Overcoming barriers to self care
Mandy Galloway,
Mandy Galloway,
Editor
With general practice at breaking point and the press full of stories about how long patients are having to wait for appointments, what can practice nurses do to help manage demand?
Demand for GP services has reached unprecedented levels but a significant proportion of this pressure comes from people consulting for self-treatable conditions. Of the estimated 18 million ‘unnecessary’ appointments each year,1 5.2 million were for blocked noses, over 1 million were for backache, 40,000 were for dandruff and 20,000 were for travel sickness.2
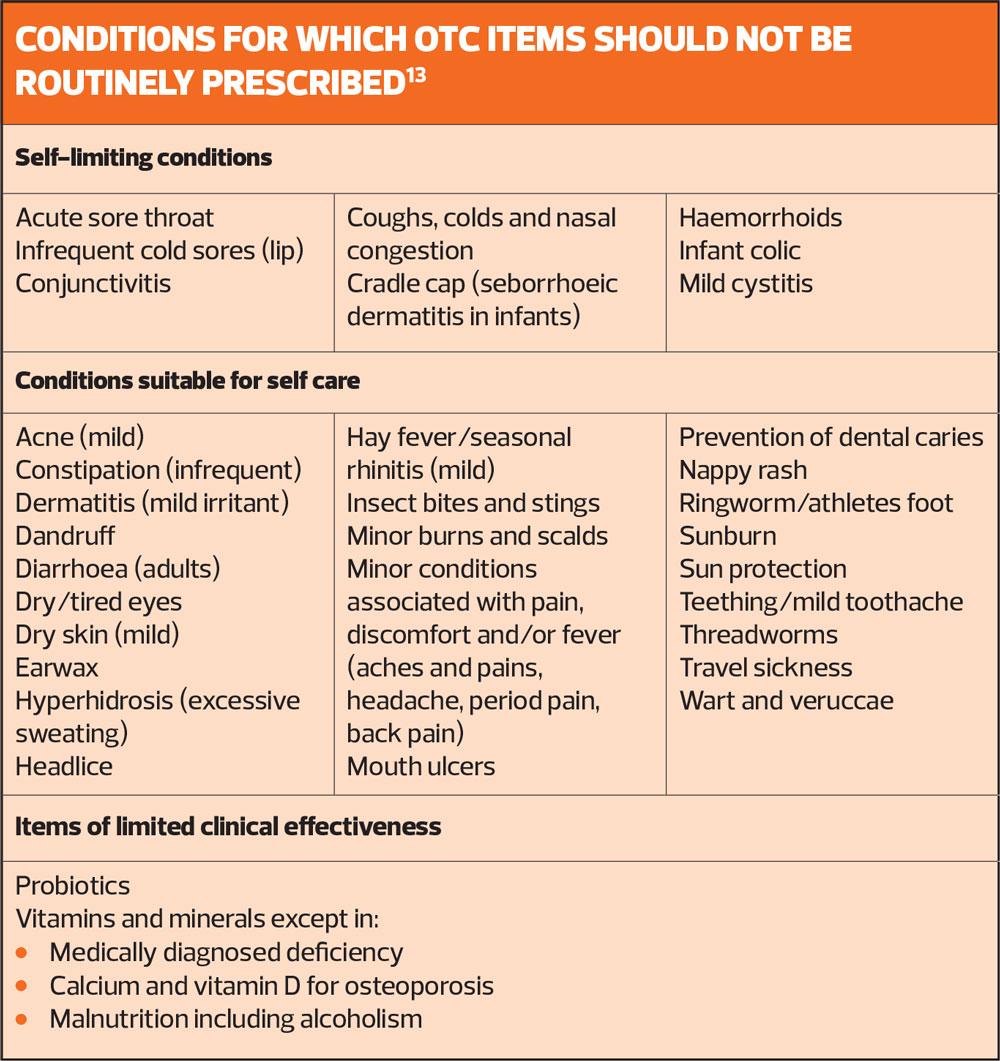
The NHS spends more than half-a-billion pounds on medicines which can easily be bought over the counter at a pharmacy or supermarket, including items for conditions that are self-limiting – and so do not need treatment as they will resolve on their own, and for conditions that lend themselves to self-care – i.e. the person suffering from the condition does not normally need medical care but could self-treat symptoms with an over-the-counter (OTC) medicine.3
A report from NHS England in 2018 found that each year, the NHS spends:
- £22.8m on constipation – enough to fund around 900 community nurses
- £3m on athletes foot and other fungal infections – enough to fund 810 hip replacements
- £2.8m on diarrhoea – enough to fund almost 3,000 cataract operations.3
The NHS has therefore produced guidance on conditions for which OTC items should not be routinely prescribed in primary care. It is worth noting that many of the products that were included in the guidance cost the NHS up to four times more than they would cost to buy in a pharmacy or supermarket once dispensing fees are taken into account – and more than ten times as much if the cost of the GP consultation is included.3
The Proprietary Association of Great Britain (PAGB), which represents the manufacturers of branded OTC – proprietary – products, says the move needs to be backed up with self care advice and recommendations for OTC treatments when patients attend the surgery with a self-treatable condition – a so-called ‘recommendation prescription’. This would not only support people to access the most appropriate level of care but also educate them on self-care in the longer term.4
PRESSURES IN GENERAL PRACTICE
As the first point of contact for most patients, GP surgeries are experiencing significant strain, with rising demand, practices struggling to recruit staff and patients having to wait longer for appointments.5
In October 2019, the monthly appointment count reached 31 million, the highest it has been since this data began to be recorded in mid-2018. Between 1 November 2018 and 30 October 2019, GP practices undertook 312 million consultations.5 Although the number of doctors entering GP training is higher than ever (3,538 training places in 2019), the number of full time equivalent (FTE) GPs has been decreasing since September 2015. A King’s Fund survey in 2019 found that of 840 trainee GPs, only 27% intended to work full time in general practice one year after qualifying.
