Finding the right combination: choosing combination inhalers for asthma and COPD
Beverley Bostock-Cox
Beverley Bostock-Cox
RGN MSc QN
Nurse Practitioner Mann Cottage Surgery
Education Lead Education for Health
Inhaled therapies are the bedrock of pharmacological management of both asthma and COPD, and often two or more drugs will be used in a combination device to simplify treatment and aid concordance: but which should be used and how should you choose?
There are so many combination inhalers on the market that general practice nurses (GPNs) could be forgiven for feeling that they should just stick to a few that they know. However, the fact that there are so many options suggests that there is no inhaler which fits the bill for every individual and so nurses who are involved in supporting patients to choose the most appropriate device for them need to be aware of as many options as possible. In this article, the range of combination inhalers available will be discussed and a structured approach suggested to help GPNs decide, with their patients, the most suitable, individualised treatment aimed at achieving symptom relief and reduction in exacerbation risk.
By the end of this article you should be able to
- Recognise the current inhaled corticosteroid/long acting beta2 agonist (ICS/LABA) inhalers available
- Consider the key elements when choosing the most appropriate drugs for each patient
- Identify the delivery devices available for each combination
- Identify which combinations are licensed for each condition and age group
- Develop a structured approach to individualised care through the appropriate prescribing of combination inhalers
N.B. In the drug lists below, an alphabetical approach has been used in each section. Drugs and/or devices are not listed in order of preference.
PRESCRIBING – WHAT DOES THAT MEAN?
For the purpose of this article the term ‘prescribing’ will be used to include non-medical prescribers (NMPs) who sign their own prescriptions and GPNs who are suitably trained and competent in asthma and/or chronic obstructive pulmonary disease (COPD) management and who recommend medication which may be prescribed for the patient by others because the GPN is not a qualified NMP. Any review of a patient with asthma or COPD should include consideration of their current medication and should compare their treatment regimen with current best evidence. Even if the GPN carrying out the review cannot prescribe any medication, they should have a thorough understanding of the range of therapies available and be able to support patients with making the most appropriate choices. Furthermore, GPNs may be involved in reviewing patients who have been switched from one product to another (usually for cost purposes) and should understand the advantages and disadvantages of any switch and be able to advise the patient about these too.
Further information on the products described below can be found in their individual summary of product characteristics (SPCs) via the Electronic Medicines Compendium at www.medicines.org.uk/emc/, the British National Formulary at www.bnf.org and the MIMS website www.mims.co.uk.
THE ROLE OF COMBINATION THERAPIES IN ASTHMA
The British Thoracic Society/Scottish Intercollegiate Guidelines Network (BTS/SIGN) asthma update includes a treatment algorithm for both adults and children.1 Combination therapies are recommended for anyone over the age of five who is inadequately controlled on an ICS alone. Children age 5-12 can be prescribed an ICS/LABA combination if a very low dose ICS (200mcg total daily dose of a standard ICS or equivalent) has been helpful but the individual is still needing to use a reliever two-three times a week or more.1,2 For children over the age of 12 and adults, the initial dose of ICS would be a low total daily dose of 400mcg. Again, if the individual being treated has demonstrated a good response to the ICS but still needs to use a reliever two-three times a week or more, a combination would be indicated.1,2 All of the ICS molecules in combination therapies are anti-inflammatory and provide the cornerstone of asthma treatment.
THE ROLE OF COMBINATION THERAPIES IN COPD
In COPD, inhaled corticosteroids are only licensed to be given in combinations and should never be prescribed alone. The evidence for ICS therapy in COPD is in reducing exacerbations.3 The Evaluation of COPD Longitudinally to Identify Predictive Surrogate End-Points (ECLIPSE) study demonstrated that the best predictor of exacerbation risk was a previous history of recurrent exacerbations, i.e. twice a year or more.4 However, the latest guidelines from the Global Initiative for Obstructive Lung Disease (GOLD) have taken their lead from the FLAME study,5 and highlighted the use of dual bronchodilators in COPD for both symptom relief and reduction of exacerbations.6 Nonetheless, there is evidence for ICS/LABA inhalers for COPD patients who exacerbate (category C and D) and many GOLD category D patients will be on an ICS/LABA plus a LAMA as part of triple therapy. It is therefore important to be able to differentiate between the combination therapies when prescribing for COPD.
