Flu 2025-26: thinking ahead
Mandy Galloway, Editor
Getting ahead with preparations for this winter’s flu season will be vital if uptake figures are to be improved, especially among those in a clinical risk group
Practices have been urged to ensure that 100% of those eligible are offered flu vaccination in the 2025-26 season and to make firm plans to equal or improve uptake from previous years, especially in groups where uptake has usually been lower.1
These include people in clinical risk groups, health and social care workers, children aged 2 to 3 years, and pregnant women.1
Last winter was one of the worst on record in terms of patients admitted to hospital with flu – with 5.408 patients a day in hospital with flu in the first week of January 2025 alone.2
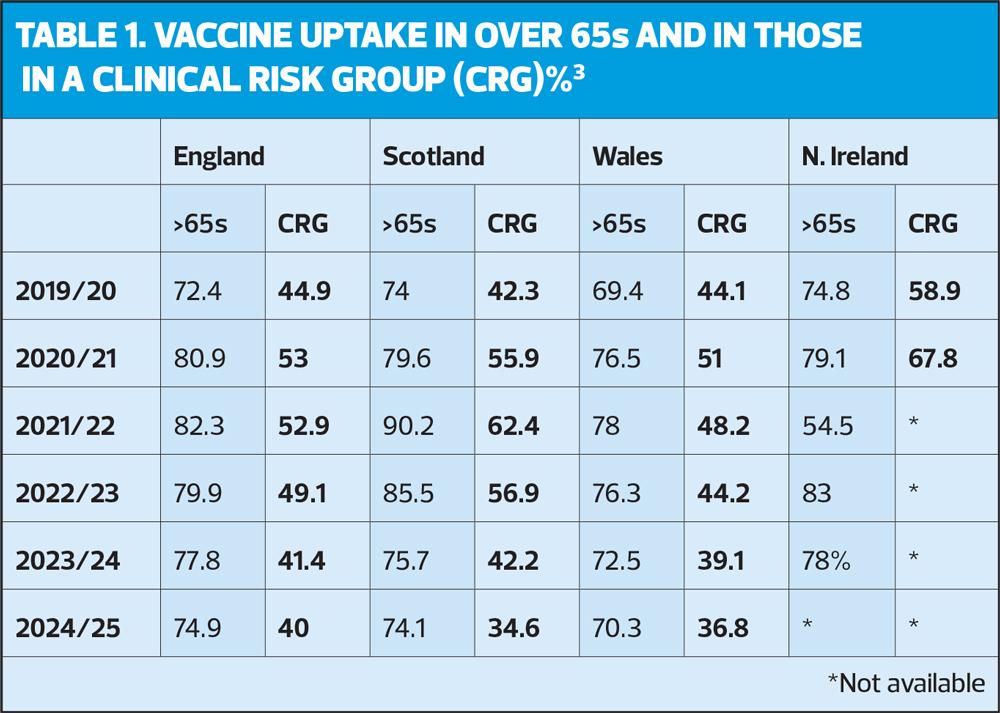
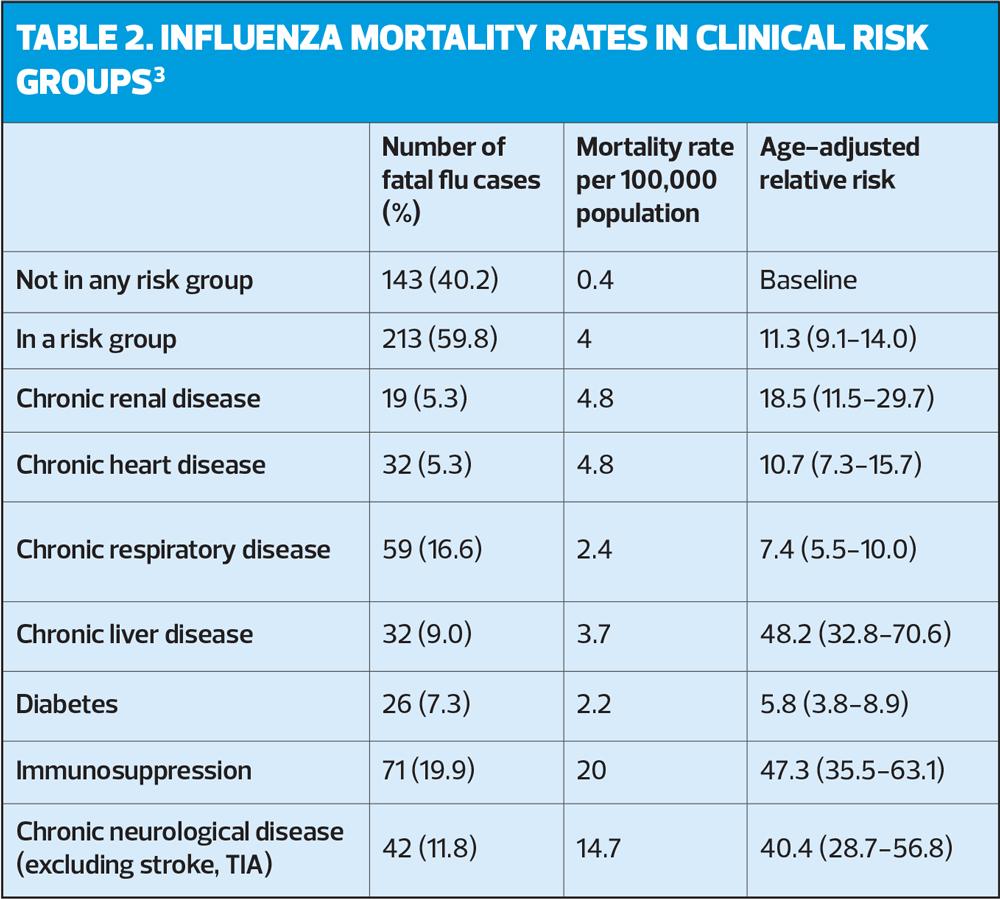
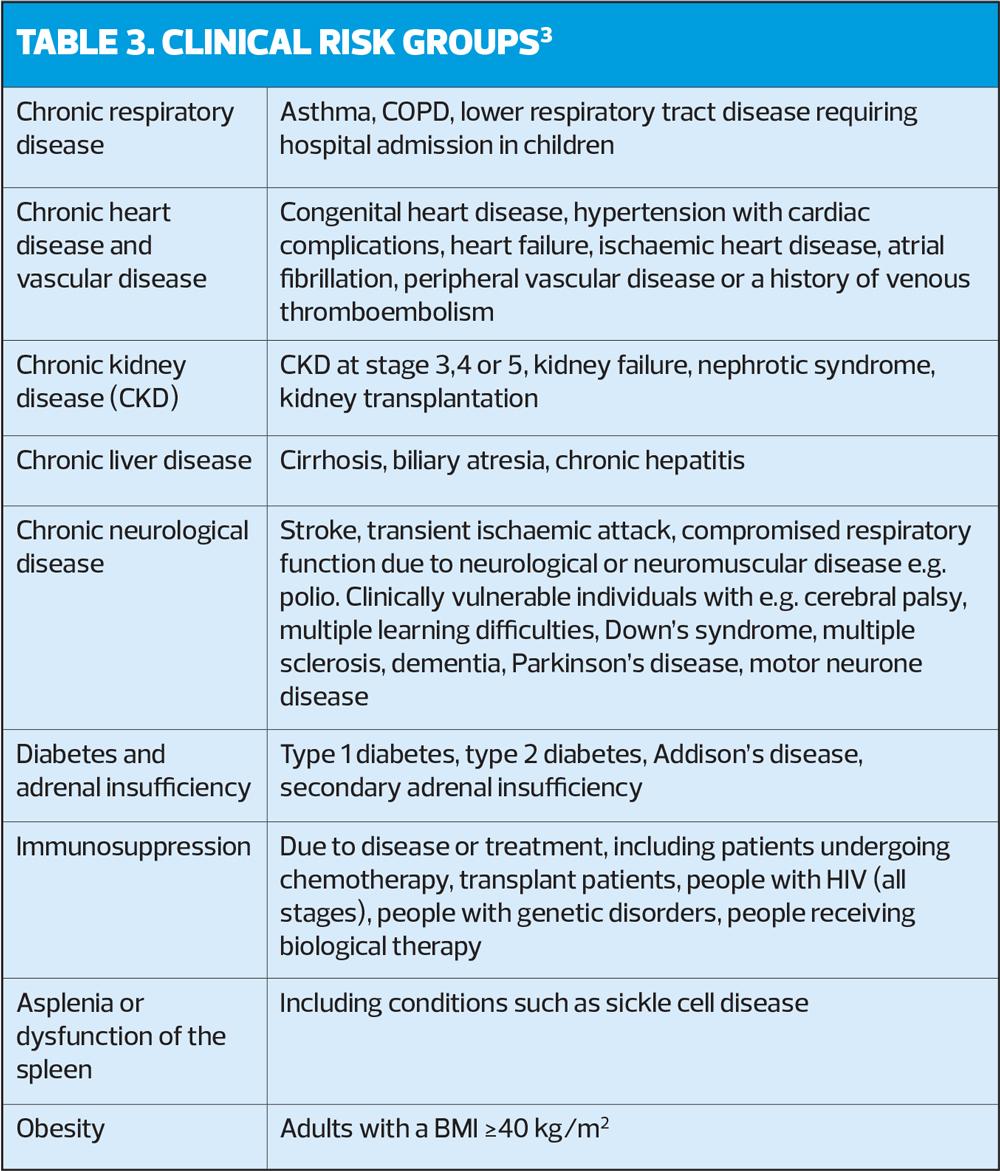
Historically, uptake in patients in clinical risk groups has fallen far short of that in the over-65s, as seen in Table 1.3 This is despite the markedly increased mortality rates among those with chronic diseases, including asthma, COPD, heart disease and diabetes (Table 2). As an aide-memoire, the full list of risk groups is given in Table 3.
Key reasons for the less-than-ideal uptake of vaccination in people in a clinical risk group include perceptions of the risk of flu, trust in flu vaccines, and the availability of reliable information.4
