Lifestyle, health and wellbeing – COVID-19 and beyond
Rhian Last
Rhian Last
Nurse Educator
Associate, Experienced Led Care Programme
RCGP Yorkshire Faculty Board Member
Self Care Forum Board Member
As a society we have all had to make huge changes to the way we live and the way we work in order to stay safe and to curb the spread of coronavirus, but it seems the population is emerging from lockdown less healthy than before
The COVID-19 pandemic has the potential to change our daily living and working lives radically and permanently. As this country gradually emerges from lockdown we are moving towards a phase where services are starting to resume, albeit with restrictions. This is a good time to reflect on day-to-day life during the pandemic, and to consider the impact COVID-19 has had on our lifestyles, health and wellbeing and how research can help with forward planning.
After working through this article, you will be able to understand:
- The challenges when facilitating large scale change
- The social impact of the COVID-19 pandemic
- The need for a strategy for supporting lifestyle, health and wellbeing as we move from pandemic to recovery.
When lockdown measures were first imposed, COVID-19 had instilled fear and an appreciation of the seriousness of our situation so that in general people have adhered to lockdown rules, regulations and recommendations.
Irrespective of personal choices, our behaviour will be associated with social settings and when planning and implementing a large scale change with the intention of facilitating changes in behaviour, it is an imperative to give full consideration to the social, political and economic aspects and implications. This has all come into play with the government’s organisation and implementation of lockdown in England.
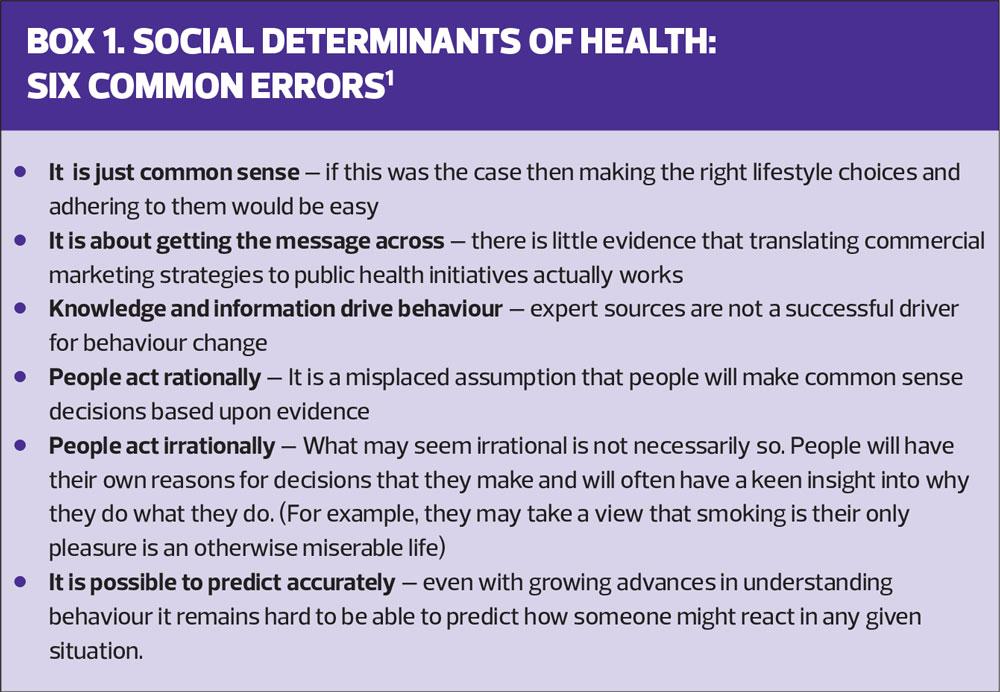
Changing long term, engrained behaviour is challenging and yields limited success. In their research paper,1 Michael Kelly and Mary Barker identify six common misconceptions which contribute to this lack of achievement (Box 1).
A recent YouGov survey in conjunction with a self-care app and website Your.MD found that harmful habits have emerged during the course of lockdown and identified that Britain is set to come out of lockdown unhealthier.2 Four out of five participants (81%) reported an increase in harmful habits including smoking, poor diet and staying up late. However, only a third (31%) of those surveyed plan to shake off their new habits after lockdown.2 The combination of these habits will, if sustained, lead to long-term implications for a person’s health, making lockdown a risk to health in its own right. It is those long term implications which give particular cause for concern.
