What lies beneath: diabetes and multi-morbidity
Beverley Bostock-Cox
Beverley Bostock-Cox
RGN MSc MA QN
Nurse Practitioner Mann Cottage Surgery, Moreton in Marsh
Primary Care Cardiovascular Society Committee Member
People with type 2 diabetes are at high risk of a wide range of comorbidities. In this article we consider how concurrent conditions can complicate their management and discuss the evidence for interventions to improve the holistic health of people living with complex diabetes
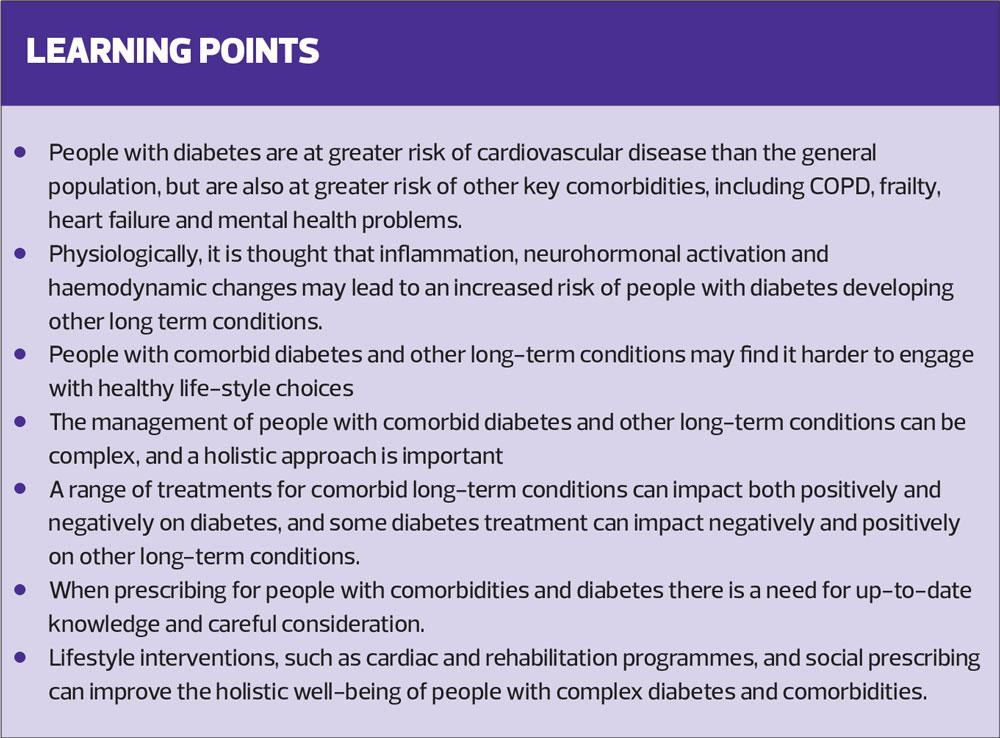
As the prevalence of overweight and obesity increases so too does the incidence of type 2 diabetes (T2D), and along with that the risk of vascular complications.1 T2D is known to lead to a higher risk of both macrovascular and microvascular complications, and this risk can be minimised or avoided through good control of blood glucose levels and effective management of lipid levels and blood pressure.1 However, people with T2D are also more likely to suffer comorbidities such as chronic obstructive pulmonary disease (COPD), frailty, heart failure and mental health problems, all of which can add an extra layer of complexity for healthcare professionals supporting them to optimise their well-being.
DIABETES AND THE RISK OF COMORBIDITIES
People with a diagnosis of T2D are at increased risk of other health problems. The reasons for this are multi-factorial and include:
- Ageing – when comorbidities become more likely
- Physiological factors
- Lifestyle factors.
Physiologically, it is thought that inflammation, neurohormonal activation and haemodynamic changes may lead to an increased risk of people with diabetes developing other long term conditions.2 However, lifestyle factors may also play a part. People with a long term condition may find it more challenging to make healthy choices with regard to diet, exercise, smoking cessation and alcohol regulation.3 The individual with COPD, for example, may find that breathlessness limits activity levels and increased dissatisfaction with quality of life makes quitting smoking harder to achieve. As a result, weight may increase, along with diabetes risk and the risk of cardiovascular complications. This underlines the importance of treating the person with comorbid conditions holistically, because very often, one condition is affecting (and is affected by) another.
