Medication errors
DIANE BAYLIS
DIANE BAYLIS
Risk and Education Manager, Medical Protection
Prescribing is the most common therapeutic intervention in general practice, but can also be a significant cause of unintended harm
Medication errors are a complex safety issue in primary care and the related failures can lead to avoidable patient harm and medicolegal action. Medication errors account for approximately 20% of Medical Protection general practice claims.
A recent review commissioned by the Department of Health and Social Care (DHSC) estimated that 66 million potentially clinically significant medication errors occur each year in the NHS and 71% of those occur in primary care.1 It also estimated that avoidable adverse drug reactions in primary care that lead to hospital admissions result in 627 deaths a year, with a cost of £83.7 million each year.
As a result, a new system for tracing prescribing errors was introduced last year. It links general practice prescribing data with hospital admissions data to enable the NHS to monitor and understand if a medication error was the likely cause of a patient being admitted to hospital.
NATIONAL REPORTING AND LEARNING SERVICE
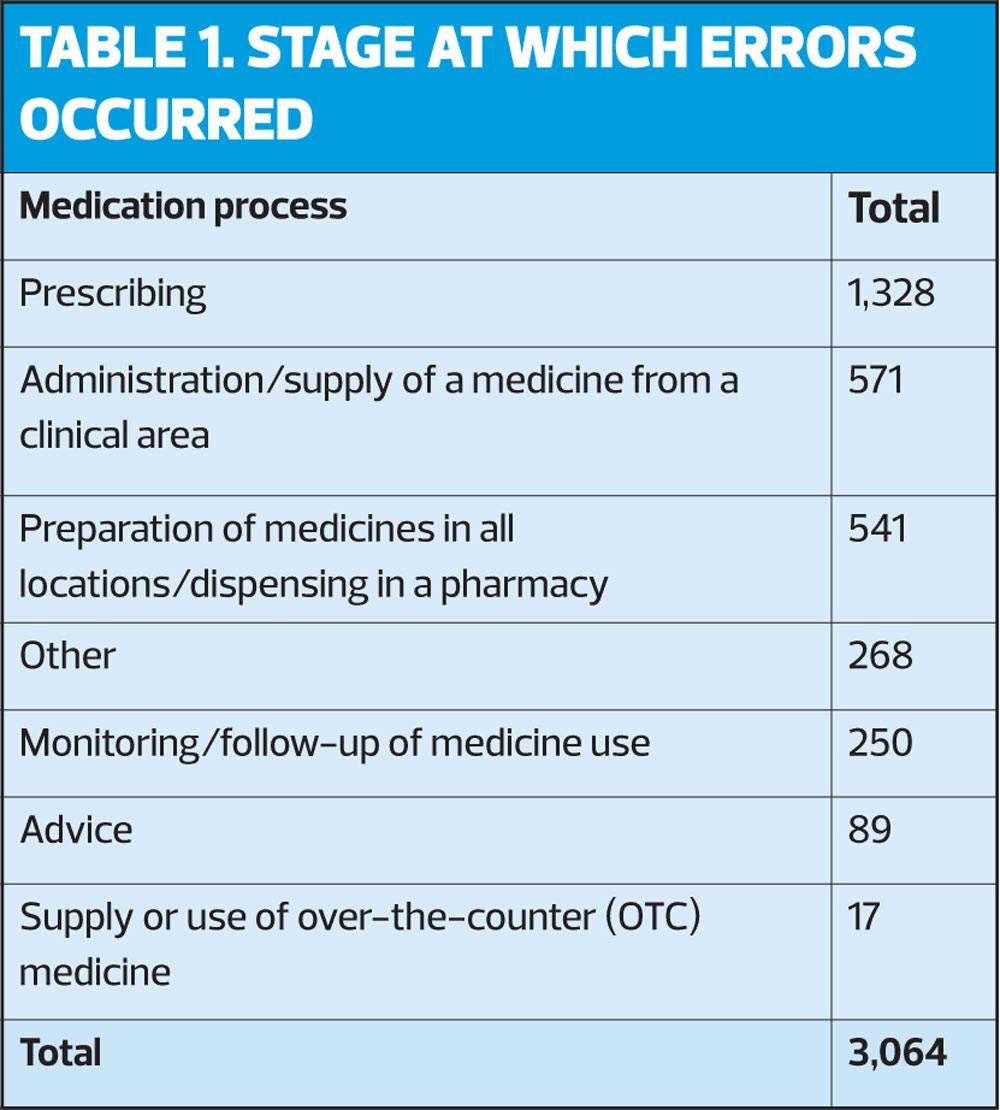
Data from the National Reporting and Learning Service (NRLS)2 for medication-related incidents reported to have occurred in general practice from 01 March 2017–28 February 2018 revealed 3,064 incidents, of which 2,810 caused no or low harm, and 1.14% caused death or severe harm. The largest proportion (43.3%) of reported medication-related incidents occurred at the prescribing stage (Table 1).
The top five errors occurring at the prescribing stage were:
1. Wrong/unclear dose or strength
2. Wrong drug/medicine
3. Contraindications to the use of the medicine in relation to drugs or conditions
4. Mismatching between patient and medicine
5. Wrong quantity
WHY DO THINGS GO WRONG?
