Getting back to basics
Beverley Bostock
Beverley Bostock
RGN MSc MA QN
ANP Mann Cottage Surgery,
Moreton-in-Marsh
PCN Nurse Co-ordinator, Hereford
Practice Nurse 2022;52(5):16-18
Harsh findings from two recent surveys suggest that there is room for improvement in the way we manage long term conditions, and that there is a great deal of catching up to do after the past couple of years
It’s tough in general practice at the moment. There’s a never-ending list of things to do and we are playing catch-up as a result of the pandemic. It is easy to feel overwhelmed, disheartened and as if what we do is never quite good enough. However, most of us are doing our utmost to be the best we can, doing the job we (hopefully) love. It can be quite frustrating, then, when patient feedback delivers a harsh truth by telling us that what we are doing is not good enough. That’s the message from two recent patient surveys, one from Asthma and Lung UK looking at asthma care, the other from Diabetes UK (DUK), assessing diabetes care, which suggest that the quality of care delivery is a real cause for concern.1,2 As a nurse working in general practice myself, and one who has a particular interest in asthma and diabetes care, I’m worried about the key messages being given by people living with these conditions to healthcare professionals.
This article aims to identify the important findings from the Asthma+Lung UK and DUK surveys and offers an opportunity to consider how general practice nurses (GPNs) can ensure the delivery of a high standard of holistic, evidence-based care to improve a broad range of patient outcomes including optimising quality of life and minimising the risk of complications or exacerbations. In view of these reports, the article focuses on getting back to basics with asthma and diabetes reviews and identifies what should be included in the review.
The onset of the pandemic ended normal practice as we knew it. Clinics were cancelled and then switched to remote delivery, with the impact being felt most keenly in areas of health where face-to-face care is either essential or preferred by the clinician, the patient or both. We are now seeing a gradual return to more 'normal' practice for the first time since the pandemic started. April 2022 also saw the return of the Quality and Outcomes Framework (QOF) so we now have opportunities and a driver for re-engagement, especially with people who may not have been seen during the past 2 or more years.
Before the Asthma+Lung UK and DUK patient surveys make us too despondent, it should be recognised that these surveys are made up of self-selecting groups of potentially dissatisfied individuals who feel that they are not being heard and the survey offers an opportunity to voice their discontent. Furthermore, the numbers in these surveys represent a tiny minority of the total population with each condition. It would be completely wrong, however, to dismiss the messages that are coming from the reports, and we should be prepared to take a long hard look at what we are doing and reflect on whether there is room for improvement. This is not just for each nurse to consider but is something that needs to be taken to practice managers, GP employers and lead nurses in primary care networks and beyond, so that effective, streamlined and person-focused care can become the ‘new normal’. The delivery of high quality care needs adequate resourcing – time, training and funding – and nurses need to be prepared to assert the need for all of these things in order to do a good job.
Patient organisations have clearly indicated that patient satisfaction with care during the past year has dropped significantly,1,2 with the Asthma+Lung UK survey suggesting that a significant proportion of respondents were not even getting the most basic care.1
