Optimising the nutritional status of patients with COPD
DR ANNE HOLDOWAY
DR ANNE HOLDOWAY
Consultant Dietitian and
Chair of the Malnutrition Pathway
HILARY FRANKLIN
Healthcare Communications Consultant and Malnutrition Pathway Co-ordinator
Practice Nurse 2024;54(2:20-22
Poor nutritional intake is common in patients with COPD, and low body mass in COPD patients is associated with worse outcomes: optimising nutrition and encouraging activity are therefore essential elements of comprehensive care
Chronic obstructive pulmonary disease (COPD) is primarily managed in the community and accounts for around 1.4 million GP consultations a year.1 Malnutrition is highly prevalent in COPD, with a global prevalence reported at 30% and an at-risk prevalence of 50%.2 Loss of muscle and strength impairs both respiratory and physical function and negatively impacts health status.2 A low BMI and low fat-free mass are associated with worse outcomes in people with COPD,3 and therefore optimising nutrition and preserving lean tissue through adequate protein combined with resistance activity should be an integral component of care.
The aetiology of malnutrition in COPD is often complex and multi-factorial,4 arising from symptoms associated with the disease such as breathlessness and inflammation (especially during exacerbations), societal and environmental factors (income and the ability to acquire, prepare and consume an adequate diet) and issues associated with increasing age (loss of taste, poor dentition or anorexia).
The nutritional needs of individuals with COPD can vary over the course of the disease. On diagnosis, for example, some individuals may be overweight, obese or pre-diabetic, necessitating dietary advice to improve metabolic health and reduce the risk of cardiovascular disease. During acute exacerbations, and as the disease progresses, individuals are at increasing risk of undernutrition (commonly referred to as malnutrition), unplanned weight loss and muscle loss. Malnutrition and poor nutritional intake, left unaddressed, can hamper recovery and impact on long-term health and wellbeing.