Latest figures from NHS Digital show that there are currently 16,573 FTE general practice nurses, an increase of 1.8% from September 2018,6 but far fewer new nurses have entered general practice than the 5,000 ‘non-medical staff’ promised in the GP Forward View. The Nursing and Midwifery Council also points out that although there have been increases in the number of nurses on its register, the number of people on the register approaching retirement age is growing quicker than the number of those under 30.7
As a result of these staffing pressures, almost one-in-five patients waited longer than two weeks for an appointment from the time of booking,5 and according to reports in the Sunday Times, ’11 million patients have endured waits of more than three weeks to see a GP’. However, once they see a member of the general practice team, satisfaction with GP services remains high: the British Social Attitudes survey found that although public satisfaction has been eroded over time, it relates specifically to issues in getting an appointment, not quality of care.5
Diverting demand could result in significant financial savings. The PAGB estimates that £810m per year is spent on GP appointments for self-treatable conditions, £200m could be saved by reducing unnecessary prescriptions for OTC medicines for self-treatable conditions, and £518m could be saved if all A&E attendances resulting in a primary treatment of ‘guidance or advice’ were diverted – most probably to community pharmacy.8
RECOMMENDATION PRESCRIPTIONS
Both patients and clinicians tend to expect a consultation to result in a prescription.4
But a recommendation prescription provides self care advice or an OTC treatment recommendation when a patient presents with a self-treatable condition.
Healthcare professionals and policy makers have expressed concern that providing a physical prescription – albeit in recommendation form – would continue to foster patient reliance on general practice, encouraging people to continue to present with minor illnesses, rather than easing pressures on primary care.4
But when such a scheme was introduced in Germany, 91% of patients purchased the recommended OTC treatment, and evaluation of the scheme found that if they experienced the same symptoms, they remembered the advice and went directly to a pharmacist without consulting their GP first.4
The PAGB acknowledges that there would be modest costs to set up recommendation prescriptions in primary care, but says that these would be more than offset by the savings on prescription medicines. The PAGB is calling on NHS England to make a self care GP resource pack available for every Primary Care Network (PCN) to include recommendation prescription pads, a director of OTC products – ideally embedded into GP IT systems, and patient information leaflets such as those provided by the Self Care Forum.
