Adherence: to what and for whom?
LIZ BRYANT
LIZ BRYANT
MMedEd, RGN, NP
Nurse practitioner in general practice, practice tutor at the Open University, Regional Trainer for Education for Health
Adherence might be described as ‘sticking to the plan’. The question is what plan, who contributes to it and how does that affect a person’s ability to stick to it?
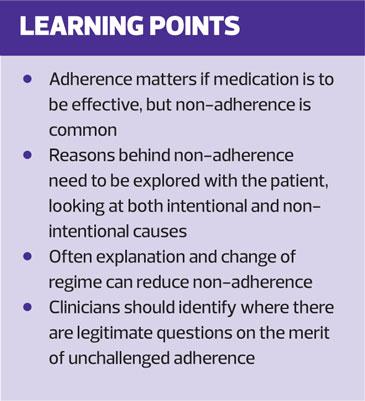
People often do not adhere to advice and/or treatment. They don’t always ‘stick to the plan’. In fact one in five patients in the UK do not complete their course of treatment and 200,000 people in the European Union die because of non-adherence to medication.1
Consider the importance of effective medication regimens, such as isosorbide mononitrate or methotrexate, or the role of behaviour change, such as someone stopping smoking or starting to walk their dog, and the difference they can make. We would expect the impact to be most powerful when the behaviour or medication is adhered to regularly. Actions to improve health or control illness often need to be continued to be effective, and poor adherence leads to poor outcomes. You will be able to think of many examples, such as Judith (below), from your own practice.
Judith
Judith, a carer for both her mother and her grandchildren, came for a NHS Health Check after her 60th birthday in April. Her blood pressure and lipids were raised and her risk of cardiovascular disease over the next 10 years was calculated as 12% (using QRisk3). She was not overweight, and she had a reasonable diet, but her father had had his first episode of angina aged 55.
She could not see how she could fit regular exercise into her busy life, but accepted treatment for hypertension (amlodipine). Her blood pressure was 128/82mmHg when it was checked 2 weeks later so the medication was continued. She was next seen in the autumn having only taken two months of the prescription. Her blood pressure still exhibited Stage 1 hypertension (over 135/85mmHg at home).
Why didn’t she take the tablet as prescribed?
- She forgot when she was busy – unintentional non-adherence
- She ran out of them when she was unable to get to the chemist – intentional non-adherence due to the additional complications of adhering, and
- In the hot summer her swollen ankles appeared to return to normal when the medication ran out – intentional non-adherence because of perceived side effects.
In addition, like many people with high blood pressure, she saw the cause as stress and therefore when she felt less stressed there was less need of medication. An international, systematic review noted that patients very commonly thought that high blood pressure caused symptoms such as dizziness and headache, and without symptoms medication was not necessary.2
WHAT ARE THE ISSUES?
There are many reasons for medication not being taken as prescribed, and those reasons do not always divide neatly into intentional and unintentional non-adherence. Forgetting a tablet is far more likely if you do not have much confidence in its efficacy.3 How might one identify and explore the issues behind non-adherence in an individual or in a group of people?
A study of people with type 2 diabetes,3 identified a link between the complexity of the medication regimen and unintentional non-adherence, and between concern (about impact and side effects) and intentional non-adherence. However, the perceived necessity for the medication did not seem to correlate with the level of adherence. So someone might conclude: ‘I am reluctant to take it because of possible side effects despite my understanding of the dangers of poorly controlled diabetes’.
