Anaemia – why it’s important and what you need to know
Samantha Timmins
Samantha Timmins
Patient Blood Management Practitioner
NHS Blood and Transplant
Practice Nurse 2021;51(6):20-22
Accessing education about anaemia is just one of the barriers to improving the care of patients who face the risks of greater need for perioperative transfusion, poor pregnancy outcomes, and increased morbidity and mortality
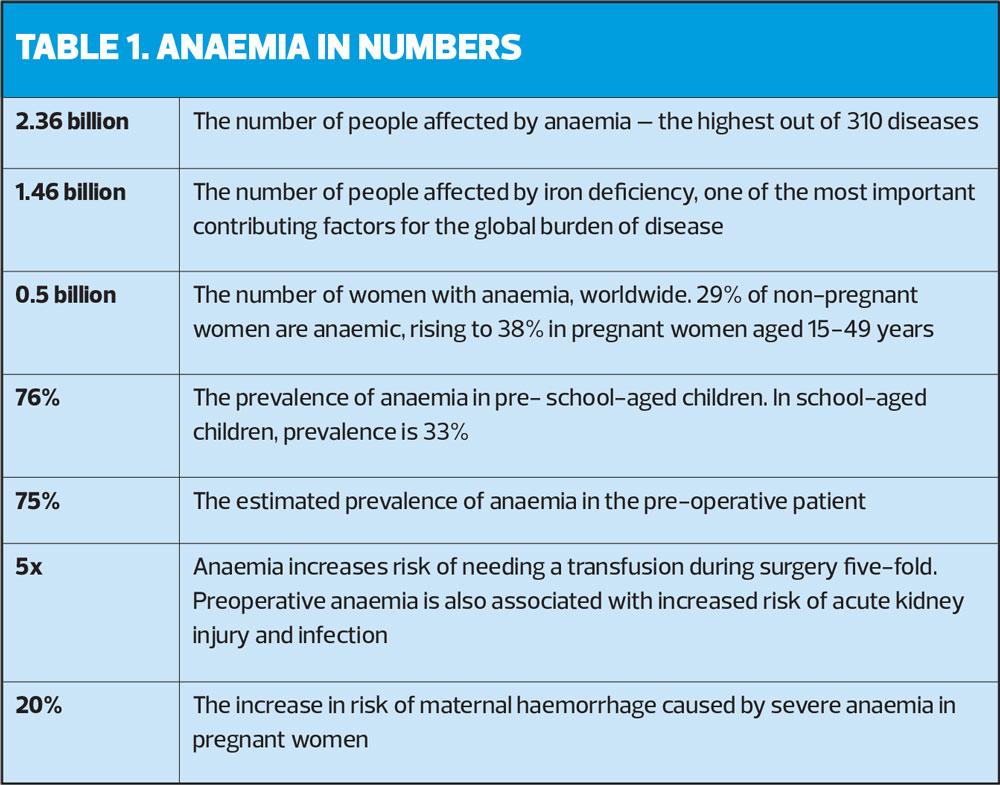
A lack of understanding and awareness of anaemia among healthcare professionals has been widely documented over many years, yet a recent study estimates that anaemia affects over 1.7 billion people worldwide, accounting for more than 58 million years of life lived with disability. With anaemia associated with increased risks of morbidity, mortality and poor pregnancy outcomes, it’s a topic that should be on every nurses’ radar.1
Accessing anaemia education remains a barrier to raising awareness and improving care. Specific education during my own undergraduate training in the early 2000’s was limited, and on becoming an anaemia specialist nurse, I embarked upon a difficult journey of self-teaching to ensure I could give my patients the best possible care. A survey in 2015 confirmed that this was the experience of many nurses; 49% of participating nurses felt their understanding of iron deficiency anaemia, specifically, was basic at best.2
Patient Blood Management (PBM) is an international initiative to optimise the care of patients who may require a blood transfusion, and the management of anaemia is a cornerstone of PBM. The PBM team at NHS Blood and Transplant (NHSBT) support clinical practice via education, resources, toolkits, and patient information leaflets. This year we launched a series of e-Learning modules designed to support anaemia management in clinical practice, from basic pathophysiology of anaemia, to identification and management guidance for primary and secondary care practitioners. These modules are free and accessible to all via e-LFH, ESR, and our PBM website https://hospital.blood.co.uk/patient-services/patient-blood-management/.
ANAEMIA IS A SYMPTOM, NOT A DIAGNOSIS
Most professionals can correctly define anaemia as a low level of circulating haemoglobin (Hb), using the World Health Organization (WHO) definition of 130g/L for men, and 120g/L for women*.3 What is often missed is that anaemia alone is not a diagnosis, but a symptom, and arbitrary thresholds are not always useful in isolation.
A key principle of anaemia management is to identify and manage the underlying cause, and as specialties place more focus on the symptom burden of anaemia associated with specific diseases, they set their own guidance and define Hb thresholds.