Public Health England produced ‘Treat your infection’ non-prescription leaflets as part of its Keep Antibiotics Working campaign in 2017, which aimed to explain to patients why they had not been offered an antibiotic – or had been provided with a deferred prescription, with advice on self care measures such as analgesia and taking adequate fluids and resting. Almost all patients – 97% – said they found them helpful.9 Leaflets on respiratory and urinary tract infections are available from the PHE campaign resource website, at https://campaignresources.phe.gov.uk/resources/campaigns/58-keep-antibiotics-working/resources
HEALTH LITERACY
Among the barriers to implementing effective self care strategies are low levels of health literacy.
Health literacy is defined as ‘the personal characteristics and social resources needed for individuals and communities to access, understand, appraise and use information and services to make decisions about health’.10
But it is estimated that 43% of working-age adults in England do not have adequate literacy skills, and 61% of adults lack adequate numeracy skills to understand health information, with people from disadvantaged socioeconomic groups having disproportionately low or inadequate levels of health literacy.8
Low levels of health literacy impact on the individual’s ability to manage long term conditions, engage with preventative programmes, make informed, health lifestyle choices, and keep to medication regimes.10
Strategies to improve health literacy – or at least deal with low levels of health literacy on a practical level include using clear and simple language, using materials that employ tested pictures and symbols, and using ‘teach-back’ techniques to test comprehension. Teach-back involves asking the individual to repeat back to the healthcare professional what they have just heard. Rather than simply asking ‘do you understand everything we have discussed?’, ask – for example – ‘Can you tell me how you are going to explain [this] to your family when you get home?’ or ‘We discussed a lot today, can you tell me what you found most important?’
You an also use the ‘chunk and check’ technique, to break information down into short sections and assess understanding as you go.
THE SELF CARE AWARE CONSULTATION11
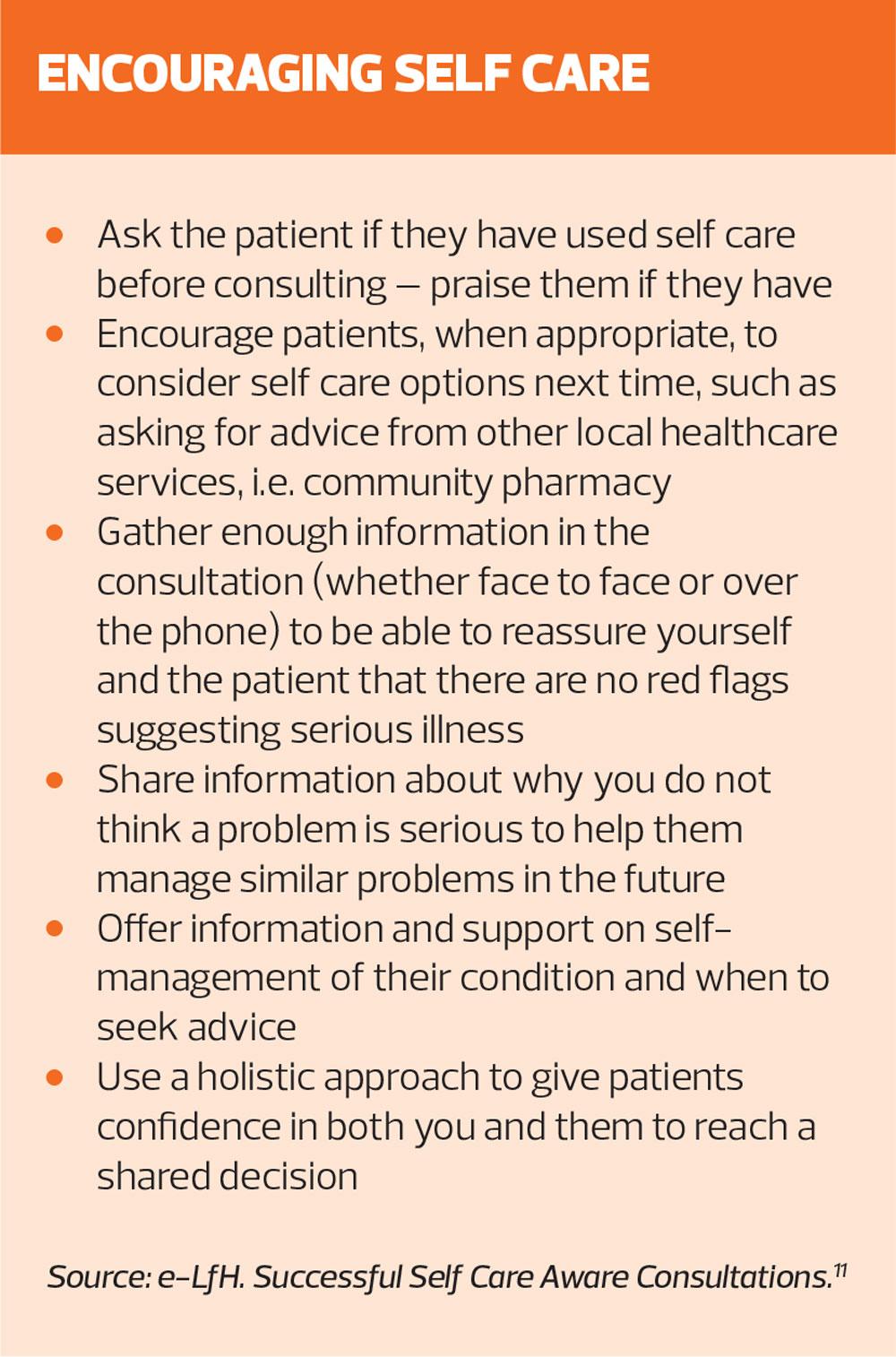
When a patient presents with a self-treatable condition, it is important to identify why they have sought a consultation, their ideas, concerns and expectations. While they may be expecting a prescription, their real agenda may be that they want reassurance, help to return to work, or simply a diagnosis. With some conditions, such as lower back pain, you should also rule out any serious pathology.