COPD
People with diabetes are more likely than the general population to be diagnosed with COPD and other lung conditions.4 This is thought to be related to inflammation and to the effects of diabetes on the pulmonary vasculature.4 There is also an interesting relationship between smoking, T2D and respiratory disease, linked to inflammatory processes.5,6
The pulmonary complications of diabetes are not often discussed but they have been shown to be affected positively and negatively by different hypoglycaemic drugs. For example, metformin seems to have a therapeutic effect in diabetic lung diseases, whereas insulin has the potential to exacerbate lung diseases.4 The relationship between diabetes and COPD works the other way too. It has been previously shown that the use of high dose inhaled corticosteroids (ICS) in the management of COPD increases the risk of developing T2D by 64%.7 In those patients who already have diabetes, the use of ICS therapy in the management of COPD may have a negative impact on diabetes control. A recent study of people with comorbid T2D and COPD showed that they had greater risk of diabetes progression if they were on higher dose ICS therapy.8
High dose ICS, used to control COPD, and frequent courses of oral corticosteroid (OCS) therapy for COPD exacerbations are also likely to increase the risk of cardiovascular complications of diabetes. Steroid therapy is now recognised as a risk factor for cardiovascular disease (CVD) in the QRisk 3 assessment tool,9 so people with diabetes using high dose ICS, or having repeated courses of OCS can add another potential cardiovascular risk factor to those resulting from their diabetes. OCS can also lead to a deterioration in diabetes control, with the associated increased risk of potential short- and long-term side effects.10
In this situation, it is important to consider whether giving rescue packs which include OCS is appropriate and if so, to give extensive education and support about when to initiate them and how to monitor blood glucose readings at home. People on high dose ICS therapy should be reassessed to determine whether any ICS is needed, as both NICE and GOLD guidance advise that the role of ICS therapy is far less certain than previously thought, mainly because of changes in the perception of the risk: benefit ratio.11,12 If the patient does require ICS-containing inhalers, lower doses should be aimed for, avoiding inhalers with, for example, fluticasone proprionate at doses at 1000mcg per day, even though these are licensed.7
Another area where diabetes and COPD overlap is with regard to the impact of statins. People with diabetes and a cardiovascular risk score of 10% or more, are normally offered a statin to reduce LDL cholesterol and to reduce their future risk of a cardiovascular event.9 However, research has also shown that the use of statins in people with COPD and diabetes, seems to modify the risk of acute exacerbations of COPD. A systematic review and meta-analysis identified a protective effect of statin treatment on the risk of COPD exacerbation; those patients receiving statins had both a lower risk of having a mild COPD exacerbation and a lower risk of a severe COPD exacerbation requiring hospitalisation.13 Overall, however, the evidence is not strong enough to make population-based recommendations about giving statins to everyone with COPD. Nonetheless, this review and analysis identifies an unexpected link, thought to be related to the anti-inflammatory effects of statin therapy.14
Lifestyle approaches to managing diabetes can also be effective in improving COPD outcomes. People should be encouraged to engage with lifestyle change by highlighting the dual benefits of smoking cessation, increased activity levels and healthy eating for both conditions. In COPD, a diet rich in anti-oxidants has been linked to a lower rate of exacerbations,15 and pulmonary rehabilitation programmes, which include physical activity, are known to lead to improvements in COPD symptoms, lung function, exacerbation risk and mental health.16 Encouraging people with COPD to attend a pulmonary rehabilitation programme will offer broader benefits if they also have diabetes and this may encourage those who are reluctant to attend to reconsider.
FRAILTY
As the UK population ages the competing challenges of hitting targets (HbA1c, blood pressure and lipids) and minimising the risk of ‘going too low’ (especially through the use of more and more medication with the associated increased risk of adverse drug reactions) become more complex. This challenge may be particularly difficult if the older person being treated for diabetes also suffers from frailty.
Recommendations regarding targets for people with type 2 diabetes from the American Diabetes Association and the European Society for the Study of Diabetes (ADA/EASD)* take a much more tailored and personalised approach to glycaemic control than previous guidelines, factoring in issues such as established vascular disease, avoidance of hypoglycaemia, and the impact of comorbidities.17 This consensus statement recognises the importance of offering a patient-centred approach to care, including when it comes to making choices about glucose-lowering medication. This is a useful resource for people wishing to deliver ethical healthcare as the National Institute for Health and Care Excellence (NICE) has not yet published its updated guidance on the management of diabetes,18 and local formularies may focus more on cost than comorbidities (See Further reading).
