GPs thought that supporting self care would add to workload.2
There are challenges in effectively implementing this action. Potential obstacles include the time and effort required to educate patients effectively, the need for broader work beyond the efforts of individual practices to help educate the public, and the need to ensure that patients do not receive mixed messages.
The RCGP says: ‘Every opportunity should be taken to support people playing a greater role in their own health and care. This may be through better signposting to sources of information, advice and support in the community, including patient information websites, community pharmacies and patient support groups. For people with long-term conditions, this may involve working in partnership to understand patients’ mental and social needs as well as physical.’
Supporting self-care is already being tried by 42% of the respondents to the RCGP survey (conducted from December 2017 – January 2018). However, some patients are not made aware of alternative sources of effective care and advice, and there are suggestions that primary care clinicians may not know how best to go about it.
The Proprietary Association of Great Britain (PAGB), the organisation representing manufacturers of over-the-counter medicines, has called for self care to be included as a ‘key requirement’ in professional training for GPs and other healthcare professionals.4
In a report demanding a national strategy for self care,4 the PAGB argues that this measure would help improve public health literacy and reduce the burden on the NHS.
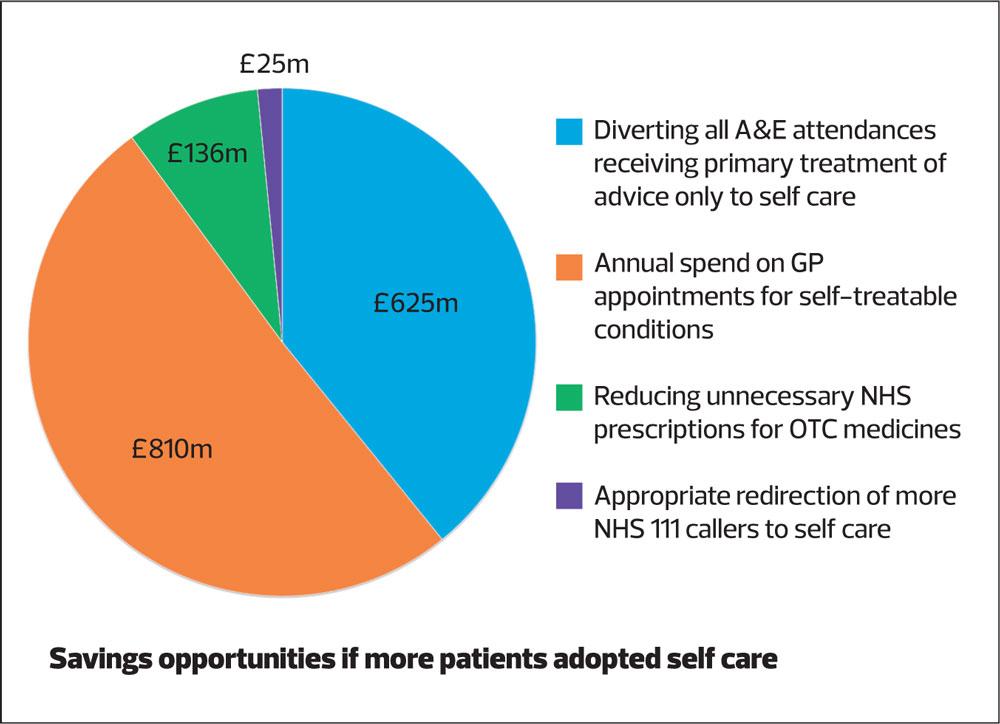
PAGB research reveals 34% of people admit to visiting a GP rather than a pharmacist for self-treatable conditions. Interactions with the NHS, including A&E attendances, GP appointments and prescriptions for over-the-counter (OTC) medicines, that could reasonably be dealt with elsewhere, cost an estimated £1.5 billion, which could be saved each year and re-invested into the NHS if more people were enabled to take care of their own health and self-treat.4
PAGB Chief Executive John Smith said: ‘We believe that self care is not only the responsibility of the individual but also of healthcare professionals, who need to provide advice and information that people can easily understand to help them identify the right care for their condition. Training healthcare professionals to support people to self care will improve health literacy and ultimately reduce unnecessary demand on the NHS.
