Understanding Electrocardiography
Margaret Perry RGN BSc(Hons) MSC
Margaret Perry RGN BSc(Hons) MSC
Advanced Nurse Practitioner, Linkway Medical Practice, West Bromwich
Knowing how to perform an ECG and to interpret, at least at a basic level, is an essential part of practice nursing
The electrocardiogram (ECG) is a commonly used test and is widely regarded as an indispensible and important tool for the detection and diagnosis of heart disease. An increasing number of general practices now offer the ECG in their surgery, and for many practice nurses, performing an ECG has become an expected part of their daily workload. This article aims to give an overview of the test, helping nurses to understand the procedure and its use in the primary care setting, to provide you with more knowledge and greater confidence when asked to perform this procedure.
WHAT THE ECG RECORDS
An ECG is simply a representation of the electrical activity of the heart muscle as it changes with time, usually printed on paper for easier analysis.1 In common with other muscles cardiac muscle contracts in response to electrical changes known as depolarisation2 which are then detected by the electrodes attached to the body. The amplification and recording of this electrical activity is therefore what we see on paper and is what is known as an ECG.
THE CARDIAC CYCLE
The heart and cardiovascular system are fundamental to the functioning of almost every other organ system.3
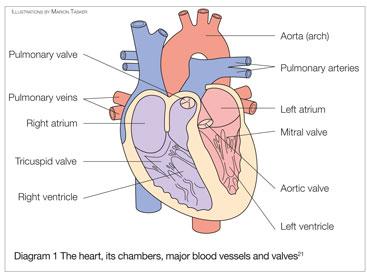
Diagram 1 show the chambers, major blood vessels and heart valves
A single cycle of cardiac activity can be divided into two basic phases, diastole and systole.4 The diastolic phase represents the time at when the ventricles are relaxed. Venous blood enters the right atrium form the superior vena cava and the inferior vena cava, whilst the left atrium receives its blood supply from the pulmonary veins which carry oxygenated blood from the lungs. The systolic phase occurs when both left and right ventricles force open the aortic and pulmonary valves to allow blood to enter the aorta and pulmonary artery. During this phase no blood can enter the ventricles as the atrioventricular valves remain firmly closed, however blood continues to flow from the vena cavae and the pulmonary veins in both the left and right atria, ready for the cycle to repeat. The whole process works in close correlation with electrical impulses, which pass through the heart and are responsible for ensuring the heart contracts as a complete unit.
THE ROLE OF ELECTRICAL IMPULSES
The sino atrial node (SA node) sends impulses to the myocardium at the rate of seventy to eighty per minute and these are responsible for the rhythmical contraction of the heart muscle, whilst the atrio-ventricular node (AV node) provides a pathway between the atria and the ventricles. When the ventricles are in diastole (relaxed), the SA node sends an electrical impulse to the atria, which causes the atria to contract and the ventricles to fill with more blood. The electrical signal that causes contraction, moves from the atria toward the ventricles, reaching the atrioventricular node (AV node) which then delays the signal so that the ventricles can contract all at once rather than a little bit at a time.5
THE 12 LEAD ECG
The ECG can be used as a tool to aid diagnosis of heart conditions but may also be carried out during surgery to monitor cardiac function and also to observe heart function in patients who are on a ventilator. Box 1 shows some of the cardiac conditions that may be found.
The ECG can however also detect ECG abnormalities, which can be present in a wide variety of non-cardiac conditions, complicating the differential diagnosis. Table 1 shows some of the non-cardiac problems which may be detected.