Topics you should cover in the self care aware consultation include:
- The patient’s use of OTC medicines, including dosages, frequency and duration
- Checking their understanding to ensure they are taking appropriate medicines correctly and safely
- The expected progression of the condition, and advice to seek appropriate medical attention if red flag signs or symptoms occur
- Give clear follow up advice and instructions if the ailment persists
- Support verbal advice with a patient information leaflet and/or advise the patient where to access evidence-based information, such as the NHS website (formerly NHS Choices) at https://www.nhs.uk or the Self Care Forum http://www.selfcareforum.org/fact-sheets/
Promoting self care involves harnessing your patient’s potential for independent action, and building a knowledge base and set of skills they can use in the future. You may need to provide support to family members as well as the individual, and provide information about the skills and knowledge of other healthcare professionals, e.g. pharmacists. Past experience with self care builds confidence, and the majority of those who have previously used self care will do so again for new episodes.11
Educating people with accurate information about the usual duration of common self-treatable conditions is essential – the patient may have presented soon after the onset of their condition, which had they waited, may have resolved spontaneously. However, clinicians also need to be vigilant for the patient who comes in to discuss an apparently self-limiting condition as a way of broaching their concerns about a more serious illness.11
Another strategy is to advise patients to purchase generic name OTC medications, and to keep supplies of these to hand in case similar symptoms recur in future.11 You should tactfully explain why you are not allowed to prescribe these medications on the NHS.
All healthcare professionals worry that they may be the subject of a complaint or litigation if they advise patients to try self care, and this may discourage them from promoting self-care.11
However, becoming a victim of the ‘compensation culture’ is less likely if patients are provided with adequate safety netting – ‘If you experience any of the following relevant red flags or aren’t feeling better after an appropriate interval, come back and see me again,’ and steps have been taken to eliminate serious pathology.