Malnutrition is commonly defined as a deficiency, excess or imbalance of a wide range of nutrients, resulting in a measurable adverse effect on body composition, function and clinical outcome.5 Although malnourished individuals can be under or overnourished, ‘malnutrition’ is often used synonymously with ‘undernutrition’. Malnutrition in COPD is a predictor of increased healthcare use including hospitalisation and increased length of hospital stay.6,7 Taking time to consider the nutritional care of people with COPD has the potential not only to improve an individual’s quality of life but also more effectively manage the health and care costs of those affected.8-11
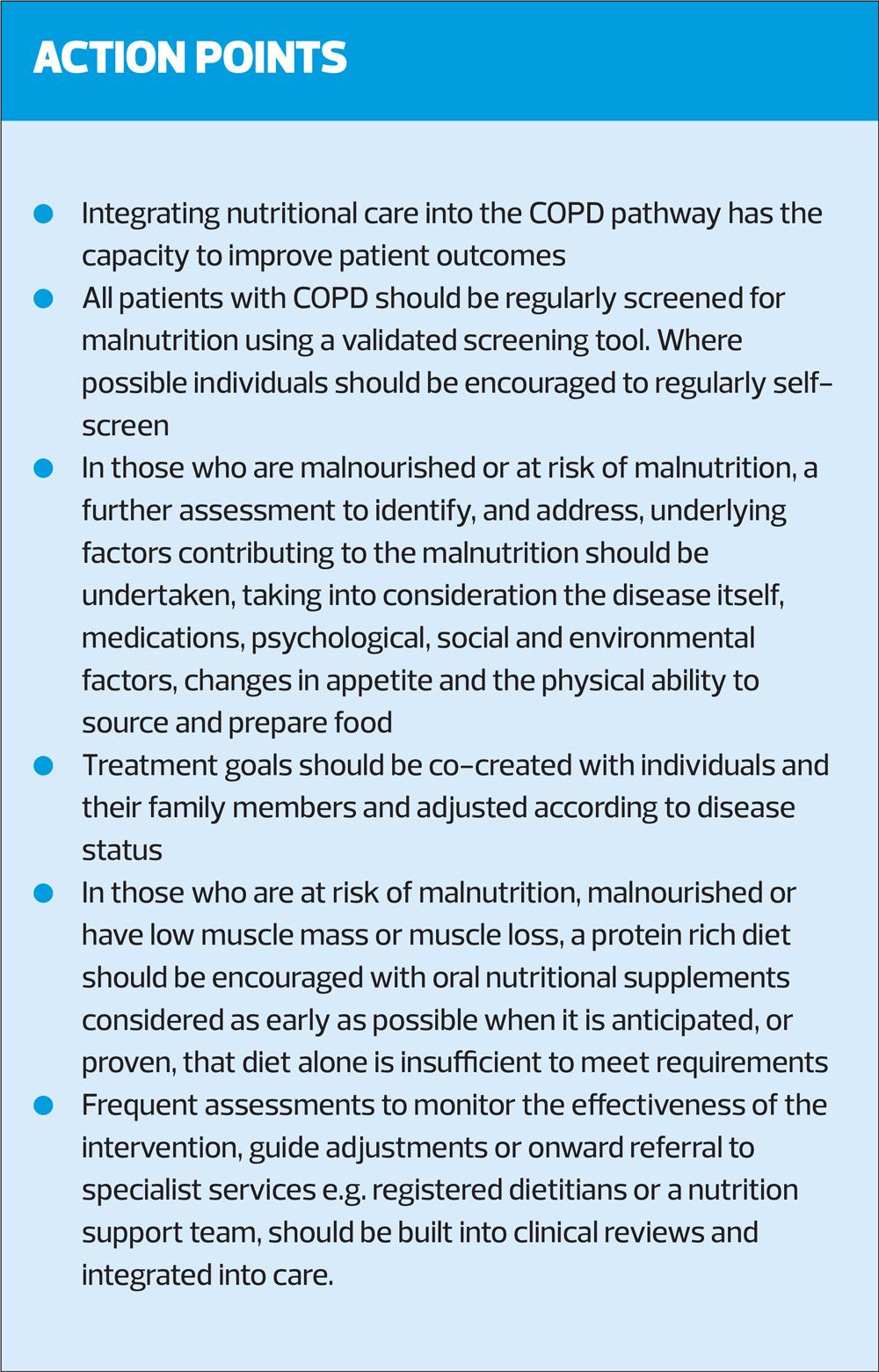
MANAGING MALNUTRITION IN PATIENTS WITH COPD
The Malnutrition Pathway team has recently updated its Managing Malnutrition in COPD guidance. The guide aims to provide a practical resource to assist the multi-disciplinary team to deliver timely nutritional advice for patients with COPD, across the spectrum of their disease. Supported by an unrestricted educational grant from Nutricia, the content was developed independently by experts in the field of COPD, representing nursing, dietetics, pharmacy, physiotherapy, respiratory medicine and research. The resource incorporates current evidence, clinical experience and good practice and translates into practice the guidance on nutrition published by the National Institute for Health and Clinical Excellence (NICE)12 and the Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease (GOLD).8
A pilot study carried out in primary care demonstrated that by implementing the Managing Malnutrition in COPD pathway, not only did nutritional care improve but significant cost savings were achieved through reductions in healthcare use.11
Helping practice nurses to deliver nutritional care
The main Managing Malnutrition in COPD guidance document provides nurses with a succinct summary on the role nutrition plays as part of a holistic approach to care. It incorporates a four-step approach, outlining how to screen for malnutrition and undertake further assessment in those at risk of malnutrition (including exploring issues that may be causing eating and drinking difficulties) to subsequently tailor treatment and advice and monitor the individual.