The most common causes of prescribing errors are:3,4
- Lack of knowledge about patient or drug
- Poor communication
- Not following best practice and/or prescriber not keeping up-to-date
- Failing to review treatment
- Prescription generation, e.g.
– Calculations
– Abbreviations
– Similar sounding and/or looking.
PRACTICAL WAYS TO PRESCRIBE MORE SAFELY
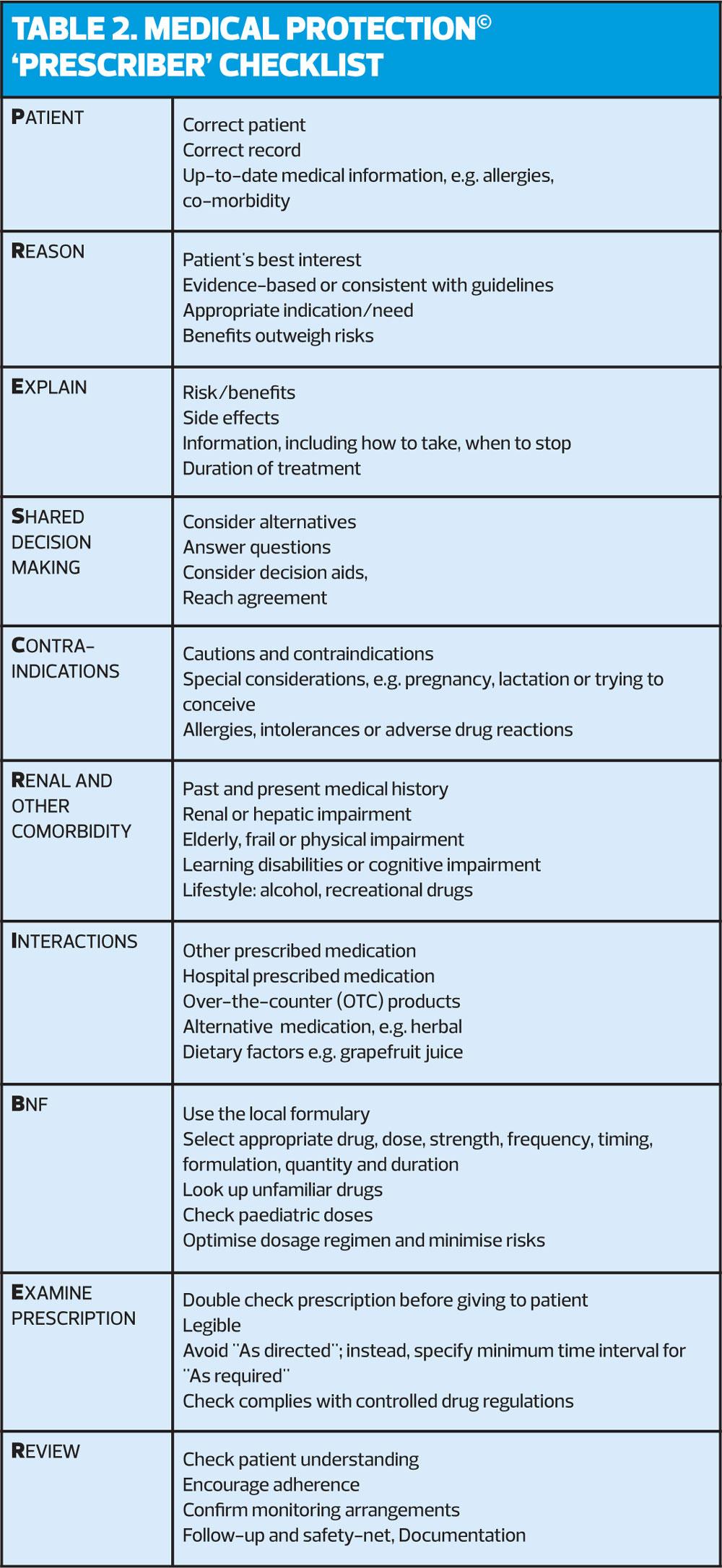
Checklists are a simple way to enhance safety and reduce the risk of medication errors and harm to patients. Medical Protection developed a simple checklist – PRESCRIBER© (Table 2, overleaf) – which can be used in routine practice.
IN SUMMARY
Medication errors are common and it is estimated that a large amount of potentially clinically significant medication errors occur each year in the NHS, with a substantial percentage of those occurring in primary care.1
An awareness of the interactions between people and elements of the repeat prescribing system will enable clinicians to better understand why things go wrong. Practices should focus on improving the design of their systems. The people who work in these systems are best placed to understand the complex interactions between patients and work tasks, processes, technology and the wider environment. Using a simple checklist may assist nurses to prescribe safely, reducing the risk of medication errors and harm to patients.
REFERENCES
1. Elliott R et al (2018). Prevalence and Economic Burden of Medication Errors in The NHS in England. http://www.eepru.org.uk/wp-content/uploads/2018/02/eepru-report-medication-error-feb-2018.pdf
2. National Reporting and Learning Service. Patient safety incident reports.
https://improvement.nhs.uk/resources/national-quarterly-data-patient-safety-incident-reports/
3. Department of Health. Building a safer NHS for patients improving medication safety, 2004:
4. Royal Pharmaceutical Society. A Competency Framework for all Prescribers, July 2016
https://www.nice.org.uk/news/article/new-competency-framework-for-all-prescribers
Related articles
View all Articles