A sound understanding of the pathophysiology of anaemia from deficiencies, to erythropoietin insufficiency or inactivity, to blood loss and disorders affecting distribution and circulation of red cells, as covered in the first module, Anaemia – the only introduction you need, will help support practitioners with the identification of underlying causes and the disease processes contributing to them. More importantly the module highlights key populations at risk of anaemia, and why identification and management are so important.
As the NHS shifts its focus to improving population health and prevention of ill health as part of The Long-Term Plan,4 optimising the management of anaemic patients must be a priority. Anaemia is associated not only with the standard symptom list of dizziness, fatigue, and pale skin, but patients often report low mood, isolation from a lack of energy to engage in social interaction, lack of appetite and changes in eating habits, as well as confusion and lack of concentration resulting in loss of working hours. The scope for improving general health and wellbeing is vast. But how?
The basic principles of a balanced diet are a good start for all patients and central to health promotion. The Anaemia in Primary Care Patients module provides specific dietary support, and NHSBT provides a helpful patient information leaflet, Iron in your diet available to download at www.hospitalblood.co.uk.
Deficiency-based anaemia affects the body’s ability to absorb the nutrients required for erythropoiesis. For example, when considering how to treat B12 deficiency, it is important to understand the underlying cause of the deficiency in order to treat it effectively. Oral supplementation is only recommended in the presence of dietary deficiency. Where malabsorption is suspected, further investigation is required and only parenteral supplementation is indicated for treatment.5 This can often be the case for iron deficiency anaemia in the presence of inflammation, and further information and support for understanding the physiological mechanisms of anaemia can be found in the first module.
ASSESSMENT AND HISTORY-TAKING
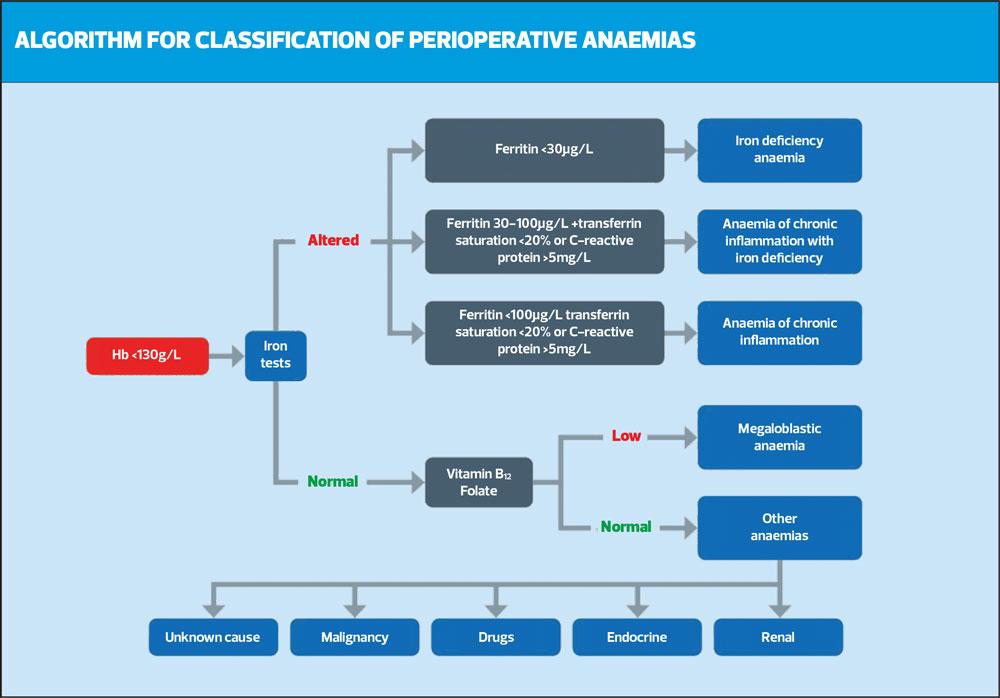
Assessment and investigation are key. A thorough medical history can give clues to any risk factors for or existing conditions contributing to anaemia. Recognising symptoms of anaemia is also a key part of clinical assessment, but it’s important to recognise that symptoms of anaemia can be vague and may apply to many conditions, including those that are pre-existing. The Anaemia in Primary Care Patients module can support you with a comprehensive list of symptoms to consider, as well as helping you to make the most of preliminary investigations such as full blood counts (FBC) to guide further investigations. For example, understanding mean cell volume (MCV) and identifying a macrocytic anaemia or microcytic anaemia can indicate the underlying cause. An MCV > 100 fL is a widely agreed defining value for macrocytic anaemia, which may indicate a folate or B12 deficiency, and therefore warrant blood tests to check folate levels. An MCV of <80 fL is a recognised value for identifying microcytic anaemia, which may indicate an iron deficiency directing your next steps to iron studies. It is important to recognise that there are many causes for macro- and microcytic anaemias, and normocytic levels do not exclude those causes, but this readily available information can be a useful tool for guiding next steps. Laboratory reference values can vary, so check with your testing laboratory.
