Caring for carers
Katherine Ellerby
Katherine Ellerby
RGN, RM, BSc (Hons)
Non-medical independent prescriber, NDFSRH
Practice Nurse, Framlingham Medical Practice, Suffolk & Clinical Research Nurse, Suffolk Primary Care
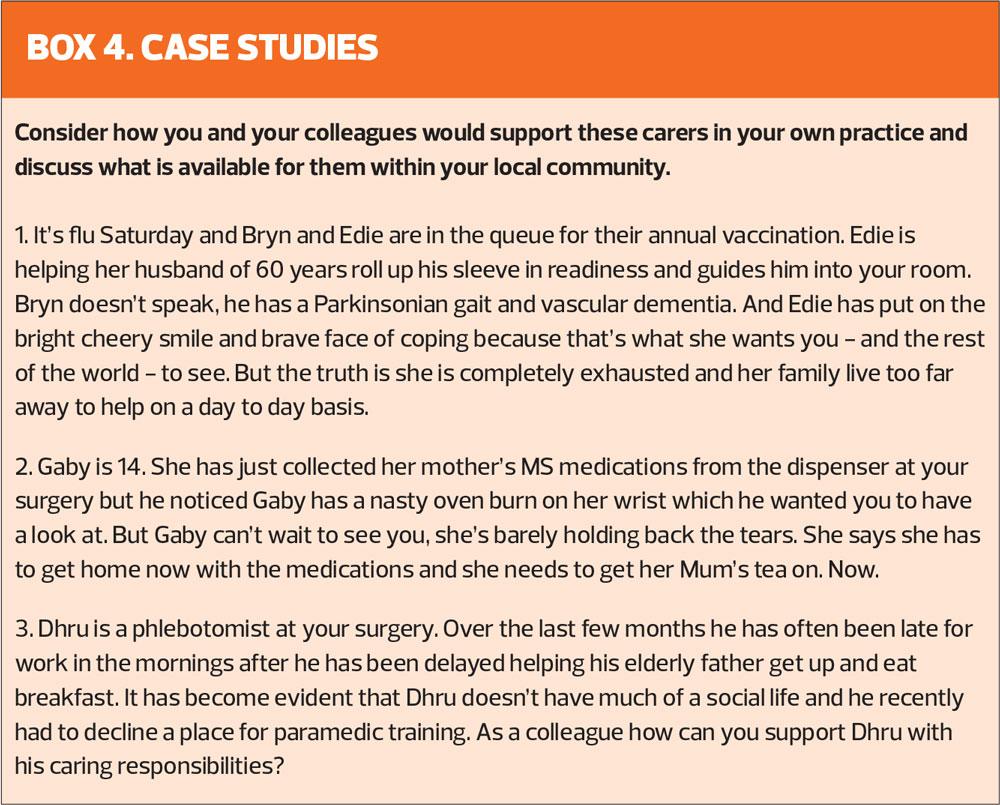
Everyday we see patients who would struggle to get through their daily life without the support of someone else to help them. In the absence of professional or voluntary organisational support, who is there within the community to enable these people to live their lives? Do we look at our patients in the wider context and ask the question – who is actually caring for them?
WHAT IS A CARER?
A carer is anyone who looks after a family member, partner, friend or neighbour who needs help because of their illness, frailty, disability, mental health problem or addiction and cannot cope without their support. The carer may be an adult or a child and the care they give is unpaid.1 We know that one in ten of the population is a carer, which equates to around 5.5 million people in England alone.2,3 Unpaid carers are worth billions of pounds to the UK economy each year, covering the shortfall in the ever increasing need for care.1 Furthermore, our most elderly carers (aged 80 and over) are providing 23 million hours of unpaid care each week.4
Carers who support other people through each day, who make the care prescribed by GPs and Social Care happen are fundamental to the lives of the people they care for. Most people do not plan to be a carer. Their caring role may have slowly evolved as a spouse’s health has deteriorated or it may have come out of crisis. And while caring can be rewarding and fulfilling, equally it can impact significantly on the carer who may also be struggling with their own health. Prioritising the needs of others, a carer’s own physical, emotional and social wellbeing can suffer. They can feel isolated, lonely, undervalued, taken for granted. It can have a detrimental affect on relationships and family life. Carers may have to juggle work with their caring role leading to financial pressures. Carers may indeed choose to hide it from their employers for fear of being unsupported or letting colleagues down. Caring for someone else can take its toll.