IMPLEMENTING SELF CARE IN PRACTICE – TOP TIPS
The Self Care Forum offers top tips to practices who want to promote self care, starting with recognition – throughout the team – that this is one of the few effective strategies for demand management in general practice. This means including self care messages and strategies in practice meetings, and incorporating self care into staff training.12
- It is important that everyone in the team delivers consistent self care messages for common self-limiting illnesses – for example, flu, chickenpox, headlice etc. Discuss the advice the clinical team will offer in future, make a note of it, and make it available electronically to all staff.
- Involve local pharmacists and community nurses so that everyone is giving the same advice and support for self care, and work with local pharmacists to ensure that their triage of common problems is similar to that in the practice.
- Involve all doctors and nurses in a review of the practice’s policy on antibiotic prescribing, to ensure consistency and best practice, and to ensure that patients do not perceive inconsistencies, which they may use to play one clinician off against another.
- Use long term condition reviews to inform and educate patients, carers and families on the aims of management, choices they can make and responses to changes in their condition. Support patients to make good choices to improve outcomes, allowing time to establish the patient’s own preferences and goals.
- Involve the patient participation group and others to design, plan and obtain feedback on your self care initiatives.
- Use your website, displays in waiting and reception areas and other media to support patients to self care. Guide your patients to online resources such as NHS Choices, Patient UK, Self Care Forum leaflets etc.
- Consider using self management courses such as Expert Patient Programme for some or all of your patients with long term conditions, or link with national patient groups such as Asthma UK.12
CONCLUSION
The self care aware practice nurse is a patient-centred, positive communicator and educator who is highly valued by patients.12 Supporting self care requires healthcare professionals and patients to engage in a two-way process and shared decision-making – it does not mean abrogating your responsibility or leaving the patient to simply ‘get on with it’. Converting just a small proportion of current consultations for self-limiting conditions to self care would deliver benefits to the practice and patients.11