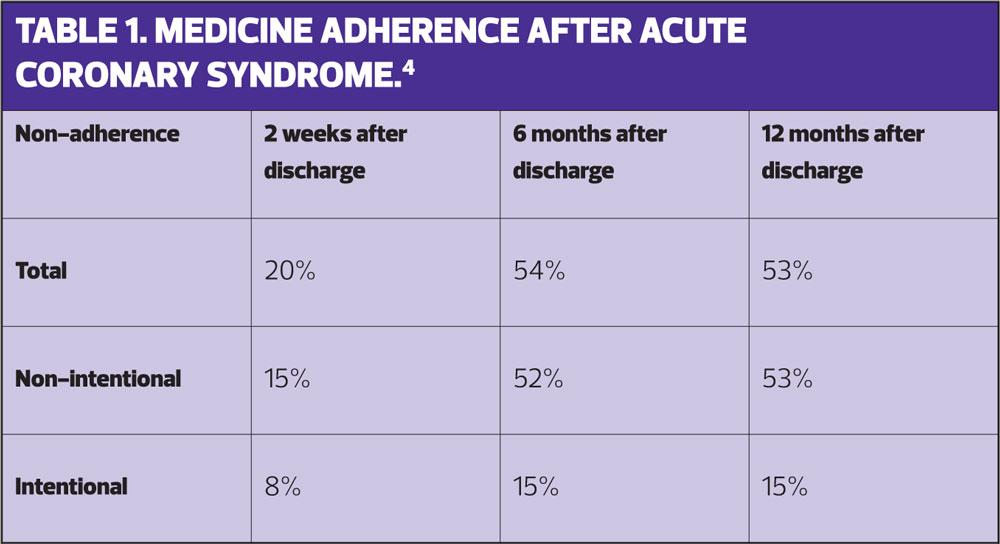
In a study on medication adherence in the year immediately after acute coronary syndrome (ACS), total medication non-adherence was 20% two weeks after discharge, 54% six months after discharge and 53% twelve months after discharge. Interestingly the corresponding figures for intentional non-adherence were 8%, 15% and 15% and for unintentional non-adherence 15%, 52% and 53%.4 In this study, perhaps due to the turbulence and vulnerability created by an episode of ACS, people forgot to take medication, or could not access it, and this unintentional non-adherence increased significantly in the first six months after discharge. (Table 1)
A ‘systematic review of systematic reviews’ discounted severity or duration of the disease as factors affecting adherence.5 However, belonging to an ethnic minority, unemployment and cost to the patient all had negative impacts on the regularity of medication intake. It appears possible that day-to-day complexity is a powerful deterrent to taking prescribed treatment. These findings are unlikely to surprise you, but they can be forgotten even during a medication review.
STRATEGIES FOR TESTING THE VALIDITY OF ADHERENCE
What strategies could you use the test the validity of adherence in a particular individual at a particular time, and how might this understanding affect your consultations?
Consider the case of Hussein.
Hussein
Hussein has type 2 diabetes and had a myocardial infarction 3 years ago. You can see that his last prescriptions for bisoprolol, atorvastatin and metformin are dated six months ago, but he tells you that he has ‘plenty left’ and is sure that he takes them regularly.
Here are some helpful approaches.
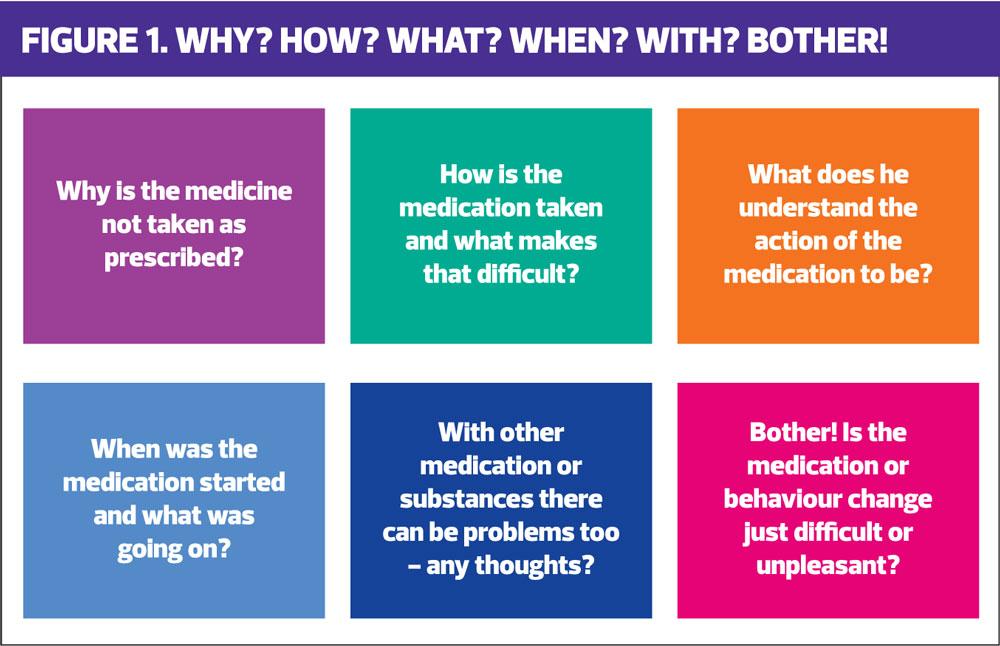
- Listen to what the patient thinks may be happening, and why he thinks this is so. Explain that many people forget medication, but it is important to explore any fears, concerns or possible side effects he has.