RECOGNISING CARERS
What steps do we take to ensure we recognise the carers in our practice population? We may be fully aware of the wife who is coping with her husband’s deterioration at the end of his life through the Gold Standards Framework care plans. During multidisciplinary team meetings we may have identified the mother who is exhausted from supporting her daughter with an eating disorder. We liaise with colleagues – community nurses, mental health teams, social prescribers and community wellbeing services – who support our patients. But how good are we at recognising the role of the daughter who has to take time off work each time her Mum needs her weekly leg ulcer dressing? Or the kind neighbour who collects prescriptions and does the laundry for the frail gentleman living alone next door? Do they recognise themselves as a carer or do they just think it is something they should be doing because they are a son or a wife or ‘just being a good neighbour’? Or even a child?
There are likely to be many carers who carry on in this supportive role behind the scenes, unidentified and unacknowledged. There will be patients on our list who look after relatives who are registered at other practices so may also go under the radar. They too need recognition and support. And our own colleagues who are carers, do we make life a little easier for them?
SUPPORTING CARERS IN OUR PRACTICES
Building on from the NHS Five Year Forward View, the 2019 NHS Long Term Plan has set priorities to further improve the recognition and support of carers.5 Acknowledging the enormous contribution of care-givers to society, the plan specifically aims to improve identification and support of carers, specifically targeting carers within vulnerable communities; supporting carers during emergency crises; taking a more proactive stance for young carers and improving digital access to services to improve interaction with the NHS.
