The challenge of changing perceptions of practice nursing
Monica Horton
Monica Horton
RGN BSc (Hons) Nursing Practice
Hardwicke House Group Practice, Sudbury
Making general practice nursing a first destination career is a cornerstone of official plans to overcome current shortages of practice nurses. It can still be difficult for newly or recently qualified nurses to enter general practice but it can be done – with hugely positive results
Practice nursing has long been regarded as a ‘step down’ for older nurses, a pathway suitable for those wanting to escape the stresses of acute nursing with fewer working hours and a more sociable work pattern.
We are part of an ageing workforce, with more nurses approaching retirement and fewer nurses coming into general practice to replace them. The Queens Nursing institute survey in 2015 found that 30% of general practice nurses were due to retire by this year.1 A National Audit Office report this month (March 2020) found that 35% of nurses in primary care were aged 55 years or older, and only 1% are under 25.2
Practice nursing has changed radically, especially in the last two decades which have seen general practice nurses assume autonomous management of long term conditions and sexual health, the development of advanced practitioner and nurse practitioner roles, and increasing numbers of nurses qualifying as independent prescribers. The role has changed and perceptions of the general practice nurse need to change with it.
While the role has developed, there is still very little to encourage newly or recently qualified nurses to consider practice nursing as a possible career path, despite publication in 2017 of the General Practice Nursing Workforce Development Plan,3 which was developed to raise the profile of general practice nursing and promote general practice as a first destination career.
Our practice is an example of how, with the direction and support of a forward-thinking practice manager, we are achieving the aims of the development plan.
NEW RECRUITS
In the past 12 months, our busy five-branch practice has employed a relatively newly qualified nurse and a nurse direct from her training. Despite concerns from some of the practice staff, and in contradiction of our own practice nurse job description, these two nurses became the newest members of our nursing team, and what a difference they have made! Both came with fresh, creative ideas, enthusiasm, outstanding attitudes and expert digital knowledge. Becoming catalysts for the nursing team they complemented the more experienced nurses. Sharing our knowledge and experience with their more modern viewpoints and skills has helped reform our practice, made us think differently, and prepared us for future changes.
Laura Bird, newly qualified, has initiated a plan to be the first practice in our CCG to take nursing students. Collaborating with the CCG Primary Care Educator Lead, she has arranged assessor and supervisor training for the team. Driven by her own ambition to become a practice nurse immediately post-qualification, she is opening doors for other newly qualified nurses. As a student, she spent one week working with a practice nurse, a friend of the family. Not a placement, but an opportunity she arranged for herself. This gave her a ‘glimpse’ of general practice nursing and she was amazed by the experience. From that time, she was focused on becoming a practice nurse. As a student, Laura was an RCN student committee member conveying her passion to follow a pathway into general practice and ignoring barriers and obstacles put in her way. Now as a qualified nurse, she has been asked to become an ambassador for the General Practice Nursing Student Nurse Network, visiting universities to promote general practice and leading the vision through social media, engaging student nurses and building positive perceptions of a career in primary care.
Her passion has led to the nursing team planning for students with enthusiasm and excitement. Giving students a positive and rewarding placement will provide more than a ‘glimpse’ and may provide the spark needed to lead them into general practice nursing.
Shelbey Mahon, qualified for two years, had worked on a surgical ward but had become disheartened by the pressures of acute hospital nursing. Throughout her training, practice nursing was never suggested as a possible career path and there was no education about what it involved and certainly no placement opportunity.
Applying for the job, she was told ‘you will never get it’ and ‘won’t it be a bit boring?’ from colleagues. Given a chance to become a practice nurse, she has flourished in primary care. Shelbey has sailed through the basic training and is already working towards her second chronic disease diploma.