Although some areas may have their own guidance on frailty and diabetes, a ‘Frailty toolkit’, developed by Strain et al provides pragmatic advice about supporting people with diabetes and frailty more holistically.19 Their guidance suggests that frailty assessments for people with diabetes should consider any history of falls, mobility issues, limitations when performing activities of daily living, weight loss or fatigue. These considerations can help to personalise care, particularly when it comes to HbA1c and blood pressure targets, but also when it comes to decisions about statin therapy and lifestyle interventions, such as nutritional requirements and help to become more active, safely. Any frailty issues that have been identified can then lead to referrals for support from the multi-disciplinary team, such as dietitians to improve overall nutritional status, and physiotherapists and occupational therapists to optimise physical activity capacity.
The ADA/EASD guidance reminds clinicians that avoidance of hypoglycaemic episodes is a key consideration in the population who have diabetes and frailty, so sulfonylureas and insulin should ideally be avoided in this group.17 If insulin is required, a harm reduction approach should be taken to optimise the risk: benefit ratio.
The moral of the diabetes and frailty story is that standard rules do not apply and the age old advice to ‘First do no harm’ must take priority.*
* The ADA/EASD have updated their guidance on drugs to be used in type 2 diabetes to reduce the risk of developing, or progression of, cardiovascular and renal complications – see Further reading.
HEART FAILURE
The risk of developing heart failure is significantly greater in people with diabetes than it is in the general population, irrespective of the individual’s cardiovascular status.20 Although hypertension and coronary heart disease are known to be risk factors for heart failure, people with diabetes are at higher risk purely by virtue of their diabetes diagnosis. As mentioned above, there are several reasons for this: neurohormonal and haemodynamic changes but also structural changes that can occur in the heart as a result of having diabetes.21
It is important to always remain alert to the possibility of heart failure in people living with diabetes. However, the common symptoms (breathlessness, oedema and fatigue) are often seen in a range of other conditions, both significant and insignificant. It may not always be obvious. Also, in people with diabetes with comorbid COPD, symptoms of heart failure may be mistaken for an exacerbation of COPD.
Decisions about medication should be made carefully in people with, or at risk of heart failure. Pioglitazone is contraindicated in heart failure, but other drugs may have a positive effect. The role of the sodium-glucose transport protein 2 inhibitor (SGLT2i) drugs is increasingly being scrutinised in a range of comorbid conditions, because they seem to be offering benefits beyond glycaemic control.
The evidence for SGLT2i
In the CVD REAL study, people with T2D, with or without existing cardiovascular disease (CVD), were assessed for rates of hospitalisation for heart failure and cardiovascular death. Half were on an SGLT2i and the use of this class of drug (irrespective of which one was used) led to a 39% lower risk of hospitalisation for heart failure (hHF).22
In a further study, OBSERVE 4D, new users of the SGLT2i canagliflozin had:
- A 61% reduction in their risk of hHF when compared with new users of non-SGLT2i therapies in the overall population, and
- A 56% reduction in risk among those with established cardiovascular disease.23
The DECLARE TIMI study also demonstrated the importance of SGLT2i therapy in reducing heart failure risk. It demonstrated around a 27% relative risk reduction in hHF in a population in which the majority did not have a history of heart failure.24
The DAPA-HF trial included people, with and without diabetes, who had heart failure with reduced ejection fraction. The trial showed that the risk of worsening heart failure or death from cardiovascular causes was lower among those who received dapagliflozin than among those who received placebo, regardless of the presence or absence of diabetes.25
Considering the morbidity and mortality burden of heart failure, the findings of these trials are highly significant.
ACE inhibitors
ACE inhibitors are recommended for both hypertension management in diabetes,26 and to improve symptoms and disease outcomes in chronic kidney disease and heart failure.27,28
In summary, the overall advice for someone with diabetes and heart failure would be to optimise heart failure drugs, and consider diabetes medication choices carefully. The 2019 update to ADA/EASD guidelines, however, is more specific. It suggests the addition of an SGLT2i in patients with diabetes and heart failure as there is evidence of cardiovascular benefit for patients with heart failure, irrespective of their baseline or target HbA1c level.29 There may also be a developing role for SGLT2i drugs in a broader population in the future, including those with heart failure who do not have diabetes.25
In terms of life-style modification, cardiac rehabilitation (CR) referrals can now be made for people with heart failure (they were often excluded in the past) and engaging with a CR programme is likely to offer additional benefits for the diabetes, too.
MENTAL HEALTH PROBLEMS
Clinically significant depression is present in around one in four people with T2D,30 and the relationship is bi-directional. Research indicates that people with a diagnosis of depression have an increased risk of insulin resistance, raised blood glucose levels and microvascular and macrovascular complications.30,31 Although the direct cause of this relationship between diabetes and depression is not fully understood, it is thought that autonomic and hypothalamic-pituitary-adrenal axis dysregulation, weight gain, inflammation, and hippocampal structural alterations may all play a part.32
Mental health problems can make it far harder for people to engage in healthy lifestyle choices; a healthy diet, physical activity, smoking cessation and regulating alcohol intake.3 It is therefore important to both diagnose and treat depression effectively. Diagnosis can be aided by the use of screening tools, and treatment may consist of a combination of pharmacotherapy and behavioural support. Cognitive behavioural therapy can also lead to improvements in glycaemic control.