COVID-19: IMPLICATIONS AND IMPACT
To gain an understanding of some of the implications and impact of COVID-19 we shall look at the following areas: obesity, health eating, exercise, smoking, alcohol, mental health and inequality.
Obesity
During the course of this pandemic it has become increasing apparent that outcomes for people who are obese and who contract COVID-19 are poor. It has been noted that obesity was surprisingly frequent in patients who were admitted to intensive care with COVID-19; the greater the BMI, the greater the severity of illness, with severe obesity significantly associated with the need for invasive mechanical ventilation.3 People with severe obesity who require intensive care can be difficult to intubate, diagnostic imaging can prove challenging and overall patient management can be problematic.
Healthy eating
Anecdotally, lockdown has seen an increase in people with more time and inclination for home cooking and this has perhaps provided an opportunity for us to eat more healthily. However, we are also able to tap into take away food services, and home deliveries of convenience foods. Lockdown stress, tedium and monotony can make some people turn to comfort eating. Interestingly, the YouGov survey reported that a third (33%) of the public say their eating habits are less healthy now than before lockdown began, with full-time students and 18-24-year-olds leading the trend (47% and 49% respectively).2 Could this be an under-representation?
A new survey from the British Nutrition Foundation confirms stress, anxiety, tiredness and boredom have contributed to unhealthy eating habits during lockdown.4 Nearly half (48%) of respondents said they were not motivated enough to eat well, while 63% admitted eating more out of boredom.4
Exercise
At the start of lockdown we seemed to be awash with free online classes to keep us fit and active. People were also encouraged to exercise outside, initially limited to just once a day though this limit has now been lifted. However, the YouGov survey found that in spite of the rise in online fitness classes and government encouragement to get outside to exercise, 30% of participants reported that they had become less active during lockdown.2 This is most notable in London, where 39% report that they are exercising less than before lockdown began.
Office of National Statistics (ONS) data on ‘Coronavirus and the Social Impacts on Great Britain’ reveal that across Great Britain, 42% of people are unable to exercise as normal, due to the implications of the virus.5 A global study undertaken by one of the leading wearables* companies would seem to support that while people are not able to undertake their normal daily activities they are finding alternative ways of getting exercise.6 What we need to take into account here is that people who use ‘wearables’ will generally already be taking some interest and action on their active health and so this is not necessarily a true representation of the public at large.
*Wearables – electronic technology or devices incorporated into items that can be comfortably worn on a body.
Smoking
Research has demonstrated that smoking has a likely association with negative progression and adverse outcomes of COVID-19.7 Another study has indicated that around 300,000 smokers may have quit due to COVID-19 fears.8 Although fear can be a motivator, it is important that we look at long term strategies to sustain this momentum.
Alcohol
When lockdown started many people reacted to the closure of bars and public houses by stocking up on alcohol to drink at home. The YouGov survey tells us that almost a fifth (17%) of people claim to have started drinking more than 14 units of alcohol a week (approx. two bottles of wine) during lockdown. This is more common in 35-44-year-olds (20% and 13% respectively).2
Just before the COVID-19 pandemic took hold in the UK, the Alcohol Health Alliance embarked on a commission on alcohol harm. The implications of COVID-19 on alcohol harm will create an imperative for action.9
Mental health
The impact of the COVID-19 pandemic is likely to lead to heightened anxiety, depression and engagement in harmful behaviours. A position paper in The Lancet Psychiatry articulates the need to explore the psychological, social, and neuroscientific effects of COVID-19 and sets out the immediate priorities and longer-term strategies for mental health science research.10 It states that multidisciplinary mental health science research must be central to the international response to the COVID-19.10
In a recent report on loneliness, the Royal College of Nursing noted that in recent decades loneliness has developed from a personal problem into a social epidemic. Anyone can be affected at any age and in any circumstance. For those in enforced isolation due to COVID-19 restrictions this will have a particular relevance. It is vital that nurses in all settings recognise loneliness and can respond accordingly with appropriate resources.11
INEQUALITIES AND COVID-19
The health gap between deprived and well off parts of the country has widened, and as we get through this pandemic, can only be expected to become worse. February 2020 saw the publication of the report Health Equity in England, The Marmot Review 10 Years On, with some salutary findings.12 Less than two months later, life in the UK changed dramatically. Many thousands have lost those dear to them and millions of people are facing hardship and uncertainty. This will take a toll on long term health and wellbeing.