In a study from 2024,4 participants acknowledged that there was an increased risk for people with long-term conditions, but thought that the vaccine was for ‘older people’ – not for them, especially if they considered they were managing their condition well.
Others thought that possible side effects of vaccination were a significant issue or that vaccination would exacerbate their symptoms – sometimes on the basis of one personal experience of feeling ‘really poorly’ after a flu jab.4
Another participant commented that while they received text reminders from their GP practice every year, this was only to boost the numbers. ‘They obviously have to get as many people vaccinated as possible – that’s their target.’ And comments from HCPs, such as ‘You should get your flu vaccine’ were not enough to help them make an informed decision.4
HCPs who took part in the study said that time constraints and concerns about vaccine supplies made it difficult to offer vaccination opportunistically. They also pointed out the lack of information about the importance of flu vaccination during the course of self-management and education programmes.4
However, the likelihood of accepting vaccination increases with the frequency of contact with healthcare professionals, so closer attention to how and why people in at-risk groups come into contact with their healthcare teams could help to improve vaccine delivery to these groups.4
The authors therefore recommend integrating flu vaccination discussions and delivery in hospital settings, particularly at the point of discharge, and identifying other patient touchpoints when vaccination could be offered.4
However, there is evidence from the flu vaccination in pregnancy programme that even this approach is not always effective. Uptake among pregnant women is difficult to estimate but the most recent figures suggest that only around a third of pregnant women (35%) were vaccinated against flu in 2022-23, with the highest uptake seen in 2017-18, when less than half (47%) had their flu jab.3
MAXIMISING UPTAKE
NICE published guidance on maximising uptake in 2018, but the basic principles remain unchanged, so it has not been updated.5
Take home points include:
- Raise awareness among practice staff (and staff in secondary care) of the importance of flu vaccination for at-risk groups, and provide information on identifying eligible patients
- Optimise opportunities to raise awareness among eligible people, including discussing vaccination with pregnant women during antenatal appointments and people booking GP or other clinical appointments
- Give eligible people (or their parents or carers if appropriate information on:
- How people get flu
- How serious flu and its complications can be
- How flu can be worse in people with a long term condition, even if that condition is well managed
- That flu vaccination is safe
- That flu vaccination will not give them flu!