Performing the ECG
- Make sure the patient understands why the procedure has been requested and that they are happy to proceed
- The patient will need to undress to the waist and also remove tights or socks exposing bare ankles
- For males with hairy chests it may be necessary to shave the chest to ensure pads will adhere and also to avoid discomfort when they are removed
- The patient needs to be calm and still throughout the procedure. Unfortunately nervous patients who are so nervous they have a tremor, can produce an ECG which mimics arrhythmias such as atrial fibrillation and atrial flutter, and if severe enough ventricular tachycardia or ventricular fibrillation6
- The 12 leads are attached to the body as shown in diagram 2
- It is important to make sure the leads are correctly placed. Misplacement of the electrodes can lead to detection of potentially serious arrhythmias and misdirected treatment decisions.6
Diagram 2 shows that four leads are attached to the limbs, two to the right and left arms, (which can be placed on the shoulders or at the wrist), and a further two to the right and left leg (usually at the outer aspect of the ankle). The lead connected to the right ankle is a neutral lead, like those found inside an electric plug. It is there to complete an electrical circuit and plays no role in the ECG itself.7
Limb leads
- The lead on the left wrist or shoulder is the AVL lead and this looks at the upper left side of the heart
- The AVR lead is on the right shoulder or wrist and looks towards the cavity of the heart
- The left leg lead or AVF looks at the inferior surface of the left ventricle
WHAT THE 12 LEADS DETECT
The PQRS complex
The graphical representation of cardiac activity is shown as the P wave, QRS complex and the T wave. A normal PQRS complex is shown at figure 1.
What each phase measures is explained as follows:
P wave: This represents atrial contractions
QRS: This represents ventricular contractions
T wave: this represents electrical activity when the ventricles are recharging in preparation for the next contraction also known as repolarisation.
The normal ECG
Figure 2 shows a normal ECG where the rate and rhythm is normal and a P wave is clearly visible before each of the QRS complexes. Each PR interval is less than five of the small squares which indicates that the electrical signal is travelling in a normal fashion through the heart.8
COMMON ABNORMALITIES
Obviously it is outside the scope of this article to go into depth as there are a vast number of cardiac problems, therefore only some of the commonest problems will be discussed.
Atrial fibrillation
Atrial fibrillation is the most common heart rhythm disturbance encountered by doctors affecting in excess of one million people in the UK.9 The condition may be episodic (also called paroxysmal) or chronic. It is caused when chaotic electrical activity develops in the atria leading to irregular and rapid ventricular beats detected on the ECG when the rhythm strip shows the pattern shown in Figure 3. Acute episodes may be caused by infection, high alcohol intake or cardiac events such as myocardial infarction, and there is an increased risk among the elderly, those with diabetes, hypertension, smokers and patients with valvular disease.10
Sinus bradycardia
Sinus bradycardia (Figure 4) occurs when fewer than the normal number of impulses arise from the sinoatrial (SA) node resulting in a heart rate below 60 beats per minute.11 The true incidence of bradycardia is unknown but sinus node dysfunction occurs in 1 in 600 patients per year over the age of 65 years.12 The condition can be an incidental finding in otherwise healthy individuals particularly young adults.13 However, other causes have been named as electrolyte disorders, infection, hypoglycaemia, hypothyroidism and sleep apnoea.13
Supraventricular tachycardia
Supraventricular tachycardia (Figure 5) occurs when the heart beats at an abnormally fast rate but episodically. These episodes of rapid beating can last for seconds, minutes or hours (although this is rare) resulting in dizzy spells and shortness of breath.15 Supraventricular tachycardia is common in young children and anxious young people but can also occur in heavy drinkers smokers and those who drink large amounts of caffeine.16
Bundle branch block