Worryingly, it is children who are being acutely affected. The Trussell Trust have reported a 122% rise in emergency food parcels given to children from food banks in their network during the second half of March 2020, compared to the same period in 2019.13
There was widespread alarm recently when the English government announced that they would be stopping the school meals voucher service over the Summer holiday period. Thanks to a positive and powerful national campaign, driven by the Manchester United footballer, Marcus Rashford, this decision has been overturned. Rashford’s motivation was his own experience as the child of a single (devoted) parent where money was tight and getting food on the table a challenge.14
The COVID-19 pandemic, and the wider governmental and societal response, have brought health inequalities into sharp focus, according to a report by the Health Foundation.15 It states:
- People facing the greatest deprivation are experiencing a higher risk of exposure to COVID-19 and existing poor health puts them at risk of more severe outcomes if they contract the virus. This is exposing the structural disadvantage and discrimination faced by parts of the Black, Asian and Minority Ethnic (BAME) communities.
- The government and wider societal measures to control the spread of the virus and save lives now (including the lockdown, social distancing and cancellations to routine care) are exacting a heavier social and economic price on those already experiencing inequality.
- The consequences of this action, and the economic recession that is likely to follow, risk exacerbating health inequalities now and in years to come.
- As we move from crisis management to recovery, government, businesses and wider society all have a role to play in giving everyone the opportunity to live a healthy life.
- Restoring the nation to good health will require a new social compact, backed by a national cross-departmental health inequalities strategy. Action needed will include protecting incomes, improving the quality of jobs and homes, and supporting critical voluntary and community services.15
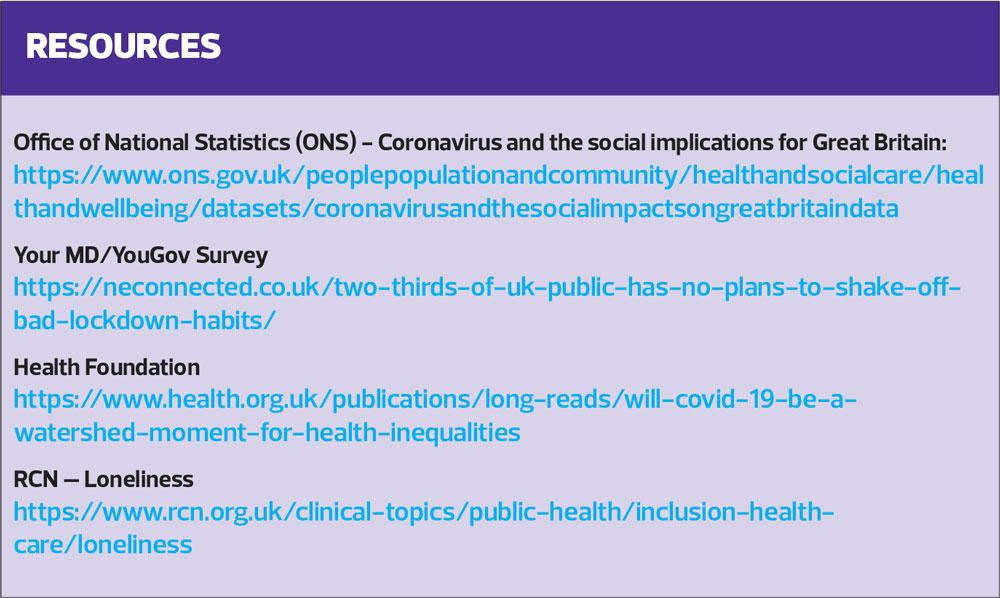
You can access the full report here:
HOW CAN PRIMARY CARE CONTRIBUTE?