- That they should get the flu vaccination every year, as soon as it becomes available
Dr Julie Yates, Deputy Director, Immunisation Programmes at UKHSA, told Practice Nurse: ‘Practice nurses are the backbone of our whole immunisation programme, and we know that they are one of the most trusted sources of immunisation advice. They are uniquely positioned to make a real difference in improving vaccine uptake. Day-to-day, they have lots of different demands on their time but by ensuring that clinics are as flexible as possible and making sure people are offered the vaccine even if they are coming in for something else, we’re confident that we would start to see our uptake increase. As trusted healthcare professionals, nurses can play a vital role in reversing the downward trend.’
Naomi Watt, Healthcare Professional Engagement Manager at Asthma + Lung UK, said: ‘People living with a lung condition are more at risk of becoming seriously ill from flu, so it is important for healthcare professionals to remind vulnerable people like them to have their annual flu jab.
‘There are several reasons why someone may choose not to accept the flu jab. Complacency is a common factor, with some individuals underestimating the seriousness of flu or believing they are not at risk. Fear of side effects also plays a part, alongside the persistent myth that the flu vaccine can actually give you the flu. Others may have had the vaccine previously but felt it didn’t work for them, leading to doubts about its effectiveness.
‘Running a successful flu vaccination programme takes a bit of planning, but it can make a big difference. It starts with ordering vaccines in good time so everything’s ready to go. Then, it’s important to identify who’s eligible, so no one is missed. Deciding when to begin and how best to deliver the programme - whether in clinics, community centres, or through outreach - is key. Thinking about who will give the vaccines and working with community partners can also really help things run smoothly.
‘Clear invitations and easy-to-understand information make it more likely people will take up the offer of a flu vaccine too and keeping an eye on how things are going through audits and feedback, helps improve the vaccination programme year after year.
‘Inviting people who are eligible for their flu vaccination works best when the message comes from someone familiar, such as a known member of the surgery team, and personalising the invitation to reflect the individual’s circumstances can make it more meaningful. It’s also important to include information about the risks of not getting vaccinated, along with clear, educational messages to support informed decision-making.
‘Practice nurses should review the immunisation records of all newly registered children to ensure they’re up to date. For adults, every contact is a chance to offer the flu jab and check vaccination status. A consistent approach across the whole team helps to ensure no opportunity is missed.
‘To further encourage uptake, surgeries could offer early morning, evening and weekend flu clinics to fit around people’s work and commitments, as well as offering walk-in clinics, so there are less barriers to getting a flu vaccine.
‘Working with local support groups and using social prescribing networks to reach people in high-risk groups or groups that are harder to reach, such as those with mental health issues or who have English as a second language, is important too.’
OTHER CONSIDERATIONS
Timing
As last year, the start of the adult programme for 2025-26 will be from the beginning of October, but for children (including those in clinical risk groups) and pregnant women, vaccination should be offered from 1 September, or as soon as vaccine becomes available. The October start date for everyone else is because protection wanes over time, so it is preferable to start vaccinating as close as possible to the time when flu virus is in circulation (the typical peak is December or January). In addition, vaccination may be brought forward for some people who would benefit from it – e.g. before commencing immunosuppressive treatment.