ICS USED IN COMBINATION THERAPIES
Inhaled corticosteroids used in the current range of combination therapies available are:
- Beclometasone dipropionate (BDP) (extra fine particle)
- Budesonide
- Fluticasone furoate
- Fluticasone propionate
Doses and dose equivalence
This is always a complex area as although it is possible to offer an approximate dose equivalence from one inhaled steroid molecule to another, the issue of equivalence is not as simple as that. For example, do we mean ‘equivalent dose to achieve the same benefits’ or ‘equivalent dose to cause side effects such as adrenal suppression’? BTS/SIGN has a list of combinations and their estimated dose equivalence here: https://www.brit-thoracic.org.uk/document-library/clinical-information/asthma/btssign-asthma-guideline-quick-reference-guide-2016/ (page 11). Put simply, using standard beclometasone (BDP) as the ‘norm’ (as found in, for example, Clenil®) the following adjustments can be made:
Beclometasone extra fine particle – 2.5 times the strength of standard beclometasone so 100mcg beclometasone extra fine particle = 250mcg standard beclometasone
Budesonide – no adjustment needed i.e. 400mcg is 400mcg
Fluticasone furoate – no direct comparison possible but BTS/SIGN suggests that 92mcg of fluticasone furoate is equivalent to a low/medium dose of ICS i.e. between 400-800mcg per puff.1 The GINA guidelines, however, have included it in the low dose category.2
Fluticasone propionate is two times the strength of standard beclometasone so 100mcg fluticasone propionate = 200mcg standard beclometasone
LABAs USED IN COMBINATION THERAPIES
- Formoterol
- Salmeterol
- Vilanterol
Formoterol and salmeterol both last for 12 hours and are often therefore taken twice daily. However, the SPCs of several formoterol-containing combinations (Duoresp, Fobumix and Symbicort) suggest that they may also be taken once daily for asthma if the patient is well controlled. Vilanterol is a once daily LABA.
Formoterol has a fast onset of action – within a few minutes – whereas salmeterol is far slower at around 30 minutes.7 Vilanterol sits between these two molecules at around 15 minutes.7
THE COMBINATIONS CURRENTLY AVAILABLE
There are eight combination therapies currently available. Some share the same ingredients albeit in slightly different doses and others are unique combinations.
- Beclometasone extra fine particle with formoterol (Fostair®)
- Budesonide with formoterol (Duoresp®, Fobumix®, Symbicort®)
- Fluticasone furoate with vilanterol (Relvar®)
- Fluticasone propionate with formoterol (Flutiform®)
- Fluticasone propionate with salmeterol (Aerivio®, Seretide®, Sirdupla®, Airflusal®)
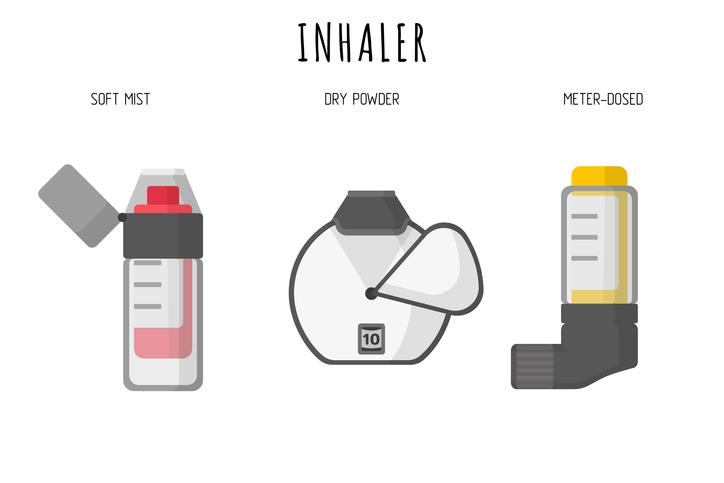
DEVICES
Although the choice of each drug is important (both the ICS and LABA) it could be argued that the device is at least as important. If the patient cannot use the device then the best drug combination in the world will have no effect. The combinations come in either a pMDI or a dry powder inhaler, so if a patient has a preference for one or the other, this may be the best place to start.