- Allow him to explain when he takes his medication, and what barriers there might sometimes be to taking it regularly. Shift work can be particularly troublesome, as can the availability of public toilets.
- Ask what he thinks each medication does; patients sometimes omit aspirin or anything else that ‘thins the blood’ in the cold weather.
- Look at when each medication was introduced; what else was going on? Has this medication never established its place in his self-care?
- Look at other medication, including ‘over the counter’ products, and other intakes e.g. alcohol, health preparations and material on line that might be taken in preference to the prescription.
- Sometimes tablets or other medications are just tiresome and unpleasant – difficult to swallow, bitter, tricky to manipulate with arthritic hands, and so-on. For example, many people are unlikely to persist with three times daily carboceistine, or a fiddly inhaler, unless they can see a positive impact.
This could be seen as ‘Why? How? What? When? With? Bother!’. (Figure 1) Use such prompts to identify reasons for non-adherence. With more information, you can look for solutions together.
TACKLING THE ISSUES
If the problem is a practical one
The exemplar for the practice nurse is respiratory medication. Similar active ingredients can be delivered in a variety of effective ways, and careful shared consideration and demonstration will help select the best device. Knowledge of the available range, including those outside the local formulary, is essential. Joint discussions between primary and secondary care, within CCGs, can help ensure a realistic and cost effective approach to providing choice and continuity of care. Patients become confused and sceptical if inhalers change with every change of provider. Pharmacists can be asked to check technique before they dispense the first script, to confirm that the patient really can manipulate the device successfully.
Slow or modified release medication can reduce frequency of administration. This has made a noticeable difference for many people taking metformin and the modified release form is specifically mentioned in the guidelines.6 Different brands of calcium and vitamin D can be more/less palatable, and dosette boxes make regular daily dosing much simpler. Pharmacists are an underused source of expertise on different formulations and adherence solutions.7
If the problem is knowledge and understanding
Many of us take medication obediently, not questioning the timing or dosage, but if we don’t understand the reasons behind the regimen we are more likely to omit or change a dose. People may have past experiences that affect the way they ration or omit tablets. You will want to explore why the patient thinks the dose should be taken in this way. You will need to value their experience, but you may also need to challenge their interpretations.
Any medication that relieves symptoms is monitored by the patient through the effect it has, most often the short-term effect. Overuse of salbutamol inhalers often starts because salbutamol makes an immediate difference while the inhaled steroid doesn’t. Paracetamol relieves pain when it is taken, but there is no indication for taking another dose until the pain worsens again. This may be eight hours after the first dose and the pain may then be less easily controlled because of the gap between doses.
Understanding of how different medications work, the length of the duration of their effect and the time taken to reach a steady state where the plasma concentration stabilises, enables you to explain how to use the dosage most effectively.8
Explaining the reasons behind the sudden imposition of at least four new pills – which appear to do nothing palpable – after cardiac revascularisation might at least encourage temporary adherence. Explaining the complementary roles of bronchodilators and inhaled steroids as relievers and preventers has proved helpful when establishing asthma action plans,9 but inhaled steroids are still often neglected until another exacerbation; this phenomenon also links in to our perceived sense of vulnerability and our beliefs about medication.
IF POOR ADHERENCE IS DUE TO BELIEFS ABOUT HEALTH AND TREATMENTS
An RCGP report10 describes how a person’s health beliefs about, for example, treatment for a particular illness are based on their perceptions of four core concepts:
- Perception of risk: how great is the risk of this illness or problem for me at this moment?
- Perception of threat: how serious might it be?
- Perception of barriers: how difficult will it be to change my lifestyle, or take the treatment that is being suggested?
- Perception of benefit: if I follow the treatment, what will be the benefits?
In the case of Hussein, if his development of diabetes was not accompanied by symptoms, his perception of the risk of complications and the threat of their seriousness may suggest to him that urgent attention is not required. His experience of large metformin tablets that give him embarrassing wind presents barriers and no clear benefits. This all adds up to his being unlikely to take the medication assiduously. However, if his older brother also has type 2 diabetes and is losing his sight and mobility, both the risks and the severity of those risks become much larger and the barriers more manageable because of the perceived benefits of not developing diabetic retinopathy.
