You too can be a digital practice nurse champion
RUTH CHAMBERS
RUTH CHAMBERS
MD, FRCGP, OBE
Clinical Chair of Stoke-on-Trent CCG & Staffordshire STP’s clinical lead for technology enabled care services, digital workstream; Honorary professor at Staffordshire University and Keele University.
ANN HUGHES
RGN, Critical care diploma
Clinical telehealth facilitator Staffordshire, GPN Tean & Blythe Bridge practices, special interest LTCs management
PAUL BEANEY
BA
Second year Medical Student, Keel University
MARC SCHMID
Director of Redmoor Health, social enterprise
Among the aims of the Ten Point Action Plan for general practice nursing was to develop ‘digital nurse champions’ to expand and support the use of digital technologies in patient care. The due date for this work was April 2018, so what has been happening and what does it all mean?
Developing confidence, capability and capacity in the general practice nursing workforce is vital if individual practice nurses and teams are to cope with the challenges ahead from the ever increasing number of people with long term conditions (LTCs), and greater public expectations of general practices and the NHS in general. Practice nurses need to be able to work more efficiently and productively and help to minimise demand by encouraging patients to take more responsibility for the care of their own health condition(s), by enabling their self care and agreeing shared management plans.
Technology enabled care services (TECS) have got to be the answer. Great examples are springing up across health and care settings, such as telehealth for medication reminders and adherence, video consultation for asthma reviews, and closed Facebook groups for invited patients focused on a clinical purpose. These reduce clinician workload and support greater efficiency across the whole system. But adoption of TECS at scale in a general practice or across treatment pathways is a complex process. So we need to identify barriers that impede the deployment of technology by practice nurses for the many opportunities that there are for digital delivery of care and overcome such challenges to speed dissemination and adoption of TECS.1
So to achieve this digital transformation in general practice TECS we need to:
- Shift towards digital delivery being usual care – via use of Patient Online, Online Consultation triage, and make a range of apps, Facebook, telehealth and videoconsultation available – in every practice
- Involve general practice nurses and all practice staff at every level to ensure that such change works in practice
- Use TECS that are affordable and doable – in relation to equipment, staff training, WiFi connectivity, computer infrastructure, sharing of patient records and staff confidence, capability and capacity (3 ‘Cs’).2
WHAT IT MEANS TO BECOME A DIGITAL NURSE
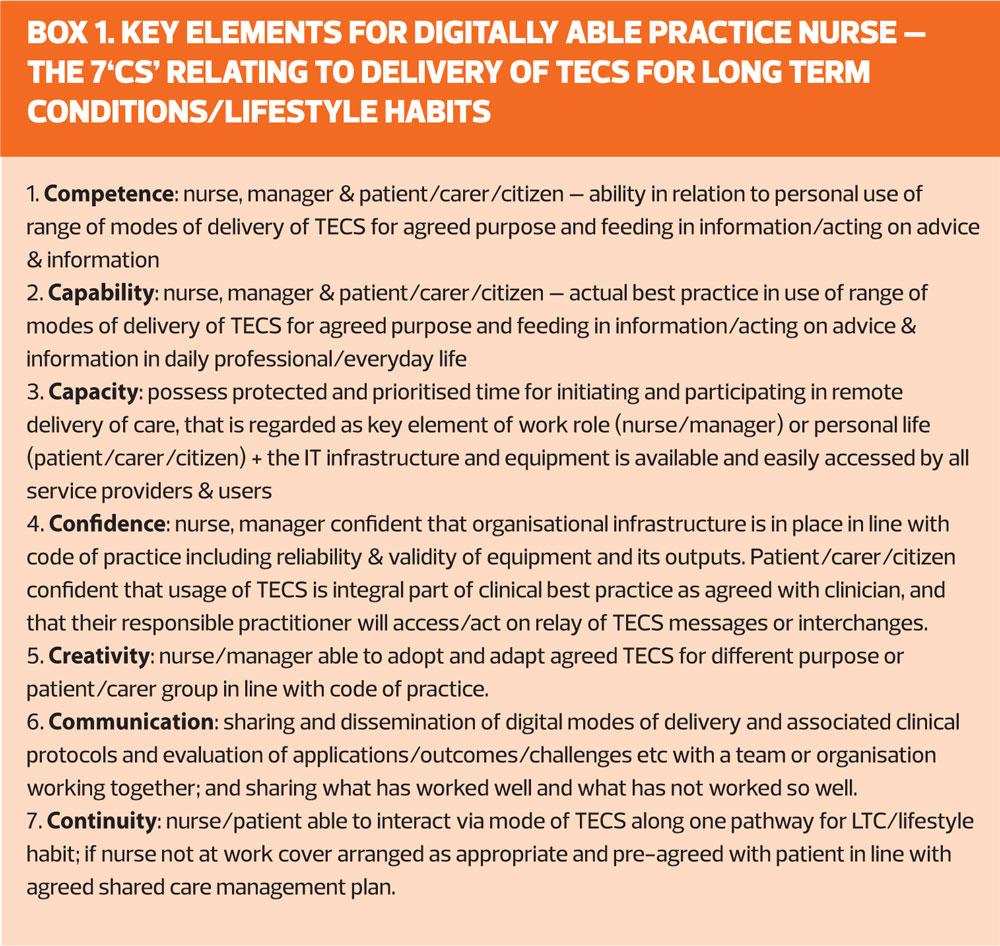