pMDIs
- pMDIs for asthma only: Flutiform®, Seretide®, Sirdupla®
- pMDIs for COPD only: Symbicort®
- pMDIs licensed for both asthma and COPD: Fostair®
Dry powder inhalers
- Aerivio Spiromax®
- Airflusal Forspiro®
- Duoresp Spiromax®
- Fobumix Easyhaler®
- Fostair NextHaler®
- Relvar Ellipta®
- Seretide Accuhaler®
- Symbicort Turbohaler®
These are all licensed for both asthma and COPD but doses may differ between the two conditions. The higher dose of Fostair pMDI and NextHaler at 200/6mcg and Relvar at 184/22mcg are both only licensed for asthma and are both high dose combinations that should normally only be used with specialist advice. With each product, care should be taken to stay within licence.
COMBINATIONS, AGE AND ASTHMA
Not all combinations are licensed to use in younger people. Appropriate inhalers as defined by licences for specific age groups are as follows:
Under 5s: Seretide pMDI is licensed from age 4 but BTS SIGN now gives preference to an ICS with a leukotriene receptor antagonist instead.1
From age 6: Symbicort Turbohaler is licensed from age 6 although an assessment should be made regarding the child’s ability to use the device before prescribing
From age 12: Flutiform and Relvar are both licensed for use in children age 12 and over
From age 18: all other combinations are licensed for age 18 and over
Once again, doses should be adjusted according to the age of the child and licence restrictions should be observed. For example, Flutiform is licensed to use from age 12 at the 50/5mcg and 125/5mcg dose but the 250/10mcg dose is licensed from age 18 only.
MAINTENANCE AND RELIEVER THERAPY REGIMENS
Maintenance and reliever therapy (MART) regimens may be suitable for people who prefer to have one inhaler to use for both their standard treatment and as reliever medication. Rather than using a combination plus a short acting beta2 agonist, they can have an extra inhalation of a combination that is licensed to be used in this way. Patients on MART regimens need to understand how to implement appropriately and not everyone will be suitable for MART.
Combinations licensed to use as MART
- Duoresp 160/4.5mcg 2-4 puffs daily plus prn up to a maximum of 12 puffs a day (age 18 and over)
- Fobumix 160/4.5mcg 1-2 puffs bd (or 2 puffs once daily) plus prn up to 12 puffs maximum in 24 hours (age 18 and over)
- Fostair 100/6mcg 1 puff bd plus prn up to a maximum of 8 puffs a day (age 18 and over)
- Symbicort 100/6mcg and 200/6mcg 2 puffs daily plus prn up to a maximum of 12 puffs a day (age 12 and over)
INFORMATION TO CONSIDER WHEN PRESCRIBING
In asthma the aim should be to offer the lowest effective dose of ICS with the requisite dose of LABA in order to optimise the risk:benefit ratio of the two drugs. However, not all low dose options (as defined by BTS/SIGN) are the same. A low dose of Flutiform (50/5mcg 2 puffs bd) offers 200mcg of fluticasone propionate (equivalent to 400mcg BDP) plus 10mcg of formoterol; a low dose of Fostair (100/6mcg 1 puff bd) offers 200mcg of extrafine BDP (equivalent to 500mcg standard BDP) plus 6mcg of formoterol. Whichever option is taken, the patient needs to be able to use the device correctly and both the drug and the device should be licensed for asthma and for the age of the individual being treated.
