Practice Nurse bite-sized learning: Understanding chronic kidney disease
Michaela Nuttall
Michaela Nuttall
RGN MSc
Founder & Director, Learn With Nurses
Joanne Haws
RN MSc
Clinical Director, Learn With Nurses
Practice Nurse 2024;54(4):10-11
INTRODUCTION
Chronic kidney disease (CKD) is a long-term condition where the kidneys do not work effectively due to abnormalities of the structure or function that are present for a minimum of three months.1 The kidneys have five main functions:
- Balance levels of salt and water
- Excrete waste from the blood
- Control blood pressure
- Make strong bones
- Boost production of red blood cells
WHAT'S THE PROBLEM
Around 7.2 million people in England have diagnosed CKD, and there are thought to be around a million people who have the condition but who are undiagnosed.2 CKD can substantially reduce quality of life and leads to premature death for thousands of people each year, even at early stages. It is also a major driver of health inequalities, with a disproportionate burden on ethnic minority groups, such as those from South Asian backgrounds with diabetes, who are ten times more likely to develop end stage kidney failure than Caucasian people with diabetes.
DETECTION
CKD does not usually cause symptoms until it reaches an advanced stage so proactive case finding is essential and should be targeted at the following population groups:
Adults with:
- Diabetes
- Hypertension
- Heart disease and/or heart failure.
- Family history of CKD or kidney failure
- Personal history of acute kidney injury (AKI)
- Structural renal tract disease, renal calculi or prostatic hypertrophy
- Multisystem diseases such as Systemic Lupus Erythematosus (SLE) or HIV
- Gout
DIAGNOSIS