We shouldn’t expect that a practice nurse would immediately be able to pick up on how to use new technology and be enthusiastic about doing so. For individual practice nurses these three ‘Cs’ need to be widened to the following seven ‘Cs’ as in Box 1.3 This fits with Health Education England’s (HEE’s) General Practice Nursing (GPN) Workforce Development Plan to maximise the professional development of the workforce and ‘respond to the population’s health needs in the 21st century.’4 The Ten Point Action Plan for GPNs specifically included the evolution of digital nurse champions (by April 2018) and improved health literacy.5 HEE’s and the Royal College of Nursing (RCN) guide to Improving Digital Literacy6 builds on the RCN’s ‘every nurse an e-nurse’ vision and the NHSE’s plan to build a digital ready workforce.
And it is not just about being competent to use or set up TECS. Nurses need to understand the extent and purpose for which technology can be applied. They must become increasingly aware of what the range of modes of TECS is capable of and how this can enhance clinical practice at scale, whilst at the same understanding the limitations and governance requirement. Benner’s novice to expert model sums this up well in which she identified five levels of proficiency:
1. Novice
2. Advanced beginner
3. Competent
4. Proficient
5. Expert7
Benner used this model to define levels of skill acquisition in nursing practice that can be individualised for the adoption of TECS in everyday practice:
Novice: The novice nurse has no background understanding of the types or use of technology for healthcare.
Advanced beginner: The advanced beginner nurse has enough background experience to recognise aspects of a situation for which TECS might be used.
Competent: The competent nurse has considerable conscious, deliberate understanding and is able to use one or more modes of digital delivery of care effectively for example, for patients with long term respiratory conditions.
Proficient: The proficient nurse has an intuitive grasp of TECS based upon a deep background understanding of the range of TECS and how it can be delivered by themselves and team members in efficient, effective and productive ways.
Expert: The expert nurse tests and refines theoretical and practical knowledge in actual clinical situations, having a deep background understanding of clinical situations based upon many past paradigm cases.
DIGITAL EXPERIENCE AND EXPECTATIONS
With pilot funding from NHSE Nurse Transformation, we have introduced action learning for practice nurses across Staffordshire in relation to digital delivery of care. In terms of who is the ideal nurse to become a digital nurse, it seems that there are few pre-requisites, as the makeup of the programme’s participants neatly illustrates.
Perhaps surprisingly, having little prior experience with technology was not a barrier, as nearly all of the 27 practice nurses who have enrolled in a three-session learning set reported at the first session that they had ‘Never’ used TECS in their current practice. This is perhaps to be expected, given that the shift to using technology in primary healthcare settings is still in its infancy. Neither was having low confidence about the incorporation of TECS in their practice prohibitive; despite being able to see the benefits of TECS, almost half felt ‘Worried’ and ‘Nervous’ about adapting to the changes that it brings.