By monitoring national and local statistics Primary Care Networks (PCNs) can develop a greater understanding of how COVID-19 is impacting on people’s lifestyle, health and wellbeing. This will help with strategy development and robust forward planning as we continue to move out of lockdown and on to recovery.
General practice nurses can gain far greater insights into how life is in general for their patients by adopting a holistic approach, through taking a social history in addition to a clinical history during consultations.16 This should be intrinsic to a practice nurse’s day-to-day work,
particularly now, as people come to terms with the huge challenges and changes that have swept through all our lives due to COVID-19.
SUMMARY
The COVID-19 pandemic has impacted on our day-to-day living and this has brought challenges to our lifestyle, health and wellbeing. Our behaviour is influenced by social settings as well as personal choice. Appreciating the six common errors that contribute to a failure to change will help us to identify meaningful ways forward that will lead to sustained behaviour change and improved lifestyle, health and wellbeing as we move out of pandemic and towards recovery.
REFERENCES
1. Kelly MP, Doohan E. The Social Determinants of Health. In Global Health: Diseases, Programs, Systems, and Policies, 3rd ed, Ed. Michael H Merson, Robert E. Black, and Anne J. Mills, pp75–113. Burlington, MA: Jones and Bartlett;2012
2. Your MD. Two-thirds of UK public has no plans to shake off bad lockdown habits; 2020. https://neconnected.co.uk/two-thirds-of-uk-public-has-no-plans-to-shake-off-bad-lockdown-habits/
3. Simonnet A, Chetboun M, Poissy J, et al. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-COV-2) requiring invasive mechanical ventilation. Obesity Journal. ePub April 2020. https://onlinelibrary.wiley.com/doi/epdf/10.1002/oby.22831
4. British Nutrition Foundation. BNF survey reveals stress, anxiety, tiredness and boredom are the main causes of unhealthy eating habits in lockdown; Press release, 22 June 2020.
5. Office for National Statistics. Coronavirus And The Social Impacts On Great Britain - Office For National Statistics; 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandwellbeing/datasets/coronavirusandthesocialimpactsongreatbritaindata
6. Garmin. The Impact Of The Global Pandemic On Human Activity: A Global Perspective – Garmin Blog; 2020. https://www.garmin.com/en-GB/blog/the-impact-of-the-global-pandemic-on-human-activity-a-global-perspective/
7. Vardavas C, Nikitara K. COVID-19 and smoking: A systematic review of the evidence. Tobacco Induced Diseases 2020;18(March):20. http://www.tobaccoinduceddiseases.org/COVID-19-and-smoking-A-systematic-review-of-the-evidence,119324,0,2.html
8. Action on Smoking and Health. More than 300,000 UK smokers may have quit owing to COVID-19 fears. ASH Daily News for 4 May 2020. https://ash.org.uk/media-and-news/ash-daily-news/ash-daily-news-for-4-may-2020/
9. Finlay I, Gilmore I. COVID-19 and alcohol—a dangerous cocktail. BMJ 2020:369:m1987.
10. Holmes E, O'Connor R, Perry V, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. The Lancet Psychiatry 2020; 7(6):547-560.
11. Royal College of Nursing. Loneliness; 2020. https://www.rcn.org.uk/clinical-topics/public-health/inclusion-health-care/loneliness
12. Marmot M. Health Equity In England: The Marmot Review 10 Years On; 2020. https://www.health.org.uk/publications/reports/
the-marmot-review-10-years-on
13.The Trussell Trust. 2020. Food Banks Report Record Spike In Need As Coalition Of Anti-Poverty Charities Call For Strong Lifeline To Be Thrown To Anyone Who Needs It; 2020 https://www.trusselltrust.org/2020/05/01/coalition-call
14.BBC News. Food Voucher U-Turn After Rashford Campaign; 17 June 2020 https://www.bbc.co.uk/news/uk-53065806
15. The Health Foundation. Will COVID-19 Be A Watershed Moment For Health Inequalities? 2020 https://www.health.org.uk/publications/long-reads/will-covid-19-be-a-watershed-moment-for-health-inequalities
16. Last R. Health Equity. Practice Nurse 2020;50(4):30-34
Related articles
View all Articles