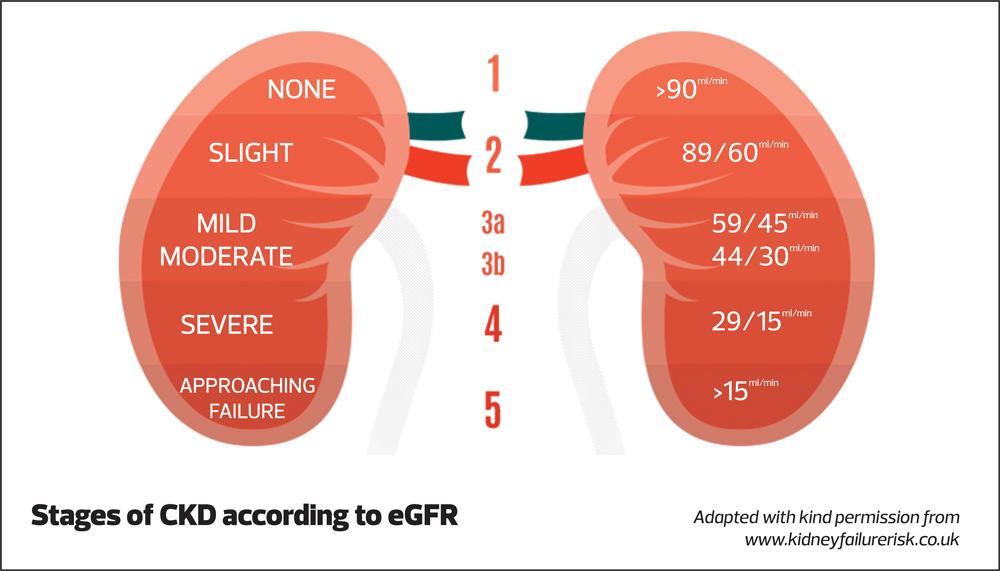
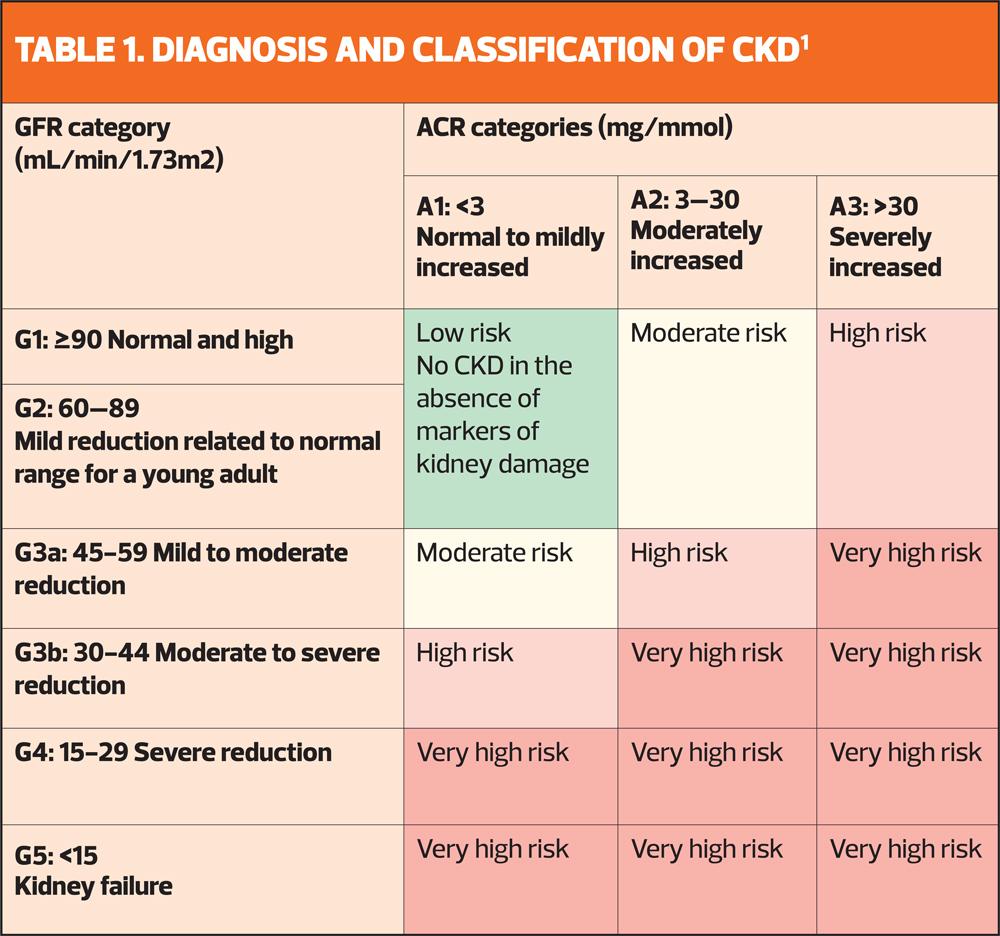
Testing for CKD should include measurement of estimated Glomerular Filtration Rate (eGFR) and urinary albumin creatinine ratio (uACR). Those with abnormal results should be retested in 3 months’ time before the diagnosis can be confirmed and classification can take place (Table 1).4 A lack of uACR measurement i.e. measurement of eGFR only, may lead to underdiagnosis, underestimation of severity and underestimation of risk in the individual.
GFR category (ml/min/1.73m2) | ACR category (mg/mmol) | ACR category (mg/mmol) | ACR category (mg/mmol) |
A1: <3 Normal to mildly increased | A2: 2-30 Moderately increased | A3: >30 Severely increased | |
G1: >90 Normal and high | Low risk No CKD in the absence of markers of kidney damage | Moderate risk | High risk |
G2: 60-89 | Low risk No CKD in the absence of markers of kidney damage | Moderate risk | High risk |
G3a: 45-59 Mild reduction related to normal range for a young adult | Moderate risk | High risk | Very high risk |
G3b: 30-44 Moderate to severe reduction | High risk | Very high risk | Very high risk |
G4: 15-29 Severe reduction | High risk | Very high risk | Very high risk |
G5: <15 Kidney failure | Very high risk | Very high risk | Very high risk |
MANAGEMENT
Management of CKD should include:1,4
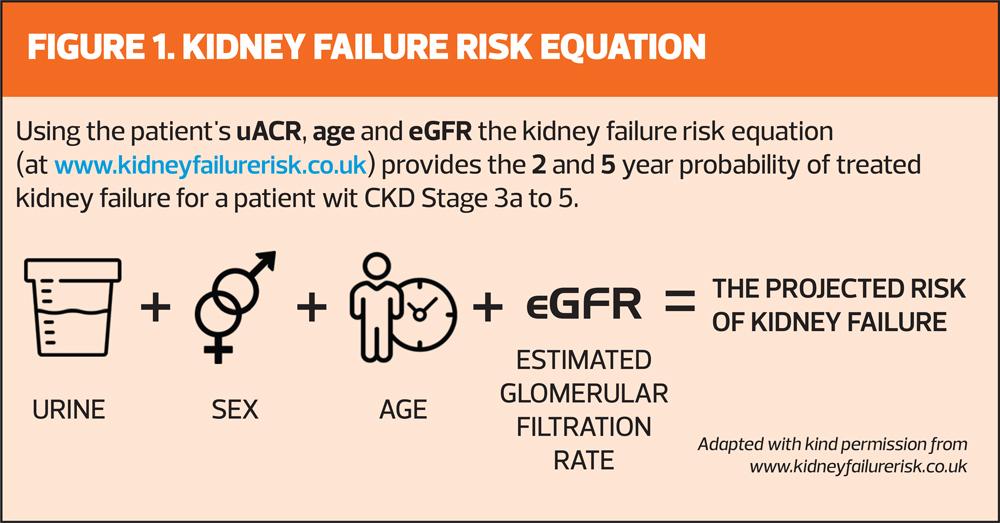
1. Evaluation of risk
- QRISK3 (if available or QRISK2) for CVD risk, be aware of underestimation of risk as uACR not included
- Kidney Failure Risk Equation (Figure 1)
2. Medicines optimisation
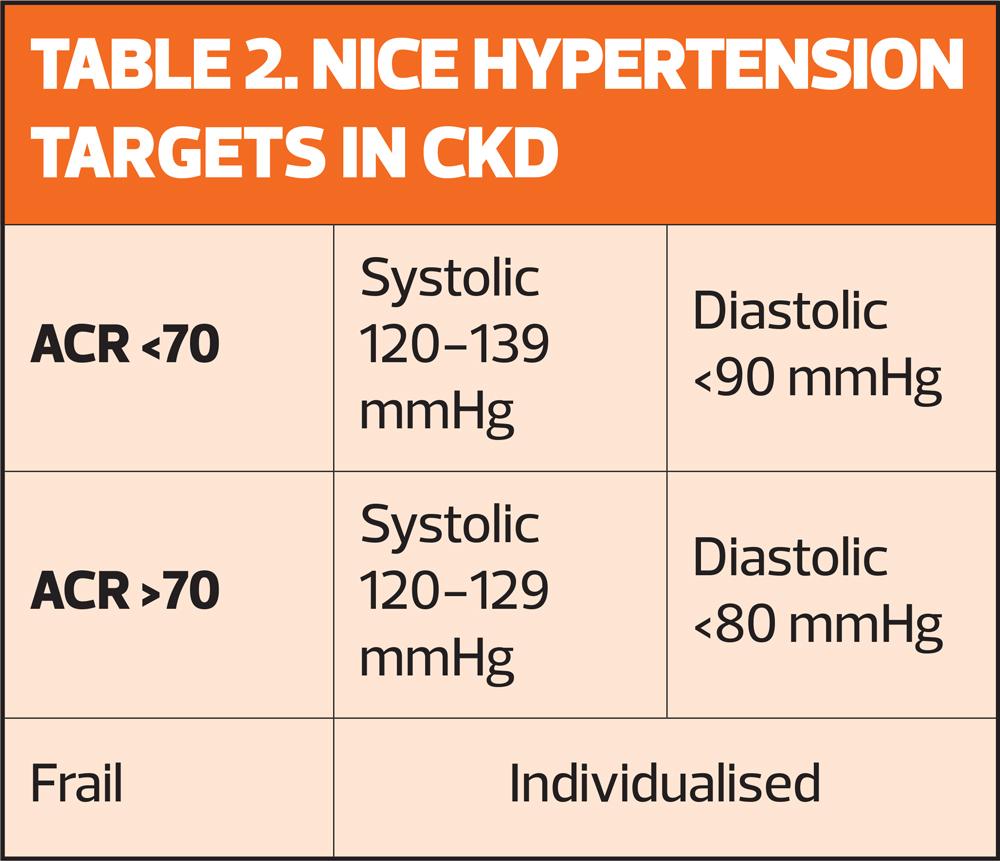
- Blood pressure control (Table 2)
- Maximum tolerated inhibition of Renin Angiotensin Aldosterone (RAAS) system with ACE inhibitor or Angiotensin Receptor Blocker