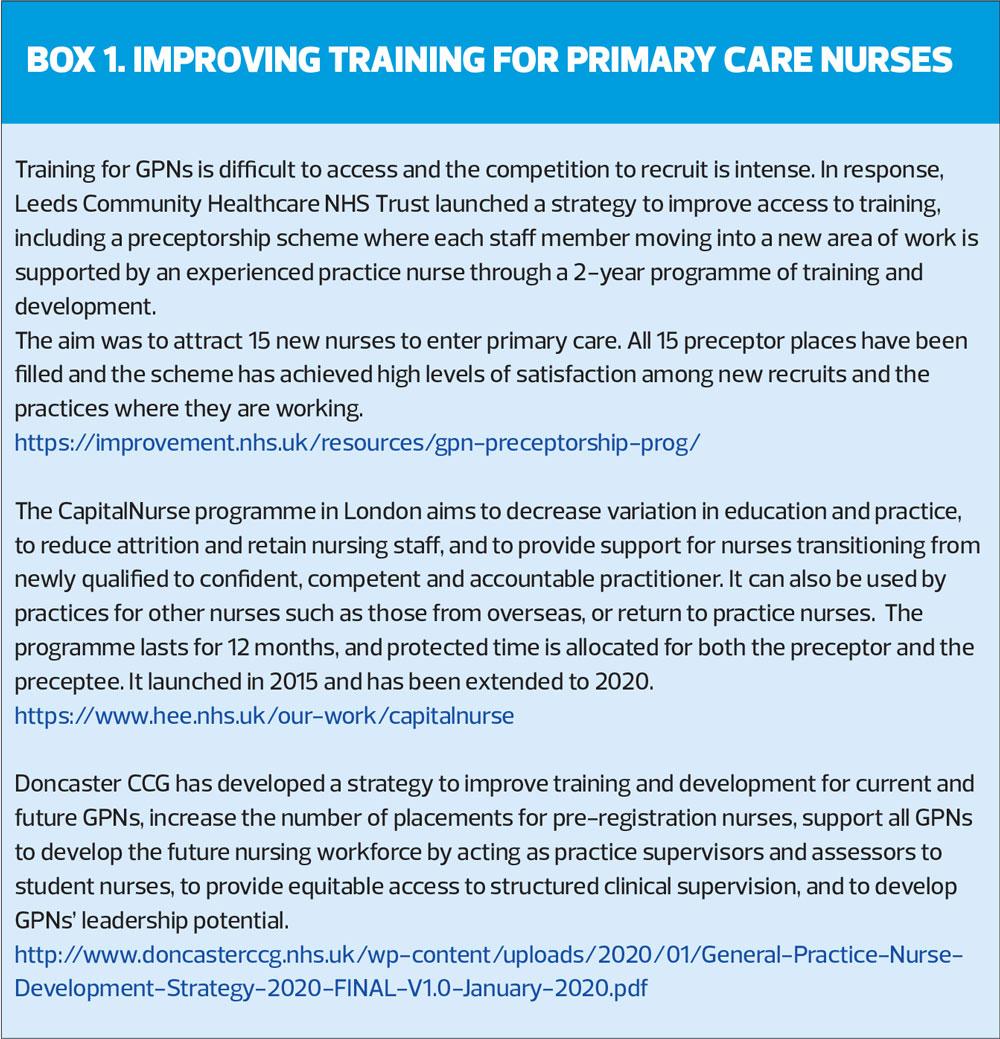
In addition, she has developed a preceptorship programme for newly qualified nurses coming into general practice nursing and is working with the CCG Primary Care Educator Lead to develop a preceptorship guide to be used across general practice. As part of the accompanying workbook, she has devised a medicines management assessment tool, specific to primary care. This workbook will allow easier progression from student to general practice nurse. (For examples of how this has been done elsewhere, see Box 1).
POSITIVE VISION
These pro-active ideas to enhance training and encourage students into primary care have earned both nurses praise from the CCG education team. The nurses’ desire to share their experiences and encourage others into general practice nursing is a demonstration of their positivity and vision for the future NHS.
Both nurses are ‘digital natives’ and have excellent computer skills, which they have used – working closely with the more experienced practice nurses – to carry out audits. Measles, mumps and rubella (MMR), flu and pneumonia vaccination figures have been identified and used to find ways to encourage uptake. Searches on diabetic and pre-diabetic patients have prompted letters to support prevention programmes and identify patients needing further review. Using QOF and Eclipse data (NHS pathways) care processes needing more attention have been identified; as an example, we have sent letters to patients inviting them in to encourage statin use. Previously slow processes have been sped up by their competent and expert help. Nursing knowledge and experience is now more connected to the business side of general practice, taking the nursing team from the treatment room into the sphere of management with the ultimate aim of improving patient outcomes.
The advantages to the practice have been demonstrated. But what about the nurses? Both have found a career path that they love and want to succeed in. Not wanting to work in acute hospital settings, where would they have been if not employed by our practice? Facing friction and negativity in their choice to pursue a career as a general practice nurse they could have chosen other paths or left nursing altogether. Thank goodness for their determination and perseverance. I have no doubt both will become excellent, experienced general practice nurses and continue to excel.
CONCLUSION
Our nurse team is a mix of full and part time nurses, experienced nurses and those new to practice. The dynamics and drive of our team has been enhanced by the addition of newly qualified nurses. The theory of reform has been put into practice and our nursing team is proof that it can work. General practices need to create an environment where recruitment of newly qualified nurses is encouraged, out-dated job descriptions are revamped, and consideration of applicants is open minded to those with no or minimum experience. Our practice is proud to be an advocate for the employment of newly or recently qualified nurses into general practice and proud to be changing the perceptions of what a general practice nurse is.
REFERENCES
1. Queens’s Nursing Institute. General practice nursing in the 21st century. A time of opportunity: 2015. https://www.qni.org.uk/wp-content/uploads/2016/09/gpn_c21_report.pdf
2. National Audit Office. The NHS Nursing Workforce; 5 March 2020. https://www.nao.org.uk/wp-content/uploads/2020/03/The-NHS-nursing-workforce.pdf
3. Health Education England. The General Practice Nursing Workforce Development Plan; 2017. https://www.hee.nhs.uk/our-work/general-practice-nursing
Related articles
View all Articles