Nothing is quite as straightforward as this. He may also dislike taking tablets and fear dependency and side effects. In the international systematic review of lay approaches to blood pressure medication,2 many patients were worried about the long term effects and preferred to ‘let nature take its course’. It is reasonable to conclude that the medication information sheets included with the prescription are not enough to allay these fears! The risks are usually listed without probabilities, so that sudden death appears just as likely as gastric irritation after a dose of aspirin.
Clear information, framed around Hussein’s understanding of his conditions and his anxieties about his treatments, can be built up through more than one consultation. The weeks in between will enable him to monitor his responses to the medication, and accumulate evidence on the positive effects, and side effects, of it. Often a ‘drug holiday’ (most notably statins) of a couple of months can confirm or refute a possible side effect, and the impact on the lipid profile.
IS ADHERENCE ALWAYS THE RIGHT THING?
‘The person who takes medicine must recover twice, once from the disease and once from the medicine’ – so wrote Dr William Osler 1892 in ‘The Principles and Practice of Medicine’.
There may be ‘an elephant in the room’. Might there be a bit too much clinician adherence to a guideline or drug regime at the expense of patient choice, shared decision making and conflicting evidence?
Let’s look at Judith again. She is taking medication for Stage 1 hypertension to prevent the development of cardiovascular disease, after discussion with the nurse practitioner and with her mother who witnessed her husband’s death. The GP might have pushed for lifestyle change first. (Apparently GPs are more likely to start medication on a single raised clinical CVD risk factor while nurses are more likely to adhere to guidelines and look at overall risk.11)
In the case of hypertension the guidelines are wavering.12 There may be little benefit from drug treatment for people without target organ damage. A recent Cochrane review established that antihypertensive drugs used in the treatment of adults (primary prevention) with mild hypertension (systolic BP 140-159 mmHg and/or diastolic BP 90-99 mmHg) have not been shown to reduce mortality or morbidity in RCTs, and treatment caused 9% of patients to discontinue treatment due to adverse effects.13
And what about lipid lowering in primary prevention? There is still significant controversy about the role of statins,14 and an increasing emphasis on the modification of lifestyle.15 And this is just from research and clinicians’ expert opinions. The role of medication is even less clear when the patient’s views are taken into account. A qualitative study in some general practices in Liverpool demonstrated that evidence-based guidelines make assumptions about people’s preferences, and that, in general, patients dislike taking medication and want to consider adverse effects and cost of treatment.16
In essence, patients may be less keen on adhering to a guideline than health professionals. Perhaps we need to adhere a little less firmly to the assumptions and processes that we bring with us. There is no replacement for sharing of information, values and preferences, as well as experiences, where decisions about treatment and management are concerned. People will rarely stick to something if they do not really like it or agree with it, and, additionally, there are many situations where there is more than one reasonable pathway.
Bosworth et al,18 uses a case study to demonstrate how patient-centred skills such as shared decision-making and motivational interviewing can be used to increase adherence and support autonomy in a primary care situation. You will have encounters every week where you have employed similar skills to arrive at a joint plan.
Steve
Steve lost faith in medication in general when his fatigue and breathlessness was put down to his COPD, and his symptoms did not improve over a series of inhaler changes and lengthy sessions with the practice nurse to relearn inhalation techniques. He stopped requesting new appointments with his GP, and it was only at his annual review that an irregular pulse generated investigations, an echo cardiogram and a diagnosis of atrial fibrillation and left ventricular systolic dysfunction. He was given a collection of tablets (beta-blockers, statins, ACE inhibitors and warfarin) to take. His breathlessness improved but he felt slow, lethargic and ached all over. Miriam, his wife, told him it was only to be expected at his age. He gave up gardening and researched his family tree online instead.
He ran out of some of his tablets on holiday but didn’t tell Miriam. He felt much more lively on his return, and took up bowls. He resumed his medications, and then realised that they were responsible for his fatigue and muscle aches, and stopped everything apart from the warfarin. He comes to see you for his annual review.
- How will you approach this non-adherence? He is raising questions about the medication regimen and its suitability for him.
- How will you respond?
There is no ‘right’ answer. It depends very much on the people involved, the degree of his heart failure and any other co-morbidities, but reflect on what his issues might be, what information might be helpful for you to consider together, and what might assist you in coming to a decision about the way forward.