- Lipid lowering therapy
- Sodium-glucose transport protein 2 inhibitor (SGLT2i): dapagliflozin or empagliflozin
- Mineralocorticoid receptor antagonist (MRA): fineronone
ACR <70 | Systolic 120-139 mmHg | Diastolic <90 mmHg |
ACR >70 | Systolic 120-129 mmHg | Diastolic <80 mmHg |
3. Optimisation of long-term conditions
4. Patient education
- Lifestyle including smoking, diet, physical activity, salt and alcohol intake
- Vaccinations including Flu, pneumonia and COVID
- ‘Over the counter’ medications including NSAIDs such as ibuprofen that are nephrotoxic
- Sick day rules – prevention of AKI with dehydrating illnesses e.g. diarrhoea
5. Early identification of frailty
REVIEW
Patients with CKD should be added to the register for a minimum of annual recall for review.3 eGR and uACR should be checked at least annually and up to 4 times per year for those at highest risk.1 As well as routine monitoring of blood pressure and pulse, auscultation of the heart sounds should also be carried out by an appropriately skilled clinician. Heart valve disease is common in people with CKD and regular monitoring is essential.1
REFERENCES
1. KDIGO 2024 Clinical Practice Guidelines for the Evaluation and Management of Chronic Kidney Disease. https://kdigo.org/wp-content/uploads/2024/03/KDIGO-2024-CKD-Guideline.pdf
2. Kidney Care UK. Facts about kidneys; 2024. https://kidneycareuk.org/kidney-disease-information/about-kidney-health/facts-about-kidneys/
3. Kerr M. Chronic Kidney Disease in England: the human and financial cost; 2012
4. NICE NG203. Chronic kidney disease: assessment and management; 2021. https://www.nice.org.uk/guidance/ng203
Related articles
View all Articles