So, if neither negligible prior experience with, nor low confidence were obstructive, what factors might predict of who is likely to put themselves forward as practice nurse pioneers of digital healthcare? Aside from being a general practice nurse (GPN), the common positive associations with TECS that the participants shared were evident in their aspirations and expectations about what they would be able to achieve and what the programme could deliver. The majority reported that if TECS were implemented more widely then this would make a ‘large, positive contribution’ to improving self-management of LTCs in the community. Furthermore, the same number felt either ‘confident’ or ‘very confident’ that they could share knowledge with colleagues to help them adopt TECS in the care they provide to their patients. Underpinning these attitudes is the view that all of the nurse cohorts strongly agreed with, that they ‘can see the benefit of using technology enabled health services for both patients and colleagues’.
So while these nurses had negligible experience with TECS in their roles they were nonetheless enthusiastic and optimistic about the role and benefits of it for the future of primary and community healthcare. Furthermore, in spite of uncertainty about their confidence in using digital technology in their practice, the nurses were confident in their ability to share knowledge of TECS with their colleagues. Therefore, it seems that what is essential to becoming a digital nurse is being able to see past one’s immediate doubts and inexperience, to the opportunities that TECS can deliver if brought to patients at the grassroots level. The nurses created individual action plans for how they wanted to bolster the care they provide and who they can see gaining the most from it. Whether it be patients who are housebound, or those with specific LTCs such as hypertension, atrial fibrillation or diabetes, they decided to make use of available technology to make a difference to their patients’ lives.
DIGITAL DELIVERY OF CARE
We need a change of emphasis in the NHS so that we really do provide patient-centric care. Helping a patient to understand more about their condition from accessing their medical records via Patient Online should help them to understand their health condition better and be more prepared to discuss their health and wellbeing when consulting their GP and/or practice nurse and more likely to agree and adhere to a shared care plan going forwards.
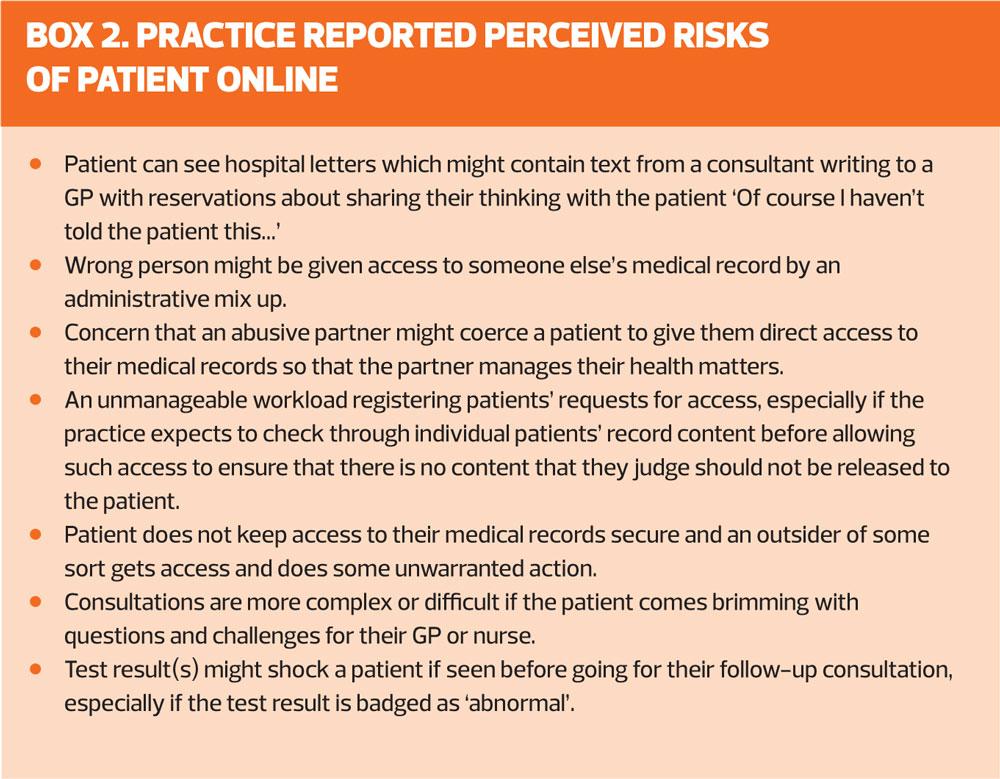
One good reason why a practice nurse would recommend a patient to access their records is to see their test results. General practice teams are gradually getting behind Patient Online as the current number of patients in England – 14 million – already signed up to it shows. Practices tend to differ in the extent to which they enable or permit access to hospital letters or test results. Some practice nurses and GPs focus on the perceived risks rather than the obvious benefits of being able to book appointments, order repeat prescriptions and access their own records – see Box 2.