General practice nurses have a key role in identifying psychological and/or psychiatric problems in people with diabetes and ensuring that they have access to appropriate levels of psychological support to help manage their diabetes, not least because the incidence of CVD is already higher in people with psychiatric disorders compared with the general population.33 Engagement with people who have mental health problems can be challenging on many different levels but a multi-disciplinary, patient focused approach may help to ensure better outcomes (and even improved prevention of CVD and T2D in these patients).34 Social prescribing may be helpful for people with mental health problems, with or without a long term condition.35
CONCLUSION
People with diabetes are known to be at increased risk of CVD but may also run the risk of developing other long term conditions when compared with the rest of the population. There are many possible reasons for this, based on neurohormonal responses, vascular changes and inflammation. However, there is a range of interventions, pharmacological and lifestyle-related, which can have a positive impact on diabetes and other conditions, thus offering extra benefits beyond those which are known for treating diabetes alone.
General practice nurses are optimally placed to recognise the potential risk of the existence of comorbid conditions in people with diabetes and also to support people to understand how some drugs and lifestyle changes can positively affect a range of outcomes in people diagnosed with multi-morbidity.
REFERENCES
1. Diabetes UK. Diabetes Facts and Stats. 2019 https://www.diabetes.org.uk/professionals/position-statements-reports/statistics
2. van der Wal HH, van Deursen VM, van der Meer P, et al. Comorbidities in heart failure. Handb Exp Pharmacol 2017;243:35–66 doi:10.1007/164_2017_27
3. Mulligan K, McBain H, Lamontagne-Godwin F, et al. Barriers and enablers of type 2 diabetes self-management in people with severe mental illness. Health Expect 2017;20(5): 1020–1030. doi:10.1111/hex.12543
4. Khateeb J, Fuchs E, Khamaisi M. Diabetes and lung disease: a neglected relationship. Rev Diabet Stud 2019;15:1-15. doi:10.1900/RDS.2019.15.1
5. Wannamethee SG, Shaper AG, Perry IJ, et al. Smoking as a modifiable risk factor for type 2 diabetes in middle-aged men. Diabetes Care 2001;24(9):1590–1595. doi:10.2337/diacare.24.9.1590
6. Song Y, Klevak A, Manson JE, et al. Asthma, chronic obstructive pulmonary disease, and type 2 diabetes in the Women's Health Study. Diabetes Res Clin Pract 2010;90(3):365–371. doi:10.1016/j.diabres.2010.09.010
7. Suissa S, Kezouh A, Ernst P. Inhaled corticosteroids and the risks of diabetes onset and progression. Am J Med 2010;123(11):1001-6. doi: 10.1016/j.amjmed.2010.06.019.
8. Price D, Russell R, Mares R, et al. Metabolic effects associated with ICS in patients with COPD and comorbid type 2 diabetes: a historical matched cohort study. PLoS One 2016;11(9): e0162903. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5033451/#!po=67.0732
9. Hippisley-Cox J, Coupland C, Brindle P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: prospective cohort study. BMJ 2017;357, j2099. doi:10.1136/bmj.j2099
10. Rogers M, Lin P, Nallamothu BK, et al. Longitudinal study of short-term corticosteroid use by working-age adults with diabetes mellitus: risks and mitigating factors. J Diabetes 2018;10(7):546–555. doi:10.1111/1753-0407.12631
11. NICE NG115. Chronic obstructive pulmonary disease in over 16s: diagnosis and management. 2018 (updated 2019) https://www.nice.org.uk/guidance/NG115
12. GOLD. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease: 2020 report; 2019. https://goldcopd.org/wp-content/uploads/2019/11/GOLD-2020-REPORT-ver1.0wms.pdf
13. Cao C, Wu Y, Xu Z, et al. The effect of statins on chronic obstructive pulmonary disease exacerbation and mortality: a systematic review and meta-analysis of observational research. Sci Rep 2015;5:16461. doi:10.1038/srep16461
14. Liao JK, Laufs U. Pleiotropic effects of statins. Annu Rev Pharmacol and Toxicol 2005;45:89–118