In COPD, age will not be an issue but again, if an ICS/LABA is indicated, the aim should be to offer the lowest effective dose of ICS in order to reduce any potential side effects. Seretide 500mcg bd delivers a total daily dose equivalence of 2000mcg BDP, whereas Symbicort offers 800mcg. Faster LABAs may also have the potential to give people symptom relief when they most need it – in the morning. As many people with COPD will be older and may have co-morbidities and issues with dexterity, it will be important to give due consideration to the device, too.
CASE STUDIES
So let’s consider these case studies and use the information above to help inform any decision as to which combination inhaler might fit best. All of the cases have a confirmed diagnosis and need stepping up to a combination inhaler.
- Alice is 5 years old and has been diagnosed with asthma 3 months ago.
- Brandon is 12 years old and has had asthma since he was 3. He plays a lot of sport.
- Cara is 28 years old and has recently been diagnosed with asthma.
- Dev is 74 years old and has COPD, GOLD category D.
Alice
Alice’s age means that she is likely to need her medication through a pMDI and spacer. The only combination licensed for this age group is Seretide so she would be given 50/25mcg 2 puffs bd giving her a total daily dose of 200mcg fluticasone propionate equivalent to 400mcg standard beclometasone – i.e. higher than the usual recommended dose of ICS for this age group. Seretide’s licence means that the pMDI must always be given as 2 puffs twice daily to ensure the full dose of salmeterol is given. Thus it might be better to try an LTRA with Clenil 50mcg 2 puffs bd (total daily dose 200mcg as per BTS/SIGN recommendations) before moving to a combination. However, if a combination is needed in a child of this age, Seretide remains the licensed option.
Brandon
Brandon has lots of options. He is on the adult guideline pathway at 12 years of age but not all combinations will be licensed for a 12 year old. If he wants a pMDI (to be used with a spacer or a Flo-tone device at home) he could have Seretide or Flutiform. Both are given at a dose of 2 puffs bd which would deliver a total daily dose of 200mcg fluticasone propionate equivalent to 400mcg standard BDP but Flutiform contains formoterol which has a faster onset of action than Seretide’s salmeterol,3 and Flutiform is the only combination which has been tested with the Flo-Tone device, too. If Brandon prefers a dry powder inhaler he can have Seretide Accuhaler (100mcg 1 puff bd), Symbicort 100/6 2 puffs bd (optimising both the dose of the ICS and the LABA), or Relvar 92/22mcg 1 puff daily. It would be important to check that he understands the importance of taking his combination inhaler as prescribed and with the correct technique to ensure optimal control so that exercise related symptoms are less likely to occur. Symbicort is licensed to be used as MART in the over 12s now so he could also have one inhaler (Turbohaler) for both treatment of his asthma and for symptom relief should this be needed. All of the other combinations are restricted to age 18 and over so would not be suitable for Brandon.
Cara
Cara is 28 years old and therefore has no restrictions on her asthma treatment. The only combinations that should not be prescribed are those that are licensed for COPD only – i.e. Symbicort pMDI. She needs to choose a device that suits her (pMDI versus DPI) and discuss any preference for once daily versus twice daily treatment. She might also want to consider a MART regimen. Cost issues may inform formularies and/or switches in practice and this may lead clinicians to opt for cheaper inhalers (e.g. Fobumix or Duoresp over Symbicort) but it is important to consider the differences between these delivery systems in terms of ease of use, taste, sensation and inspiratory flow/resistance. Any of these elements could be significant for each individual patient and no formulary can be expected to factor in the personal needs or preferences of each person that the GPN sees in the clinic setting.