So practice nurses should realise that these perceived risks are the typical reactions of NHS staff when presented with change. Many of these potential risks will be overcome by:
- The patient being prepared and supported to use Patient Online – maybe the Practice Participation Group can take a lead and help?
- The practice team optimising access to Patient Online and promoting it via NHSE resources – posters, display stand, newsletter – see www.england.nhs.uk/materialsforpatient
- Reviewing any concerns or issues at practice meetings (three-monthly) to revise how the practice operates the Patient Online service, and improving approach.
PRACTICE NURSE FOCUS
Digital technology, in all its forms has made a huge impact on the way that health professionals approach managing LTCs such as asthma and COPD. All the modes of technology available are interchangeable, and can be used alongside each other, or as stand alone ways of delivery of care.
For example nurses are now able to recommend patient focused apps such as those relating to stop smoking or asthma support (e.g. Manage Your Health app which is freely available on the Google play, Apple and Amazon App stores or see www.clinitecs.uk for more information) that appeal to both young and old – especially with the avatar animation demonstrating how to use different types of inhalers. This results in reinforcement of standardised management advice given during an annual asthma review often avoiding the patient slipping into bad habits such as incorrect inhaler technique or inappropriate use of medication.
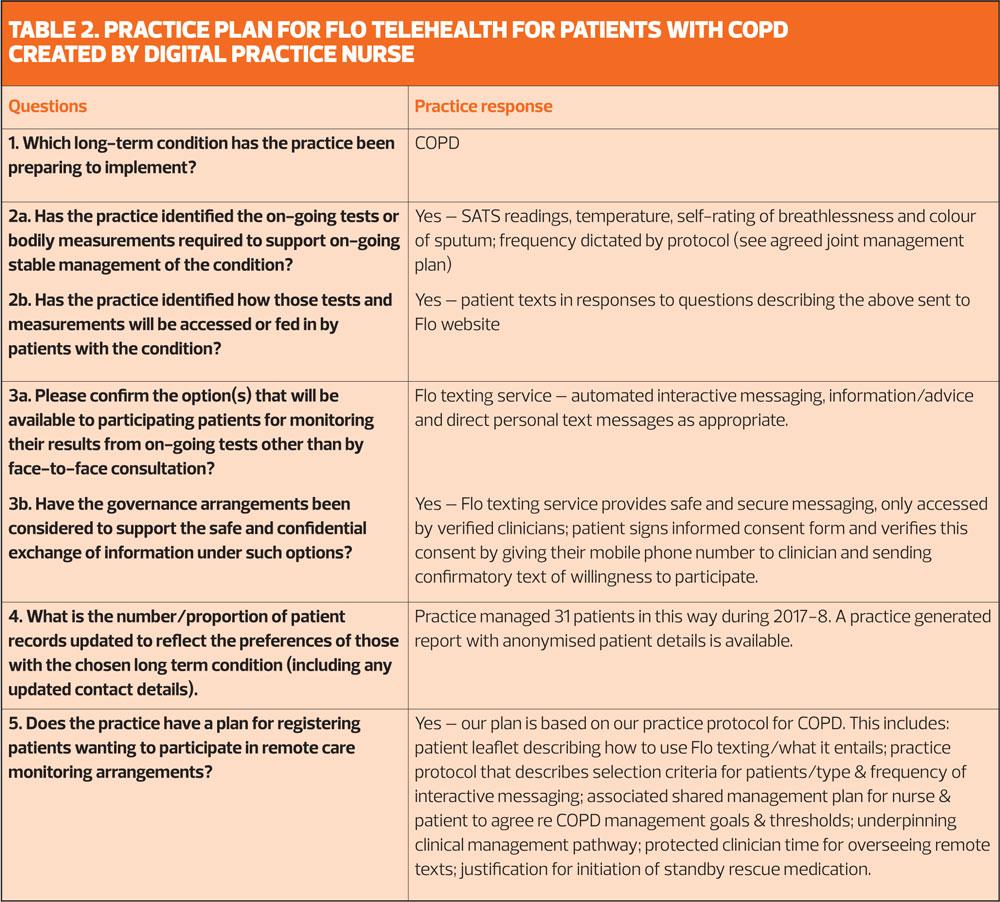
It can be beneficial to introduce the use of telehealth as a simple interactive texting service that requires only basic equipment and minimal knowledge of technology, to send text reminders to prompt the patient to use their inhaler on a regular basis. Table 2 describes how a practice team might plan to use Florence (Flo) telehealth for patients with COPD. Flo telehealth has been recognised nationally as one of ten selected innovations that have ‘helped change the face of healthcare.’8 See www.simple.uk.net or www.clinitecs.uk for more information about Flo telehealth or look at clinicians’ case studies.9
With the ever increasing pressures to avoid unnecessary hospital admissions, technology provides practice nurses with tools to support excellent patient centred care which is often all that is needed to prevent exacerbation and possible need to attend emergency portals.