15. Scoditti E, Massaro M, Garbarino S, et al. Role of diet in chronic obstructive pulmonary disease prevention and treatment. Nutrients 2019;11(6): 1357. doi:10.3390/nu11061357
16. Early F, Wellwood I, Kuhn I, et al. Interventions to increase referral and uptake to pulmonary rehabilitation in people with COPD: a systematic review. Int J Chron Obstruct Pulmon Dis 2018;13: 3571–3586. doi:10.2147/COPD.S172239
17. Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). http://diabetologia-journal.org/wp-content/uploads/2018/09/EASD-ADA.pdf
18. NICE NG28. Type 2 diabetes in adults: management. 2015 (updated 2019) https://www.nice.org.uk/guidance/ng28/resources/type-2-diabetes-in-adults-management-pdf-1837338615493
19. Strain WD, Hope SV, Green A et al. Type 2 diabetes mellitus in older people: a brief statement of key principles of modern day management including the assessment of frailty. A national collaborative stakeholder initiative. Diabet Med 2018;35(7):838–845. doi:10.1111/dme.13644
20. Lehrke M, Marx N. Diabetes mellitus and heart failure. Am J Cardiol 2017;120(1S):S37–S47. doi:10.1016/j.amjcard.2017.05.014
21. Ofstad AP, Atar D, Gullestad L, et al. The heart failure burden of type 2 diabetes mellitus-a review of pathophysiology and interventions. Heart Fail Rev 2018;23(3):303–323. doi:10.1007/s10741-018-9685-0
22. Kosiborod M, Cavender MA, Fu AZ, et al. Lower risk of heart failure and death in patients initiated on sodium-glucose cotransporter-2 inhibitors versus other glucose-lowering drugs: The CVD-REAL Study (Comparative Effectiveness of Cardiovascular Outcomes in New Users of Sodium-Glucose Cotransporter-2 Inhibitors). Circulation 2017;136:249–259. DOI: 10.1161/CIRCULATIONAHA.117.029190
23. Ryan PB, Buse JB, Schuemie MJ, et al. Comparative effectiveness of canagliflozin, SGLT2 inhibitors, and non-SGLT2 inhibitors on the risk of hospitalization for heart failure and amputation in patients with type 2 diabetes mellitus: a real-world meta-analysis of 4 observational databases (OBSERVE-4D). Diabetes Obes Metab 2018;20(11):2585-2597 https://onlinelibrary.wiley.com/doi/full/10.1111/dom.13424
24. Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2019;380(4): 347–357. doi:10.1056/NEJMoa1812389
25. McMurray J, Solomon SD, Inzucchi SE, et al for the DAPA-HF Trial Committees and Investigators. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med 2019;381(21):1995–2008. doi:10.1056/NEJMoa1911303
26. NICE NG136. Hypertension in adults: diagnosis and management; 2019 https://www.nice.org.uk/guidance/ng136
27. NICE CG182. Chronic kidney disease in adults: assessment and management; 2015 https://www.nice.org.uk/guidance/cg182
28. NICE NG106. Chronic heart failure in adults: diagnosis and management; 2018 https://www.nice.org.uk/guidance/ng106
29. Buse JB, Wexler DJ, Tsapas A et al. 2019 update to: Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2019. https://care.diabetesjournals.org/content/early/2019/12/18/dci19-0066
30. Semenkovich K, Brown ME, Svrakic DM, Lustman PJ. Depression in type 2 diabetes mellitus: prevalence, impact, and treatment. Drugs 2015;75(6):577–587. doi:10.1007/s40265-015-0347-4
31. Campayo A, Gómez-Biel CH, Lobo A. Diabetes and depression. Curr Psychiatry Rep 2011;13(1);26–30. doi:10.1007/s11920-010-0165-z
32. Joseph JJ, Golden SH. Cortisol dysregulation: the bidirectional link between stress, depression, and type 2 diabetes mellitus. Ann N Y Acad Sci 2017;1391(1): 20–34. doi:10.1111/nyas.13217
33. Bent-Ennakhil N, Périer CM, Sobocki P, et al. Incidence of cardiovascular diseases and type-2-diabetes mellitus in patients with psychiatric disorders. Nord J Psychiatry 2018;72(7):455–461. doi:10.1080/08039488.2018.1463392
34. Mulligan K, McBain H, Lamontagne-Godwin F, et al. Barriers to effective diabetes management - a survey of people with severe mental illness. BMC Psychiatry 2018;18(1):165. doi:10.1186/s12888-018-1744-5
35. Moffatt S, Steer M, Lawson S, et al. Link worker social prescribing to improve health and well-being for people with long-term conditions: qualitative study of service user perceptions. BMJ open 2017;7(7): e015203. doi:10.1136/bmjopen-2016-015203
Related articles
View all Articles