Bundle branch block (Figure 6) can affect either the right or left side of the heart. The condition arises when there is a delay or obstruction along the pathway as the electrical impulses travel through the heart.17 Heart block can be caused by cardiomyopathy, valvular disease or coronary artery disease, however right heart block can occur in an otherwise healthy heart.18 A study which followed a cohort of men aged 50 for 30 years found that the incidence of bundle branch block increased for 1% at age 50 to 17% at age 80.19
Limitations of the ECG
Patients who are under investigation for an irregular heart rate which appears intermittently may have a normal ECG if the problem is not present at the time of the recording. In common with other tests, false positive and false negatives are always possible
Conclusion
ECG is becoming more widely available in general practice and, as has been discussed, is a very useful diagnostic tool. With a better understanding of the procedure nurses can confidently approach the task with the ability to support and advise patients in the light of better knowledge and more confidence. o
REFERENCES
1. Price D. How to read an Electrocardiogram (ECG). Part One: Basic principles of the ECG. The normal ECG. South Sudan Medical Journal.2010 http://www.southsudanmedicaljournal.com/archive/may-2010/how-to-read-an-electrocardiogram-ecg.-part-one-basic-principles-of-the-ecg.-the-normal-ecg.html 2. Hampton JR. The ECG Made Easy Fifth Edition. London: Churchill Livingstone:1998
3. Epstein O, Perkin GD, de Bono DP, Cookson J. Clinical Examination 2nd Edition. London: Mosby: 1997
4. Klabunde RE. The cardiac cycle. Cardiovascular Physiology Concepts. 2011. http://www.cvphysiology.com/Heart%20Disease/HD002.htm 5. Laberge M. Cardiac cycle. Encyclopaedia of Nursing & Allied Health, 2002 http://www.enotes.com/cardiac-cycle-reference/cardiac-cycle 6. Baranchuk A, Shaw C, Alanzi H, et al Electrocardiography pitfalls and artefacts: The 10 Commandments. Critical Care Nurse 2009;29: 67-73
7. University of Nottingham. Cardiology Teaching package, 2012 http://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/chest_leads.php 8. Ambulance Technicians study ECG rhythms, 2006. http://www.ambulancetechnicianstudy.co.uk/rhythms.html 9. Atrial Fibrillation Association What is atrial fibrillation? Atrial Fibrillation Association 2012. http://www.atrialfibrillation.org.uk/patient-information/atrial-fibrillation.html 10. Benjamin EJ, Levy D, Vaziri SM, et al. Independent Risk Factors for Atrial Fibrillation in a Population-Based Cohort: The Framingham Heart Study JAMA 1994; 271:840-4
11. Ganz LI. Sinus Bradycardia Uptodate.com, 2011 http://www.uptodate.com/contents/sinus-bradycardia 12. Bernstein AD, Parsonnet VM. Survey of cardiac pacing in the United States in 1989. Am J Cardiol 1992;69:331-8.
13. Livingston M. Sinus bradycardia Medscape Online, 2010 http://emedicine.medscape.com/article/760220-overview 14. Cardionetics. Rhythms and Arrhythmia: Sinus Bradycardia. 2012. http://www.cardionetics.com/cardiology/sinus-bradycardia.php 15. NHS Choices. Supraventricular tachycardia. http://www.nhs.uk/conditions/Supraventricular-tachycardia/Pages/Introduction.aspx 16. American Heart Association Tachycardia, 2011
http://www.heart.org/HEARTORG/Conditions/Arrhythmia/AboutArrhythmia/Tachycardia_UCM_302018_Article.jsp 17. Mayo Clinic Bundle Branch block Mayo Foundation for Medical Education and Research, 2010 http://www.mayoclinic.com/health/bundle-branch-block/DS00693 18. Texas Heart Institute. Bundle branch block, 2011 http://www.texasheartinstitute.org/HIC/Topics/Cond/bbblock.cfm 19. Eriksson P, Hansson PO, Eriksson H, et al. Bundle-Branch Block in a General Male Population: The Study of Men Born 1913. Circulation.1998;98:2494-2500
20. Cardionetics. Rhythms and arrhythmia: Bundle branch block. 2012 http://www.cardionetics.com/cardiology/bundle-branch-block.php 21. American Heart Month, 2011 http://www.justfocuswell.com/607/american-heart-month-biology/ 22. Bloe C. ECG rhythms without the blues. Skills for Nurses, 2006 http://www.scottishirishhealthcare.com/index.cgi?article+147 23. Cardionetics Rhythms and arythmia: Atrial fibrillation, 2012 http://www.cardionetics.com/cardiology/atrial-fibrillation.php
Related articles
View all Articles