Iron deficiency anaemia accounts for over half of all anaemia incidence. Understanding and interpreting iron studies, recognising functional and absolute iron deficiency and how to respond to it, are therefore vital in treating this prevalent and often correctable cause of anaemia. The primary care module guides practitioners through this complex and reportedly poorly understood topic, as well as compiling national guidance on who, when and where to refer, and indicating when secondary care investigation and treatment is required.
PRE-OPERATIVE ANAEMIA
Pre-operative anaemia management became a focus point for anaesthetists and pre-operative care with the publication of NICE Quality Standards for Blood Transfusion, supporting the correction of iron deficiency with pre- and postoperative supplementation. In 2017, the publication of the international consensus statement on the perioperative management of anaemia and iron deficiency6 provided further guidance for anaemia investigation, diagnosis, and management in the preoperative patient including, but not exclusive to, iron deficiency.
The reported prevalence of anaemia in the pre-surgical population varies widely, from 20-90%. Pre-operative anaemia is associated with increased postoperative morbidity and mortality risks, increased risk of transfusion requirements7 and potential for prolonged inpatient stay and recovery period. The benefits of effective preoperative management are significant for patients and the health service alike. Studies such as the recent PREVENTT trial,8 and feedback from the University Hospital of Wales at the recent NATA (Network for the Advancement of Patient Blood Management, Haemostasis and Thrombosis) symposium, both identify the need for early identification of anaemia to allow time for investigation, allowing maximum benefits of treatment prior to surgery, without causing delays to planned surgical intervention. The module aims to raise awareness of preoperative anaemia management and encourage consideration of anaemia in patients at the point of referral to surgical care, supporting pre-operative anaemia pathways and avoiding the risks associated with pre-operative anaemia.
Anaemia, and/or the presence of iron deficiency due to blood loss, requires careful history taking and thorough assessment as bleeding can be an indicator for various types of cancer. The NICE suspected cancer guideline provides guidance on how to proceed, refer, and investigate.9 For example, iron deficiency anaemia in the presence of gastrointestinal symptoms in the over 60’s may indicate the need for a GI 2-week cancer pathway referral. In the presence of active bleeding, anaemia management can be difficult until the source of bleeding is controlled, but iron replacement and medications to reduce blood loss and optimise haemoglobin production can help reduce the impact and risk of bleeding, especially in patients who may go on to require surgical intervention. The Anaemia in primary care patients module covers anaemia triggers for referral in more detail.
The most challenging patients can be those where achieving a definitive diagnosis of underlying cause is not deemed in their best interests or has proved elusive. The module aims to shed some light on how to approach the care of this specific group, focusing on identification of a therapeutic goal to support appropriate management, and guidance on how to monitor patients in this category, and when to escalate care.
The PBM team is currently working on further resources specifically aimed to support primary care practitioners in the management of anaemia. To contribute your thoughts and ideas for how these modules can support practice, please contact the PBM team via twitter @ PBM_NHS or at NHSBTCustomerService@
NHSBT.nhs.uk
To access the modules simply search ANAEMIA on eLfH or ESR. They can be completed as a set or stand-alone modules depending on your learning needs. You can also access the modules and other resources to support the care of patients with anaemia, including a Patient Blood Management toolkit and patient information leaflets at www.hospitalblood.co.uk/patient-services/patient-blood-management/
*Later guidance suggests that the haemoglobin threshold for iron deficiency anaemia should be the same for both men and women, Hb <130g/L
REFERENCES
1. Gardner W, Kassebaum N. Global, regional, and national prevalence of anemia and its causes in 204 countries and territories, 1990–2019. Current Developments in Nutrition 2020;4(Suppl 2): 830, https://doi.org/10.1093/cdn/nzaa053_035
2. Iron deficiency anaemia: overlooked and under-treated? Nursing Times, June 2015. Online only. https://www.nursingtimes.net/clinical-archive/haematology/iron-deficiency-anaemia-overlooked-and-under-treated-25-06-2015/
3. World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System; 2011 (WHO/NMH/NHD/MNM/11.1) https://apps.who.int/iris/handle/10665/85839
4. NHS England. The NHS long term plan; 2019. https://www.longtermplan.nhs.uk/
5. NICE Clinical Knowledge Summary. Anaemia – B12 and Folate deficiency. https://cks.nice.org.uk/topics/anaemia-b12-folate-deficiency/
6. Munoz M, Acheson AG, Auerbach M, et al. International consensus statement on the peri-operative management of anaemia and iron deficiency. Anaesthesia 2017;72:233-47
7. NICE QS138. Blood Transfusion Quality Standards; 2016 https://www.nice.org.uk/guidance/qs138
8. Richards T, Baikady RR, Clevenger B, et al. Preoperative intravenous iron to treat anaemia before major abdominal surgery (PREVENTT): a randomised, double-blind, controlled trial. The Lancet 2020;396,10259:1353-1361
9. NICE NG12. Suspected Cancer: recognition and referral; 2015 https://www.nice.org.uk/guidance/ng12
Related articles
View all Articles