DIABETES
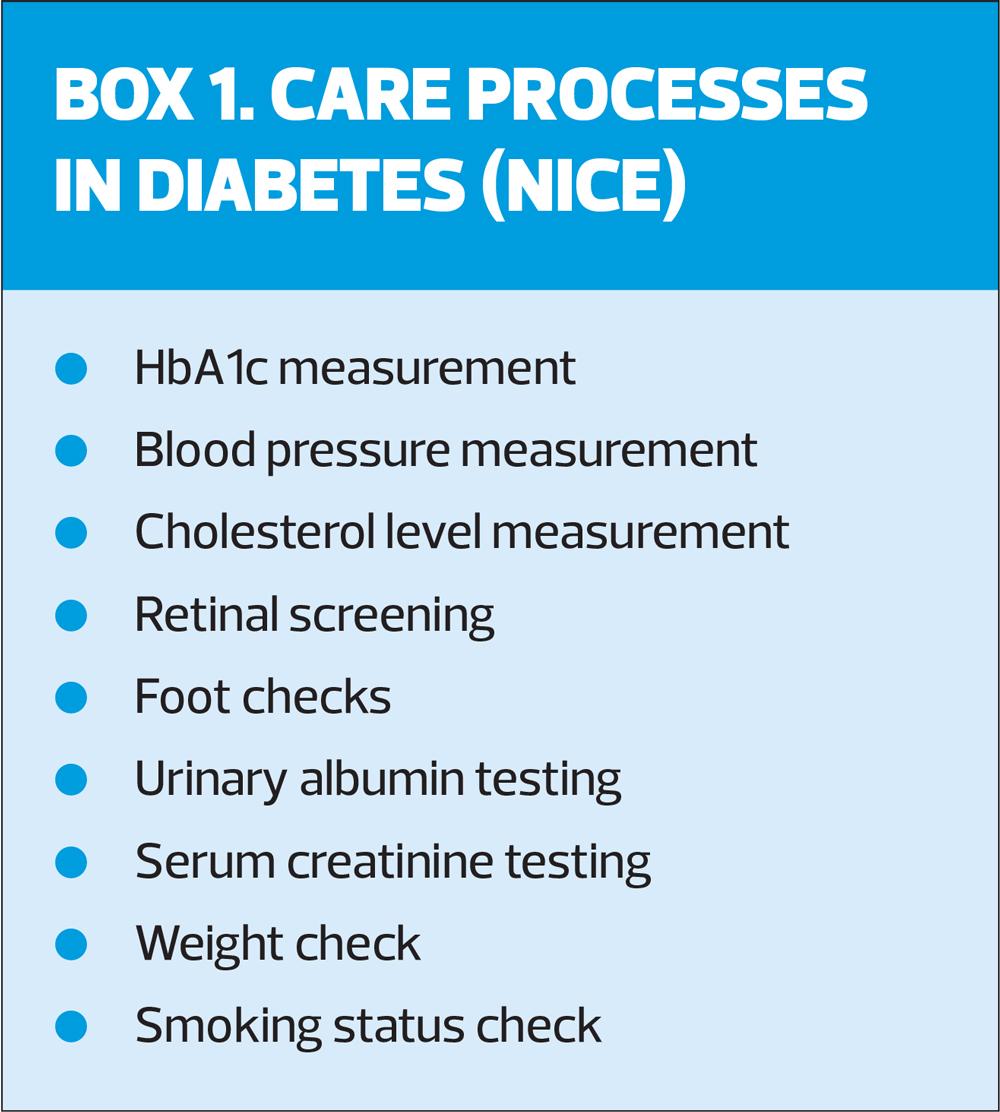
The DUK report which gathered information from 10,000 people, out of the 4.9 million people living with diabetes in the United Kingdom.2 Of those who took part in the survey, 47% reported difficulties managing their condition during 2021, with 63% linking those difficulties at least in part to not having sufficient access to their health care team. Worryingly, this figure rose to 71% in deprived areas, correlating with a reported lack of basic diabetes health checks. This lack of basic care was reportedly higher in deprived areas than in less deprived areas. Shockingly, one in six survey respondents stated that they had had no contact with their diabetes healthcare professionals since before the pandemic. It is essential that people living with diabetes have access to an adequate standard of care because of the high risk (and cost) of complications if the condition is not managed correctly and proactively. Every week, diabetes leads to more than 190 amputations, 770 strokes, 590 heart attacks and more than 2,300 cases of heart failure. Around 10% of the NHS budget is taken up on diabetes care, but 80% of that goes on treating the complications of diabetes. Complication risk is reduced by implementing the NICE care processes (Box 1), and addressing the ABC targets – A1c, blood pressure and cholesterol.
Delivering on the care processes and hitting ABC targets would help to significantly reduce the risk of complications so GPNs need to be at the vanguard of ensuring we deliver on this now we are getting back to normal.
DUK says that there must be a renewed and reinvigorated attempt to support people with diabetes to live well and avoid complications.2 In order to achieve this, they recommend that we need to get back to offering regular reviews based around the NICE care processes and taking a shared approach to developing a care plan. People should be able to access to diabetes education, so that they are better able to manage it. A routine assessment of emotional and psychological wellbeing should be made, and specialist support, where needed, should be made more accessible. Healthcare professionals need to have an up-to-date knowledge of diabetes technology to support people with diabetes to self-manage and help to lose weight should be offered including referral to specialist weight management services. People living with diabetes should also be able to access facilitated peer support, such as through group consultations.
GPNs should reflect on service provision through the pandemic. Relocation to COVID services may well have affected service delivery in other areas but now is the time to go through disease registers and identify people who have not had their annual review, prioritising those whose reviews are most out of date, and/or whose control was inadequate at their last review. These people, then, need to be offered a review at their earliest convenience, using simple, non-clinical and friendly language to encourage them to come in.
GPNs are advocates for high quality patient care (not just meeting QOF targets) but it seems that putting QOF on hold may have been detrimental to ensuring that care continued. In practical terms, people with long term conditions should be able to self-care for most of the time, as they are only with a healthcare professional for limited time. In reality, however, there are many barriers to this, including a lack of education and support and people not recognising how serious diabetes can be. It is now time for GPNs to carry out holistic healthcare assessments and offer support and education to reinforce messages that may have been forgotten.