With this in mind, what can we do at ground level to ensure that we identify and support the carers in our communities?
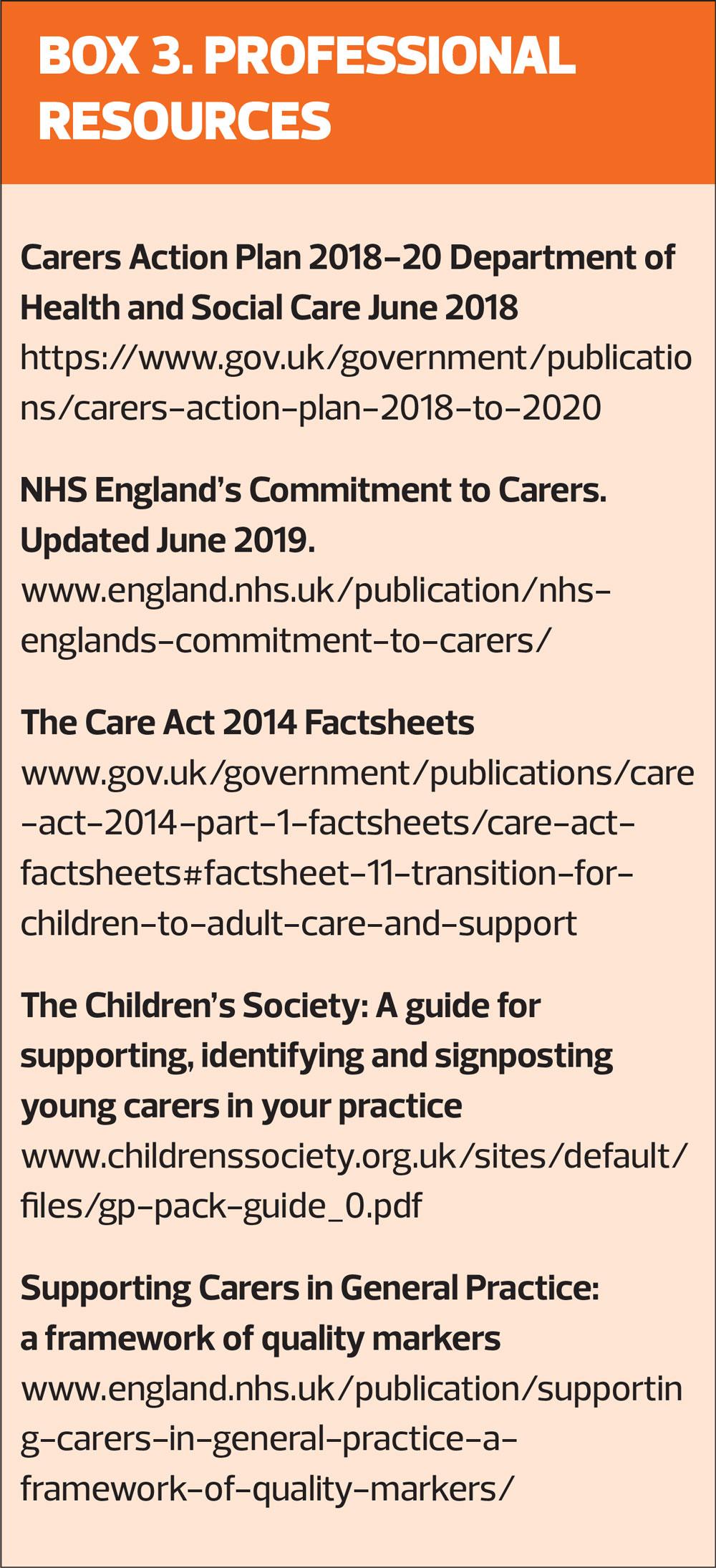
The 2019 NHS England paper Supporting carers in general practice: a framework of quality markers identifies six quality markers which primary care teams can focus on to evidence their commitment to carers.7 These quality markers ask practices to demonstrate how they:
- Identify and register carers
- Use the carers register to support holistic carer health and wellbeing needs
- Understand and respond to the needs of carers
- Make it easier for carers to access services
- Communicate with, involve and inform carers
- Promote a carer-friendly culture
Practices should involve both carers and Patient Participation Groups (PPGs) together with the whole primary care team to meet these quality markers and promote a carer-friendly ethos and to demonstrate good practice. The NHS England paper provides examples of best practice and practical tips, many of which have been recommended by carers themselves, to improve identification and support of carers. Such practical ideas include:
- Encouraging carers to self-identify in the surgery through newsletters, posters, digital displays and via the practice website.
- Reviewing the long term condition registers to help identify carers of all ages
- Supporting the physical health and emotional wellbeing of carers by offering flu vaccination, regular health checks and screening for anxiety and depression
- Readily providing information on local carer support services, referral to social prescribing schemes and local community-based support