The four steps are outlined below:
Step 1 – Screening
NICE guidelines recommend that body mass index (BMI) is calculated in all patients with COPD.12 As a high BMI is now common in a large percentage of the UK population,13 and this can mask malnutrition and loss of muscle mass, it is important that nurses are alert to any unintentional weight loss, particularly in older people with COPD. Patients with COPD should therefore undergo regular nutrition screening, using a validated tool that measures both BMI and unplanned weight loss, such as the BAPEN Malnutrition Universal Screening Tool ‘MUST’ (https://www.bapen.org.uk/pdfs/must/must_full.pdf).
The Malnutrition Self-Screening website (www.malnutritionselfscreening.org) is useful for patients (and their carers) who are digitally literate – one off and sequential results are helpful in informing the GP practice or healthcare team of changes or deterioration in nutritional status and to prompt clinicians to take action.
Step 2 - Assessment
A new section on assessment has been incorporated into the updated guidance, which aims to assist nurses in identifying the underlying causes of malnutrition so that they can give specific individual dietary advice to both treat malnutrition and prevent it recurring.
It includes the acronym LEARN,14 to prompt observations and guide care:
Look at the individual – what do you see? Have they got muscle wasting, are they thin or frail looking?
Eating – ask about what they are eating, are they consuming foods from all food groups, missing meals?
Appetite – ask about appetite, has it changed?
Relatives – family members can be a source of information and support; do they have any concerns?
Nutrition – give appropriate nutritional advice. If you are not skilled or confident to do so, seek advice from someone qualified e.g. your local dietitian.
Step 3 – Management of malnutrition
The management of malnutrition section advises on patient-centred treatment goals. This section includes practical guidance and information on:
- Optimising nutritional intake and helping nurses identify common issues affecting dietary intake, signposting to further resources to facilitate the provision of timely first-line dietary advice and oral nutrition support if needed.
- The role of high-quality protein (combined with activity) to promote muscle synthesis and preservation or improvement in muscle mass and function.
- Considerations when deciding the appropriate interventions, including impact and extent of symptoms and associated COPD treatments e.g. Inhalers, medications, escalation and de-escalation of nutritional care
- The value of integrating nutritional care into pulmonary rehabilitation.
Step 4 – Monitoring the intervention
The final section advises on monitoring individual progress including ideas on what to monitor in relation to agreed goals, frequency of monitoring and when and how to discontinue oral nutritional supplements (ONS) if they have been prescribed.
INFORMATION FOR PATIENTS AND CARERS
Three complementary patient and carer leaflets accompany the document and are designed to help nurses and other members of the healthcare team select the appropriate dietary advice for patients with COPD according to their nutritional status and malnutrition risk:
- ‘Eating Well for Your Lungs’ (green leaflet) is designed for individuals who are at low risk of malnutrition (‘MUST’ score of 0) and able to eat and drink. It includes advice on healthy eating as well as dealing with some of the common symptoms of COPD, such as breathlessness, dry mouth and taste changes, which can adversely affect the enjoyment associated with eating.
- ‘Improving Your Nutrition in COPD’ (yellow leaflet) provides advice for individuals at medium risk (‘MUST’ score of 1) who are experiencing a poor or reduced appetite, unplanned weight loss or are feeling weak and lacking energy. It includes advice on making the most of food (often referred to as ‘Food First’ by dietitians) to prevent further weight loss.
- ‘Nutrition Support in COPD’ (red leaflet) is aimed at individuals who are at high risk of malnutrition (‘MUST’ score of 2 or more) and who may have been prescribed ONS because they are unable to consume sufficient diet to manage or prevent malnutrition. This leaflet includes tips on making the most of food alongside the incorporation of ONS into the diet if recommended or prescribed.
Each of the three leaflets has been updated in line with research undertaken with individuals affected by COPD, including their request to incorporate visuals. In addition, each of the leaflets now includes key messages to reinforce the general principles on caring for yourself with COPD (e.g. smoking cessation, keeping active). The leaflets are available in English and Welsh, and can be downloaded free at https://www.malnutritionpathway.co.uk/copd.