So, let's revisit the key components of a diabetes conditions review. For every person living with a long-term condition, it is essential to acquire a general understanding of how they have been coping and how they feel about their condition at this time. Understanding an individual's perspective of their condition and considering how this perspective might influence their motivation to change may help to structure the consultation.
Specific content for diabetes reviews should include an assessment of renal function to include blood tests and urine tests for ACR. Body mass index should be measured as this may have altered during the pandemic. HbA1c, blood pressure and lipids should also be assessed (remember to Keep Watching the ABC – Kidneys, Weight, A1c, BP and Cholesterol) along with the annual foot check for pulses and neuropathy. The date of the last retinopathy screen should be noted and follow up appointments made for people who have missed their review during the pandemic. A refresher should be offered on dietary approaches to managing diabetes, including newer interventions such as very low-calorie diets or low carbohydrate options, along with a tailored discussion on activity levels. A conversation about smoking is important, even in people who have previously stopped smoking, as the pandemic, episodes of lockdown and increased stress levels may have led to a resumption of negative health behaviours. In a previous edition of Practice Nurse, we published the ‘Diabetes Diary’ which can support people living with diabetes and their healthcare professionals to ensure that the key areas of diabetes care have been addressed.3
ASTHMA
In the Asthma+Lung UK survey, only a third of people with asthma who responded received the most basic level of care last year, which is the lowest level since 2015.1 Like DUK, Asthma+Lung UK has listed the key improvements they would like to see, going forward. These include ensuring access to basic care for everyone with asthma, through the implementation of pathways that identify those with uncontrolled asthma, who are most at risk of a life-threatening asthma attack. They also recommend that treatment guidelines should be amended to reduce the role of reliever inhalers in care and embrace new treatments such as biologics, in order to improve outcomes for millions with asthma. Beyond general practice they ask that policy makers ensure that everyone with suspected asthma has access to early and accurate diagnosis and that lung health is made a priority in all plans, reflecting the fact that poor lung health is linked to health inequalities and poor health outcomes across the UK. The good news is that several of these areas are already being addressed, e.g. increased access to FeNO testing and biologics and through the development and imminent publication of the new uncontrolled asthma pathway for primary, secondary and tertiary care.
Specifically, asthma reviews should include an assessment of current control, using tools such as the asthma control test (ACT), any history of exacerbations and assessment of inhaler technique. This would also provide an opportunity to consider whether a change of inhaler is indicated, based on patient preference, patient ability or where appropriate, environmental concerns. Current doses of medication should be reviewed and the need to step up (or down) should be considered. Using a maintenance and reliever therapy (MART) approach can facilitate appropriate step up/down use of medication in a personalised way. The use of reliever therapy (short acting beta2 agonists – SABAs – or extra doses of MART therapy) should be assessed. More than six SABAs per year is a red flag for poor control as if someone is using their rescue therapy 2-3 times a week, they should only get through two inhalers per year at most. Comorbid conditions such as allergic rhinitis can contribute to asthma symptoms and nasal symptom questionnaires (or ones for reflux cough or breathing pattern disorders) can be accessed online to help identification and management of these conditions. Adherence should be checked by looking at the number of preventer inhalers ordered each year, although people can order inhalers without actually using them so questions should be asked about any stockpile they may have at home. Personalised asthma action plans should be developed and reviewed with the patient to ensure that they understand what good asthma control looks like for them, how to recognise reduced control and what to do about it. Asthma+Lung UK has published an excellent guide to making the most of the review and saving time and energy.4
CONCLUSION
Patient surveys can be devastating to read, but GPNs should see them as an opportunity to reflect on the current level of care being provided and identify any possible gaps. There needs to be a whole team approach to improving care, involving frank conversations about the need for adequate time and resources. The evidence base should be reviewed, taking note of any new guidance or interventions that might help people re-engage with their long term condition.
REFERENCES
1. Asthma+Lung UK. Transforming asthma care in the UK; 2022 https://www.blf.org.uk/sites/default/files/Fighting%20back_V3.pdf
2. Diabetes UK. Diabetes is serious; 2022 https://www.diabetes.org.uk/get_involved/campaigning/diabetes-is-serious
3. Bostock B. Diabetes - putting the patient in control. Practice Nurse 2021;51(4):18-22
4. Asthma+Lung UK. Six ways to save time and energy; 2022 https://www.asthma.org.uk/for-professionals/professionals/down-with-dnas/
Related articles
View all Articles