- Identifying a Carers Champion within the practice to support carers
- Offering priority/flexible or virtual appointments to carers and those they care for
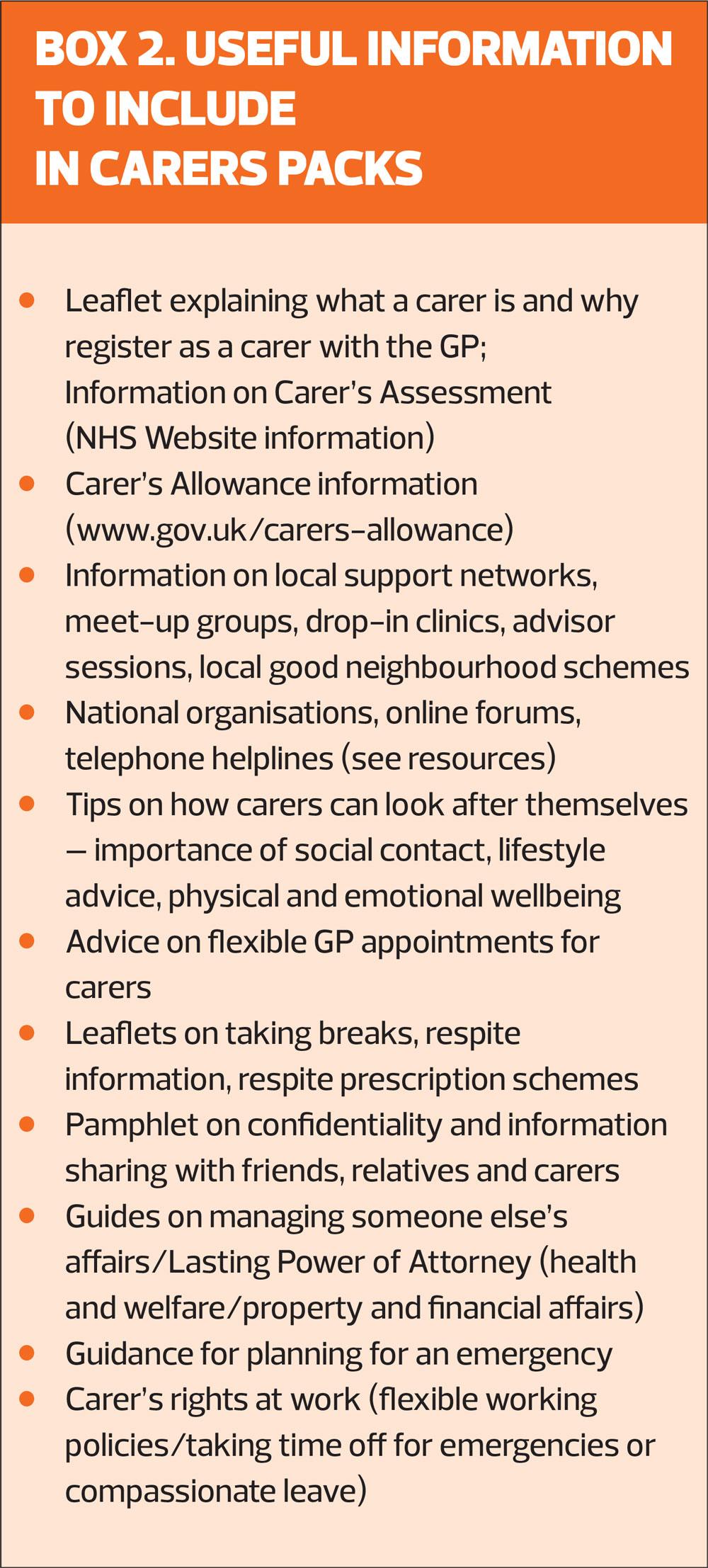
- Providing a Carers Information Pack and Carers Passport to all carers
- Using digital and social media to communicate with carers of all ages
- Formulating a contingency plan with the cared-for and carer for use in emergency or when the carer is not available
- Working with carers to build and share knowledge of local support networks and services
- Supporting staff members who are carers and accommodating their needs
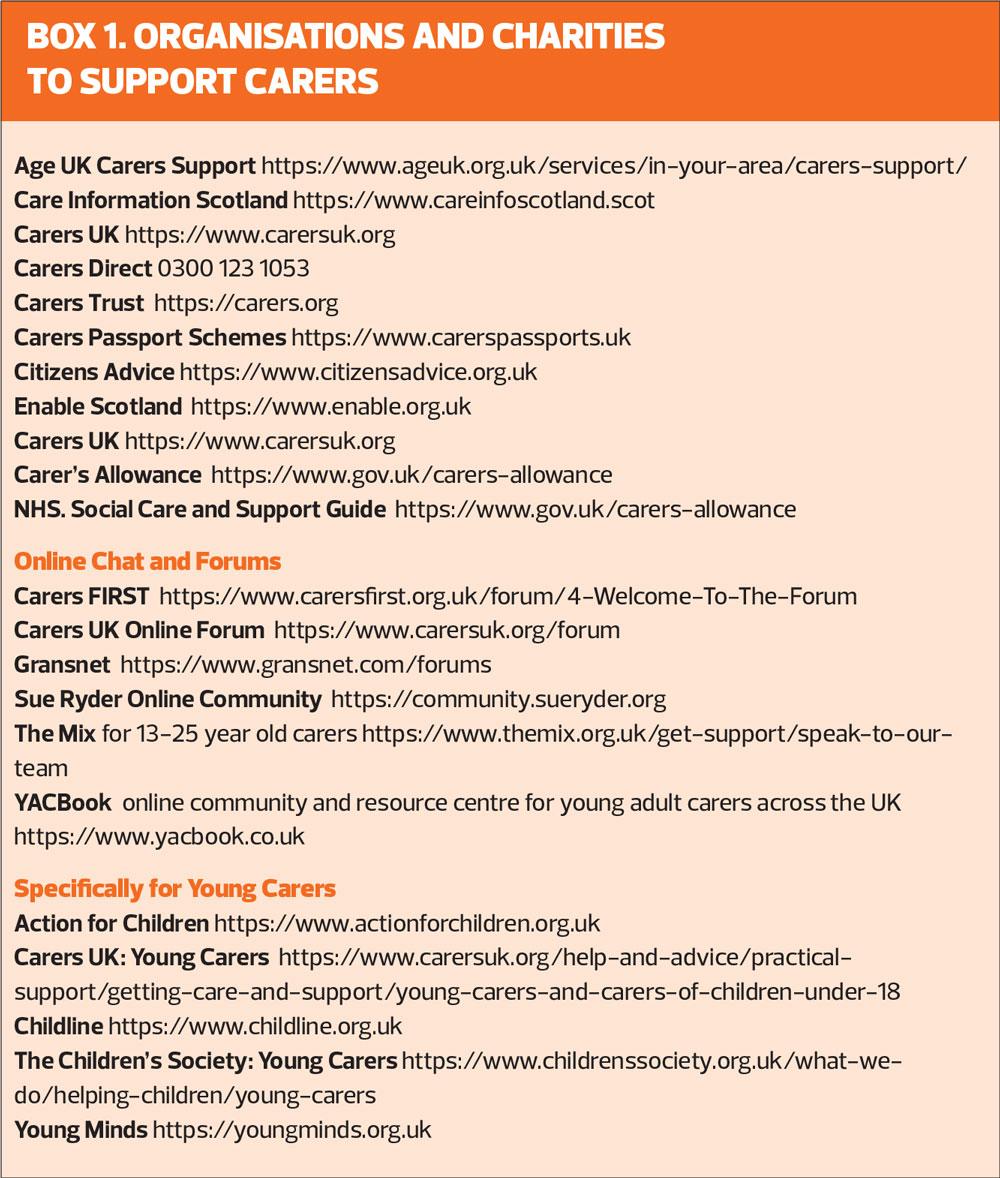
CARERS' CHAMPION
The aim of the Carers Champion is to ensure everyone within the practice knows how to identify carers, provide information and guidance as well as signpost carers to local support networks such as drop-in clinics, local support groups, online forums, helplines and workshops. GPNs are well placed to take on this role and, using the NHS document above as a framework, can form an invaluable resource for policy development and practice. Boxes 1 and 2 provide a list of national resources as well as suggestions for creating a carer’s pack. Vitally, though, is also ensuring that carers have information and access to local organisations and support.
CARER’S ASSESSMENT
The Care Act of 2014 introduced new rights for carers, recognising them in law in the same way as those they care for. Fundamentally, carers aged 18 years and over are entitled to a Carer’s Assessment from the local authority. This assesses the extent of the carer’s role and the impact on their wellbeing, work and family life. Dependent on need, carers may be given a support plan which might encompass help with transport or housework, for example, through to wellbeing support for the carer. It may also include day centre or replacement care to enable the carer to have some respite from their role. Furthermore, carers may also be entitled to a Carer’s Allowance. Carers under 18 come under the Children and Families Act 2014 and together these acts are there to ensure that the needs of all young carers and their families are met across both children’s and adult services.
YOUNG CARERS
A young carer is someone under 18 years of age who helps to look after a family member or friend who is ill, disabled or who misuses alcohol or drugs. It is estimated that one-in-five children and young people are young carers across the UK and child carers can be as young as five years old.8 Young carers may be undertaking practical tasks in the home such as housework, shopping and cooking, helping a parent with personal care, collecting and giving medications, looking after siblings or providing physical and emotional care and support. Many young carers report bullying and often keep their caring role a secret from friends and teachers. They can struggle to manage their education and caring role, missing days or being totally absent from school. They can also miss out on employment and training opportunities themselves. Mental health issues affect a third of young carers who are often being exposed to responsibilities beyond their years. Young carers are at risk of being robbed of their childhood and friendships.
Charities such as The Carers Trust and The Children’s Society are strongly committed to supporting young carers and it is absolutely vital that we identify children and young people in our practices who are providing care for others so that we can ensure they are able to access the support and assistance they need.