Dev
Dev is a GOLD category D COPD patient and his clinician has decided that he needs an ICS/LABA. pMDIs that are licensed for COPD include Symbicort 200/6mcg 2 puffs bd and Fostair 100/6mcg 2 puffs bd. The total daily dose of budesonide in Symbicort is 800mcg; in Fostair the dose of extra fine beclometasone is 400mcg but this is equivalent to 1000mcg standard BDP, as 100mcg extra fine BDP is equal to 250mcg standard BDP. If Dev prefers a DPI, he can have Seretide 500mcg bd via the Accuhaler but this will deliver a dose of ICS equivalent to 2000mcg BDP. This is a very high dose of ICS and is unnecessary when lower doses of ICS will do the same job of preventing exacerbations without the inherent risk of higher doses.9, 10 The GPN and Dev should then consider whether the faster onset of action of formoterol is important. In COPD, patients may feel that they can get up and on with their day with the swift symptom relief from formoterol compared with the slower onset of vilanterol in Relvar and the slower still action of salmeterol in Seretide. Thus Dev could have Symbicort Turbohaler 400/12mcg 1 puff bd or Fobumix 320/9mcg bd or Duoresp 320/9mcg bd which will deliver a lower dose of ICS with a full dose of LABA. Fostair NextHaler delivers the equivalent of 1000mcg total daily dose with formoterol as its LABA and Relvar 92/22mcg is also a possibility as a once daily option delivering a low/medium dose of ICS with vilanterol. Again, some patients might prefer the simplicity of a once daily inhaler, while others will feel more confident with a twice-daily treatment. If Dev needs triple therapy it is also worth remembering that the Ellipta device has an ICS/LABA (Relvar) and a long acting muscarinic antagonist (Incruse – umeclidinium) allowing triple therapy to be given in the same device with one puff once daily for each. Triple therapy in one device is coming soon.
IN SUMMARY
Working out which combination is most appropriate for each patient involves consideration of the licence and the individual needs of the patient. It is important to make sure the device is licensed for the condition being treated and that any treatment is appropriate for the age of the patient if they have asthma. The clinician should take into account whether the patient prefers a pMDI and spacer/Flo-Tone or a DPI. Consideration might be given as to whether the faster onset of action of formoterol is important and if so, focus on combinations which contain this LABA. If a once daily option is preferred by the patient then Relvar may be the one to choose although Duoresp, Fobumix and Symbicort can all be given once daily according to their SPCs. Amongst all of the different drug and device combinations there is likely to be at least one that is the right fit for any patient. The most suitable treatment can therefore be identified through collaboration between the healthcare professional and the patient, where the clinician is the expert in the treatment options and the patient is the expert in his or her self.
REFERENCES
1. British Thoracic Society/Scottish Intercollegiate Guidelines Network (2016) British guideline on the management of asthma https://www.brit-thoracic.org.uk/document-library/clinical-information/asthma/btssign-asthma-guideline-2016/
2. GINA. Global Strategy for asthma management and prevention, 2017
http://ginasthma.org/2017-gina-report-global-strategy-for-asthma-management-and-prevention/
3. Ernst P, Saad N, Suissa S. Inhaled corticosteroids in COPD European Respiratory Journal 2015;45: 525-537
4. Agusti A, Calverley PM, Celli B, et al (2010) Characterisation of COPD heterogeneity in the ECLIPSE cohort. Respir Res. 11:122.
5. Wedzicha JA, et al. Indacaterol–Glycopyrronium versus Salmeterol–Fluticasone for COPD N Engl J Med 2016;374:2222-2234
6. Global Initiative for Obstructive Lung Disease COPD guidelines, 2017 www.goldcopd.org
7. Bodzenta-Lukaszyk A, et al. Fluticasone/formoterol combination therapy is as effective as fluticasone/salmeterol in the treatment of asthma, but has a more rapid onset of action: an open-label, randomized study BMC Pulm Med 2011;11: 28 https://bmcpulmmed.biomedcentral.com/articles/10.1186/1471-2466-11-28
8. Cazzola M, Beeh KM, Price D, Roche N. Assessing the clinical value of fast onset and sustained duration of action of long-acting bronchodilators for COPD. Pulm Pharmacol Ther 2015;31:68–78
9. Crim C, Calverley PM, Anderson JA, et al. Pneumonia risk in COPD patients receiving inhaled corticosteroids alone or in combination: TORCH study results. Eur Respir J 2009;34(3):641–647
10. Ernst P, Saad N, Suissa S. Inhaled corticosteroids in COPD European Respiratory Journal 2015;45:525-537
Related articles
View all Articles