IN CONCLUSION
There are further concepts, such as patient activation which employs the degree to which someone is engaged in looking after their health,19 and group consultations,20 where sharing with peers in a similar situation can influence adherence. These are being used to advance both patient participation and the cost-effective use of medication and behavioural change, but the basis of better adherence must come from a shared agreement that the treatment is worth adhering to. Sometimes, on balance, it isn’t.
Adherence and non-adherence are best considered in the light of evidence-based medicine, policy-driven guidelines and holistic care for that individual at that time.
REFERENCES
1. Hagan P. The true cost of medication non-adherence. Omnicell UK — adherence let’s take care of it campaign 2015. http://www.letstakecareofit.com/wp-content/uploads/2015/10/The-True-Cost-of-Medication-Non-Adherence-Report.pdf
2. Marshall IJ, Wolfe D, McKevitt C. Lay perspectives on hypertension and drug adherence: systematic review of qualitative research. BMJ 2012; 344: e3953.
3. de Vries S, Joost C. Keers B, et al. Medication beliefs, treatment complexity, and non-adherence to different drug classes in patients with type 2 diabetes. J Psychosom Res 2014; 76: 134–138
4. Molloy G, Messerli-Bürgy N, Hutton G, et al. Intentional and unintentional non-adherence to medications following an acute coronary syndrome: A longitudinal study. J Psychosom Res 2014; 76: 430–432
5. Mathes T, Jaschinski T, Pieper D. Adherence influencing factors — a systematic review of systematic reviews. Arch Public Health 2014;72(1):37.
6. NICE NG28. Type 2 Diabetes in Adults: Management. December 2015. https://www.nice.org.uk/guidance/ng28
7. Abderrhaman B. Health literacy, medication adherence and thriving healthcare systems: joining the dots. Pharmaceut J 2017; 8: 11 https://www.pharmaceutical-journal.com/opinion/insight/health-literacy-medication-adherence-and-thriving-healthcare-systems-connecting-the-dots/20203831.article
8. Stringer J. Basic concepts in pharmacology: a student’s survival guide. 1995. London, The McGraw-Hill Companies
9. British Thoracic Society/Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma, 2016. https://www.brit-thoracic.org.uk/document-library/clinical-information/asthma/btssign-asthma-guideline-2016/
10. Rowlands G, Protheroe J, Price H, et al. Health literacy: a report from a RCGP-led health literacy workshop. June 2014. RCGP http://www.rcgp.org.uk/clinical-and-research/resources/a-to-z-clinical-resources/health-literacy-report.aspx
11. Mohammed MA, Ei Sayed C, Marshall T. Patient and Other Factors Influencing the Prescribing of Cardiovascular Prevention Therapy in the General Practice Setting With and Without Nurse Assessment. Medical Decision Making 2012; 32(3): 498-506
12. NICE CG127. Hypertension evidence update, March 2013. https://www.nice.org.uk/guidance/cg127/evidence/evidence-update-pdf-248584429
13. Diao D, Wright JM, Cundiff DK, Gueyffier F. Pharmacotherapy for mild hypertension. Cochrane Database Syst Rev 2012; 8: CD006742. DOI: 10.1002/14651858.CD006742.pub2.
14. Abrahamson JD, Rosenberg HG, Jewell N, Wright JM. Should people at low risk of cardiovascular disease take a statin? BMJ 2013;347:16123
15. Stewart JI, Washbrook E, Tonkin A. An international perspective on cardiovascular risk management: recommendations for moderate to low risk patients. Primary Care Cardiovascular Journal 2010;3:1
16. Lewis DK. Robinson J, Wilkinson E. Factors involved in deciding to start preventative treatment: qualitative study of clinicians’ and lay people’s attitudes. BMJ 2003;327:841
17. Bostock-Cox B. When guidelines collide – part 2: Asthma treatment. Practice Nurse 2018;48(07):20-24
18. Bosworth HB, Fortmann SP, Kuntz J, et al. Recommendations for providers on person-centered approaches to assess and improve medication adherence.Journal of General Internal Medicine 2017;32(1):93–100.
19. Gilburt H. When delivering treatment is not enough. The Kings Fund. January 2015. https://www.pifonline.org.uk/wp-content/uploads/2014/07/Pharma-Time-Patient-Activation-Engagement.pdf
20. Craig G. Group consultations: better for patients, better for nurses? Practice Nurse April 2017;47(04):15-18
Related articles
View all Articles