The vaccine
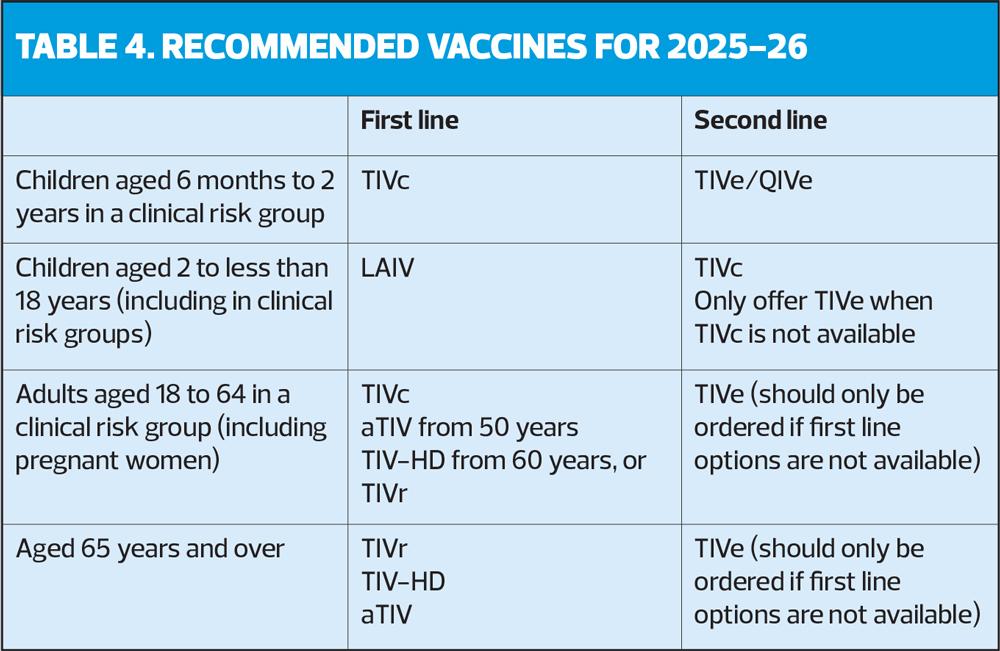
Following advice from the World Health Organization, stating that as the B/Yamagata virus lineages are no long circulating, they are unlikely to cause future epidemics, the Joint Committee on Vaccination and Immunisation recommends trivalent vaccines for the 2025-26 programme. Cell-cultured trivalent influenza vaccine (TIVc) is recommended first line. Adjuvanted influenza vaccine (aTIV) is recommended for adults over 50 years and over, with high-dose vaccine (TIV-HD) for those over 60. For adults over 65 years, the JCVI recommends the recombinant influenza vaccine (TIVr) as there is evidence of additional benefit compared with other products. Live attenuated influenza vaccine (LAIV) is recommended for children aged 2 to less than 18 years in eligible groups, with TIVc for children aged 6 months to 2 years (see Table 4).1
References
- UK Health Security Agency, NHS England, Department of Health & Social Care. National flu immunisation programme 2025 to 2026 letter; February2025. https://www.gov.uk/government/publications/national-flu-immunisation-programme-plan-2025-to-2026/national-flu-immunisation-programme-2025-to-2026-letter
- NHS England. NHS jabs tens of thousands more against flu than last winter. Press release; 14 January 2025. https://www.england.nhs.uk/2025/01/nhs-jabs-tens-of-thousands-more-against-flu-than-last-winter/
- UK Health Security Agency. Immunisation against infectious disease: The Green Book. Chapter 19, Influenza; 2023. https://www.gov.uk/government/publications/influenza-the-green-book-chapter-19
- Kasstan B, Lazurus R, Ali I, Mounier-Jack S. Improving influenza vaccine uptake in clinical risk groups… BMJ Public Health 2024;2:e000929
- NICE NG103. Flu vaccination: increasing uptake; 2018. https://www.nice.org.uk/guidance/ng103
Related articles
View all Articles