REFERENCES
1. NHS campaign aims to drive patients to pharmacists. Practice Business, 2019. https://practicebusiness.co.uk/nhs-campaign-aims-to-drive-patients-to-pharmacists/
2. Local Government Association. Millions of ‘unnecessary’ GP visits are for coughs and colds. https://www.localgov.co.uk/Millions-of-GP-appointmentsunnecessaryand-cost-billions/41987
3. NHS England. Guidance on conditions for which over the counter items should not routinely be prescribed in primary care; 2018.
4. Proprietary Association of Great Britain (PAGB). Overcoming the barriers to self care. https://www.pagb.co.uk/content/uploads/2019/11/20191120_PAGB_Overcoming-the-barriers_A4_single_page.pdf
5. BMA. Pressures in general practice; 16 December 2019. https://www.bma.org.uk/collective-voice/influence/key-negotiations/nhs-pressures/pressures-in-general-practice
6. NHS Digital. General practice workforce 30 September 2019. https://digital.nhs.uk/data-and-information/publications/statistical/general-and-personal-medical-services/final-30-september-2019
7. NMC. Nursing and midwifery numbers continue to grow against backdrop of ageing register. Press release, December 2019. https://www.nmc.org.uk/news/press-releases/nmc-register-data-september-2019/
8. PAGB. Self care White Paper: supporting the delivery of the NHS Long Term Plan; March 2019. https://www.pagb.co.uk/content/uploads/2019/03/PAGB_Self-Care_White-Paper_v1-0.pdf
9. NHS England. Enabling people to make informed health decisions. https://www.england.nhs.uk/ourwork/patient-participation/health-decisions/
10. No author stated. Public Health England to relaunch antibiotic awareness. Br J Fam Med October 2018. https://www.bjfm.co.uk/phe-relaunch-antibiotic-awareness-campaign
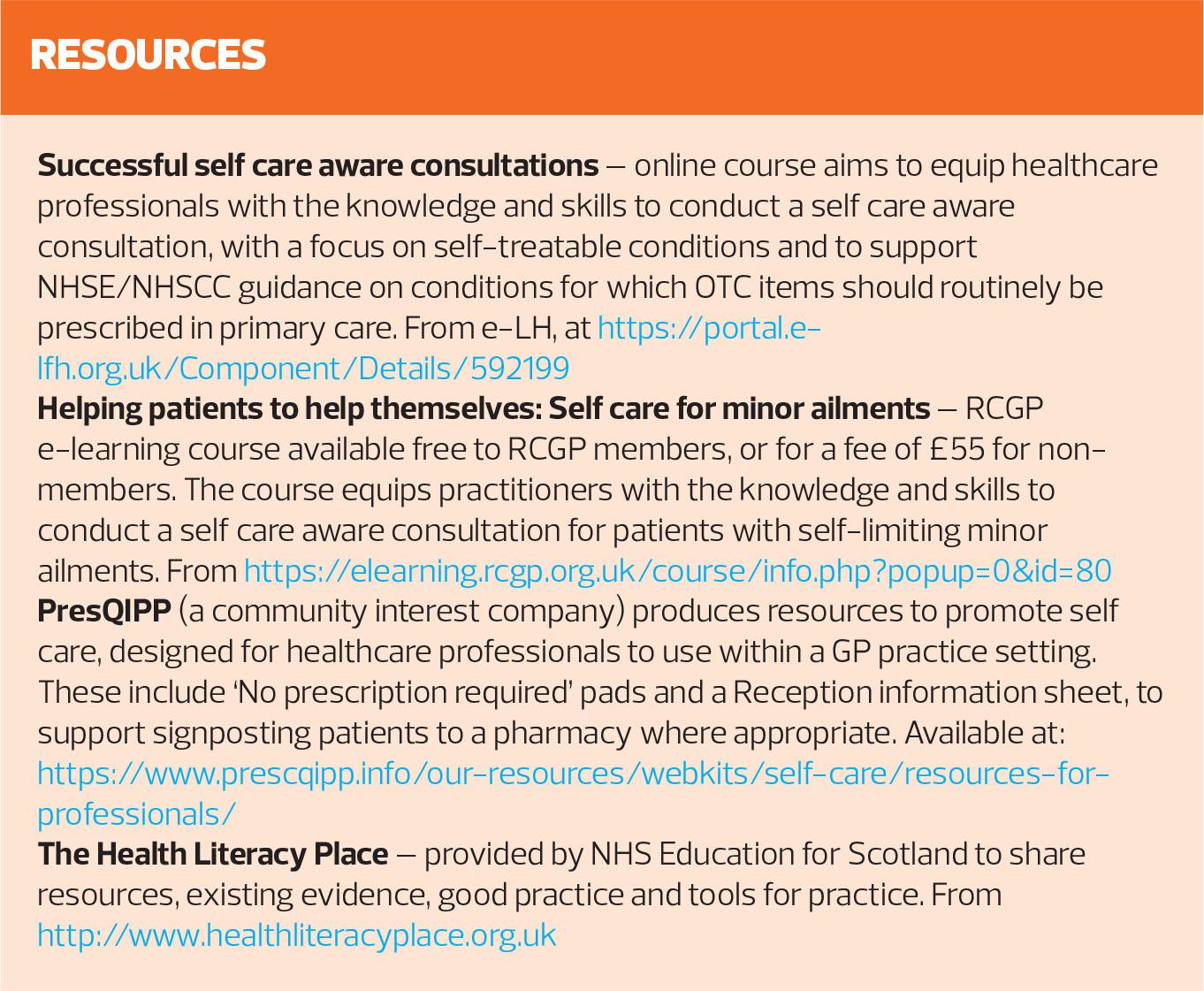
11. Health Education England. e-LfH. Successful Self Care Aware Consultations. https://portal.e-lfh.org.uk/Component/Details/592199
12. Self Care Forum. Top tips for practices in supporting self care. http://www.selfcareforum.org/getting-started/top-tips/
Related articles
View all Articles