‘Equipping HCPs with the knowledge and skills to self care should be a key focus of the NHS long-term plan. This would help to ensure a sustainable future, in terms of educating people how to manage self-treatable conditions, but also the complex challenges associated with the management of long-term health concerns, particularly in an ageing population.’
The PAGB recommendations, set out in ‘A long-term vision for self care: interim white paper’ also include:
- Introducing ‘recommendation prescriptions’ to direct patients to purchase medicines over the counter rather than on an NHS prescription, or to ‘prescribe’ behaviour change such as healthy eating or increased exercise.
- Improve NHS 111 signposting to self care options, i.e. referral of non-emergency patients to a pharmacist rather than to general practice or A&E.
- Enable community pharmacists to refer to other healthcare professionals
- Give community pharmacists ‘write access’ to patient medical records to enable medication or advice given to be recorded
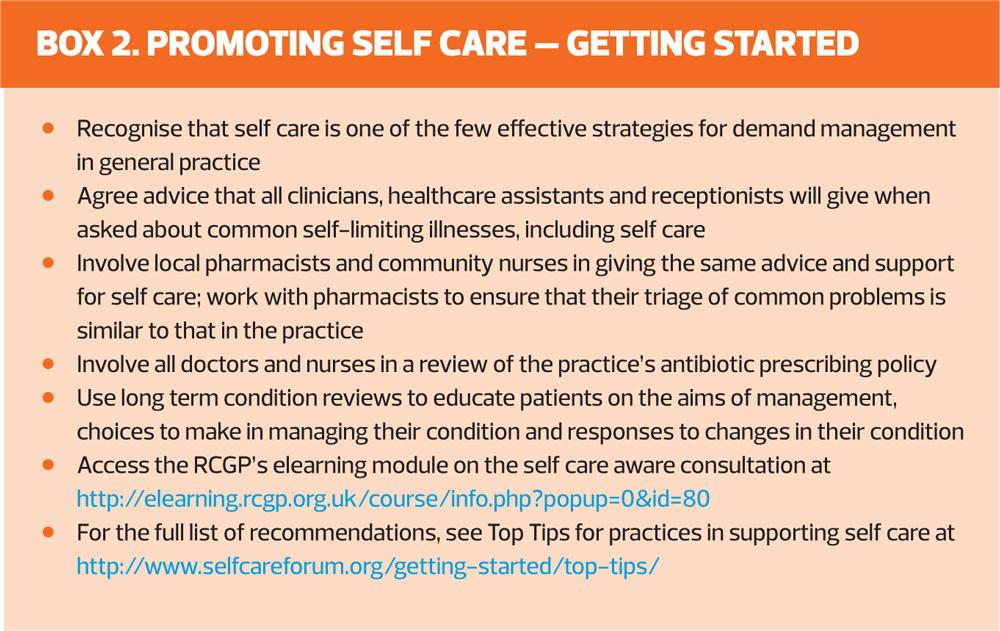
The Self Care Forum says promoting self care in general practice should be viewed as a long term project, but suggests that each practice takes on one or two steps to get started (see Box 2).5 The group says: ‘The “Holy Grail” is the self care aware consultation in which patients are asked if they have used self care before consulting and are praised for doing so; are encouraged, when appropriate, to consider self care options next time; are offered information and support on self-management of their condition and when to seek advice, and this is taken. The self care-aware doctor or nurse is a patient-centred, positive communicator and educator who is highly valued by patients.'
REFERENCES
1. Public Health England. Improving health literacy to reduce inequalities, 2015 https://assets.publishing.service.gov.uk/
government/uploads/system/uploads/attachment_data/file/460710/4b_Health_Literacy-Briefing.pdf
2. Royal College of General Practitioners. Spotlight on the 10 High Impact Actions, 2018. http://www.rcgp.org.uk/policy/general-
practice-forward-view/spotlight-on-the-10-high-impact-actions.aspx
3. NHS England. General practice development programme: 10 high impact actions to release time for care. https://www.england.nhs.uk/gp/gpfv/redesign/gpdp/
4. PAGB. A long-term vision for self care: interim white paper. https://www.pagb.co.uk/content/uploads/2018/07/A-long-term-vision-for-self-care-interim-white-paper.pdf
5. Self Care Forum. Top Tips for practices in supporting self care, 2018. http://www.selfcareforum.org/getting-started/top-tips/
Related articles
View all Articles