ADDITIONAL RESOURCES
In addition to the Managing Malnutrition in COPD materials, the Malnutrition Pathway website includes a range of resources to support a variety of healthcare professionals in managing malnutrition in other conditions in the community. There is also web content dedicated to support the specific needs of general practice nurses (https://www.malnutritionpathway.co.uk/pcn/practice_nurse.html) which includes advice on subjective indicators of weight loss, malnutrition screening, initiating conversations about weight loss and identifying causes and symptoms that may be interfering with dietary intake and enjoyment of eating.
SUMMARY
Poor nutritional intake in individuals with COPD is common. Causes of poor intake and malnutrition in individuals with COPD are varied and include the physiological effects of the disease, psychological, social and environmental factors. To optimise metabolic health, prevent malnutrition and improve outcomes, dietary advice should be an integral part of COPD management across the continuum of care. Practice nurses can play a key role in ensuring that patients are nutritionally screened and assessed to identify nutritional issues. If confident and competent to do so, nurses can offer first-line dietary advice and oral nutrition support using evidence-based resources available and refer those at high risk of malnutrition, or those with more complex nutritional needs, to the appropriate professional, i.e. dietitian, for further intervention. Timely nutritional interventions can have positive effects on overall patient care and bring benefits to the individual’s quality of life.
REFERENCES
1. NICE QS10. Quality standards and indicators. Briefing paper. Chronic obstructive pulmonary disease (COPD) update; 2015. https://www.nice.org.uk/guidance/qs10/documents/briefing-paper
2. Deng M, Lu Y, Zhang Q, et al. Global prevalence of malnutrition in patients with chronic obstructive pulmonary disease: Systemic review and meta-analysis. Clinical Nutrition 2023; 42 (6): 848-58
3. Putcha N, Anzueto AR, Calverley PMA, et al. Mortality and Exacerbation Risk by Body Mass Index in Patients with COPD in TIOSPIR and UPLIFT. Ann Am Thorac Soc 2022; 19(2): 204-13
4. Collins P, Yang IA, Chang Y-C, Vaughan A. Nutritional support in chronic obstructive pulmonary disease (COPD): an evidence update. J Thorac Dis 2019;11(Suppl 17):S2230-2237
5. Saunders J, Smith T. Malnutrition: causes and consequences. Clin Med (Lond) 2010;10(6):624-7.
6. Steer J, Norman E, Gibson GJ, et al. P117 Comparison of indices of nutritional status in prediction of in-hospital mortality and early readmission of patients with acute exacerbations of COPD. Thorax 2010;65(4):A127-A127
7. Hoong JM, Ferguson M, Hukins C, Collins PF.. Economic and operational burden associated with malnutrition in chronic obstructive pulmonary disease. Clin Nutr 2017;36(4):1105–1109
8. Global Initiative for Chronic Obstructive Lung Disease (GOLD). 2024 GOLD REPORT; 2023. https://goldcopd.org/2024-gold-report/
9. Ferreira IM, Brooks D, White J, Goldstein R. Nutritional supplementation for stable chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2012;12. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000998.pub3/full
10. Collins PF, Stratton R, Elia M. Nutritional support in chronic obstructive pulmonary disease: a systematic review and meta-analysis. Am J Clin Nutr. 2012 Jun;95(6):1385-95
11. Cawood A, Kominek N, Janik L, et al. Local implementation of a pathway to manage malnourished COPD patients in the community. Eur Respir J. 2017;50 (suppl 61):PA1609
12. NICE NG115. Chronic obstructive pulmonary disease in over 16s: diagnosis and management; 2018. https://www.nice.org.uk/guidance/ng115
13. NHS Digital. Statistics on Obesity, Physical Activity and Diet, England, 2020. https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-obesity-physical-activity-and-diet/england-2020 Accessed 12/02/24
14. Anderson L. Why unexpected weight loss in older people should not be ignored. Nursing Older People; Dec 2019. https://rcni.com/nursing-older-people/opinion/comment/why-unexpected-weight-loss-older-people-should-not-be-ignored-155766
Related articles
View all Articles