COPD patients are usually on a variety of medications to manage their condition including ‘rescue medication’ for use at home during an exacerbation. Patients typically have a COPD self-management plan, agreed with their clinician, advising them what action and/ or medication to take, according to their symptoms. Delay in identifying exacerbations and taking action, including using the correct rescue medication, can lead to emergency admission that might have been avoided with rapid treatment. As a consequence, patients often need to be seen in the primary care setting to have checks and to review their treatment along with seeking reassurance and advice. These visits can often be difficult for patients as their poor breathing can lead to reduced mobility and having to sit in waiting rooms can expose patients to the risk of further infection. Flo telehealth can be a valuable tool to help patients with COPD self-manage at home and can reduce the need for as many surgery visits if the patient’s texted responses trigger advice to take standby medication without delay, improves their compliance with medication, reduces overall anxiety and ultimately avoids hospital attendances or admissions.9,10
CONCLUSION
So rather than seeing digital modes of delivery of care as a threat and burden on their time, practice nurses should see TECS as an opportunity to meet the changing needs and expectations of patients. Using Flo telehealth or video consultation for annual LTC reviews in well patients for instance, will enhance engagement as they are more likely to participate with these types of convenient care. Patients’ use of nurse recommended apps or being invited members of focused Closed Facebook Groups such as for diabetes or weight management should enhance adherence to medication and other interventions as patients understand their condition better – making practice nurses’ work easier and more fulfilling.
REFERENCES
1. Chambers R and Schmid M. Making technology-enabled health care work in general practice. Br J Gen Pract 2018; 68 (668): 108-109. DOI:https;//doi.org/10.3399/bjgp18X694877
2. The Queen’s Nursing Institute. Nursing in the Digital Age. Using technology to support patients in the home. London, The Queen’s Nursing Institute, 2018.
3.Chambers R, Schmid M, Al Jabbouri A, Beaney P. Making Digital Healthcare Happen in Practice. A practical handbook. Oxford, Otmoor Publishing, 2018.
4.Health Education England (HEE). The General Practice Nursing Workforce Development Plan. London, HEE, 2017.
5. NHSE. General Practice – Developing confidence, capability and capacity. A ten point action plan for General Practice Nursing. London, NHSE, 2017.
6. Health Education England (HEE) and Royal College of Nursing (RCN). Improving Digital Literacy. London, RCN 2017 (RCN publication code: 006 129).
7. Benner P (1984) From Novice to Expert: excellence and power in clinical nursing practice. Addison Wesley, California.
8.The Health Foundation. Against the Odds: Successfully scaling innovation in the NHS. London, The Health Foundation, 2018.
9. Hughes A. COPD patient avoids A&E and acute admissions through self-management with FLO http://www.simple.uk.net/home/casestudies/casestudiescontent/copd-patient-avoids-a-e-and-acute-admissions-through-self-management-with-flo
10. Collis L, Whitmore M, Chambers R. Telehealth in primary care: what’s in it for me? Practice Nursing 2014; 25 (8): 406-8.
Related articles
View all Articles