PLANNING FOR EMERGENCIES
Putting an emergency plan in place in the event of the carer being suddenly unable to provide care is prudent. We can’t predict what is around the corner and carers need to consider having a ‘Plan B’ in place in the event of a crisis or unforeseen event to ensure that the person they look after is not left unsupported. A contingency plan gives both the carer and cared-for peace of mind and provides detailed written guidance for those who step into the carer’s role to enable them to do what is needed. Information on the plan may include:
- Essential personal details, next of kin information, names of family, friends or neighbours who are happy to be contacted in an emergency, key safe details
- Details of agencies and professionals involved in the person’s care including GP, support workers, Social Care
- Itemised day-to-day support such as routine care and dietary requirements, help with daily living activities and healthcare needs
- Medicine storage, requirements and administration (blister packs or dossette boxes), pharmacy delivery service details, a list of allergies
- Meal delivery service, who gets the shopping, feeds the cat or walks the dogs.
- Details of day care and scheduled appointments
The emergency plan clearly needs to be specific to the individual being cared for and can be done as part of the carer’s assessment. Being proactive and making plans for the future in the event of a unplanned delay in getting care to someone, whether from a minor delay where the carer is stuck in traffic through to a sudden hospital admission, it can prevent an emergency turning into a crisis. Many areas have ‘Emergency card schemes’ for carers provided by local councils or carers’ groups which are linked with emergency call centres as a further ‘back-up’ plan to ensure the person who is being looked after gets the care they need. Some CCGs offer a ‘respite on prescription scheme’ which can help to provide funding to pay for replacement care should the carer require medical care such as an operation. Investigate what is available in your area.
TAKING A BREAK AND RESPITE CARE
Providing care for someone else is exhausting and all carers need a break and time to themselves. That might be an hour or two off each week or longer term respite in a home for the person who needs care. Respite care options may have already been identified as part of the carer’s assessment assessment. Alternatively respite support provision such as day or night sitting services or day care may be available through local social services or professional agencies. Friends and family members may be happy to step in and ‘do their bit’ and give the main carer a break to go to the hairdressers, visit friends or have a few hours each week doing a social activity they enjoy, or to have a holiday. Neighbourhood Community Schemes as well as local charities may provide support for carers to have a much-needed break.
CORONAVIRUS
And now, in April 2020, the impact of coronavirus will be an especially concerning time for carers and their cared-for. Carers UK and the Carers Trust have issued a joint statement to give guidance for unpaid carers encouraging all carers to follow public health advice, adhere to hygiene and infection control guidance, make contingency plans, network with friends and neighbours for additional support, have key information about their cared for to hand and to use technology to maintain contact and reduce isolation.9
CONCLUSION
It is part of our responsibility to recognise, register and support the carers in our practice. They are the backbone of support in this country to enable others to live their lives. Without a break, without support, the carer will not be able to unremittingly provide care, as they put their own health and wellbeing at risk and therefore make the person they care for more vulnerable.
REFERENCES
1. NHS England. NHS England's Commissioning for Carers: Principles and resources to support effective commissioning for adult and young carers; 2014. https://www.england.nhs.uk/commissioning/comm-carers/
2. Department of Health and Social Care. Carers Action Plan 2018 - 2020 Supporting carers today; 2018. https://www.gov.uk/
government/publications/carers-action-plan-2018-to-2020
3. Department of Health and Social Care. Guidance: Care Act Factsheet 8: the law for carers; Updated 2016.
4. Age UK. New AGE UK analysis finds our over 80s save Government £23 billion a year through the unpaid care they give loved ones; 2019. https://www.ageuk.org.uk/latest-press/?p=10
5. NHS England. Next Steps on the NHS Five Year Forward View;2017 www.england.nhs.uk/wp-content/uploads/2017/03/NEXT-STEPS-ON-THE-NHS-FIVE-YEAR-FORWARD-VIEW.pdf
6. NHS England. The NHS Long Term Plan; 2019. www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf
7. NHS England. Supporting carers in general practice: a framework of quality markers. June 2019. https://www.england.nhs.uk/publication/supporting-carers-in-general-practice-a-framework-of-quality-markers/
8. Carers Trust. Key facts about carers and the people they care for. https://carers.org/key-facts-about-carers-and-people-they-care
9. Carers Trust. Joint statement: Carers UK and Carers Trust Covid-19 (coronavirus); 11 March 2020. https://carers.org/sites/default/files/
media/covid-19_joint_statement_one.pdf
Related articles
View all Articles