Understanding cardiac arrhythmias
JOANNE LOADES
JOANNE LOADES
RN MSc
Independent Nurse Consultant & Specialist in Cardiovascular Disease
Despite tremendous advances in the detection and management of cardiac arrhythmias that enable patients to be diagnosed and successfully treated more quickly, arrhythmia still carries a risk of sudden cardiac death and the experience of arrhythmia remains frightening for many patients and their families. Primary care nursing teams play an important role in the detection and long-term monitoring of these patients
The normal heart beats in a regular and coordinated way due to the generation and spread of electrical activity within the cardiac muscle cells (myocytes), which stimulates a series of organised myocardial contractions.1 A cardiac arrhythmia can be simply defined as a variation from the normal heart rate and/or rhythm that is not physiologically justified, and that may, or may not result in symptoms for the individual.2 The impact on patient outcomes may range from harmless, to a catastrophic event or even sudden cardiac death. The gateway to successful treatment of arrhythmias, where necessary, is the identification of the abnormality and timely referral to a specialist, where appropriate. Primary care nursing teams have a key role in the early identification and ongoing support of patients with arrhythmia, particularly through their monitoring of those with increased risk due to underlying cardiovascular disease.
HOW BIG IS THE PROBLEM?
Arrhythmias are experienced by more than 2 million people a year in the UK, with the most common form being atrial fibrillation, accounting for around a half of all cases.3 In the UK fatal forms account for around 100,000 deaths each year, many of which could be prevented if the arrhythmia were diagnosed and treated earlier.3
IMPACT ON THE PATIENT
The impact of arrhythmia on the patient will vary according to a variety of factors, particularly the severity of the condition and the associated symptoms. Patients may experience their heart beating too quickly, too slowly or in an irregular manner. Symptoms may include palpitations, breathlessness, dizziness and fatigue; and in the most severe cases arrhythmia can lead to loss of consciousness or, ultimately, sudden cardiac death.4 (Box 1) The symptoms can be extremely frightening for patients and their families and the fear of sudden cardiac death can result in severe anxiety and a restricted lifestyle, which can in itself be detrimental to overall cardiovascular risk.5
In addition to the symptoms and potential consequences of the arrhythmia itself, including the five-fold risk of stroke in atrial fibrillation, the burden of investigation and treatment can, unfortunately, be challenging for patients. Investigations and procedures can be time-consuming and may require travel to specialist centres, and many anti-arrhythmic drugs can have unpleasant side-effects.
The availability of Arrhythmia Specialist Nurses is inconsistent across the country and many patients will not be able to access the support that they can offer.4 Care may be delivered in a variety of settings, according to the nature and severity of the condition, and many patients will also have co-existing long term conditions. It makes sense, therefore, for nurses in primary care to become equipped to feel confident in discussing issues relating to cardiac arrhythmias with patients, and to be able to signpost to other sources of support where required.
WHAT DOES NORMAL LOOK LIKE?
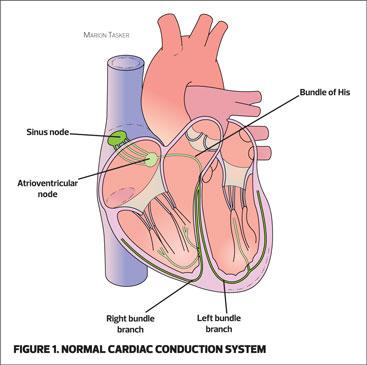
The normal heart rhythm starts in the sino-atrial (SA) node, located in the wall of the right atrium and controlled by the autonomic nervous system. The SA node is the heart’s natural pacemaker and will usually generate electrical impulses at a rate of 60-100 times per minute. These impulses spread across the atria to the atrioventricular (AV) node. The AV node is the gatekeeper that allows impulses to pass through to the ventricles via the Bundle of His, the right and left bundle branches and the Purkinje fibres.6 (Figure 1)
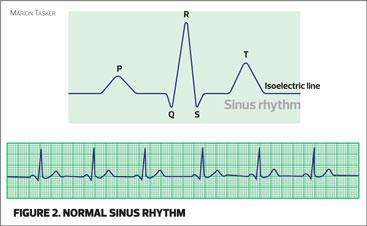
Normal sinus rhythm will have the P, Q, R, S and T wave components when seen on an ECG. (Figure 2) The most important step in being able to recognise what is abnormal is to understand what normal looks like. If primary care nurses have not previously gained this understanding and these skills, it can be very useful to be given the opportunity to develop them.
DIAGNOSING ARRHYTHMIAS
A detailed history is vital in the assessment of a patient with suspected arrhythmia, particularly the nature and frequency of any symptoms along with any precipitating or relieving factors, such as caffeine or alcohol intake, or exertion. Patients may report feelings of palpitations or fluttering in their chest, or symptoms of light-headedness, breathlessness or generally feeling unwell.
A full clinical examination of the cardiovascular system should be carried out, and investigations, including blood tests and a 12 lead ECG undertaken. Although the 12 lead ECG is a very helpful aid to diagnosis it should be remembered that this will only capture the electrical activity of the heart at the moment of recording, therefore further monitoring, such as ambulatory ECG or an event recorder, may be required.
TYPES OF ARRHYTHMIA
Arrhythmias can be divided into those that result in the heart beating too fast, known as tachyarrhythmias, and those that result in the heart beating too slowly, known as bradyarrhythmias. Some arrhythmias will allow the heart to beat at a normal rate but this will usually be in an irregular manner and may result in the presence of an irregular pulse on palpation. The arrhythmia may be short lived, paroxysmal (stops and starts), or sustained. There may only be single abnormal impulses or beats known as extrasystoles or ectopic beats. These are usually premature beats that have originated from outside of the SA node and often occur in completely healthy people. Although they can be a sign of coronary heart disease, they are often harmless and can be a result of caffeine, alcohol or nicotine intake.
Interpretation of the ECG will usually suggest where in the heart the rhythm is originating, which will help determine the treatment strategy. However, the most important observation is the effect the arrhythmia is having on the patient, and specifically whether they are haemodynamically compromised.
Tachyarrhythmias
Tachyarrhythmias occur when the heart beats more quickly than it normally should, i.e. above the upper limit of the normal range, which is greater than 100 beats per minute.
Sinus tachycardia refers to a normal heart rhythm occurring at a fast rate. While this is a normal physiological response to physical or emotional exertion, it can also be a sign of acute illness or infection.
Tachyarrhythmia may originate from within the atria or the atrioventricular (AV) junction or, more dangerously, from within the ventricles.2 Common tachyarrhythmias include atrial fibrillation and atrial flutter, though it must be stressed that neither of these arrhythmias always occur at a fast rate. A potentially life threatening tachyarrhythmia is ventricular tachycardia, which may result in syncope or sudden cardiac death. Sustained ventricular tachycardia is a common cause of cardiac arrest and ventricular fibrillation is the most common cause of sudden cardiac death.7
Bradyarrhythmias
Bradyarrhythmias occur when the heart beats more slowly than it normally should, usually less than 60 beats per minute. Sinus bradycardia is a normal heart rhythm occurring at a slow rate and is completely normal in many individuals, particularly in athletes and very fit people. It may, however, be a sign of illness such as hypothyroidism so should be reviewed in the context of the patient’s overall condition.7 A slow heart rate may also be caused by a heart block.
Heart blocks
Heart blocks occur where there is an interruption in the normal generation and conduction of impulses from the SA node. In addition to the SA node, the AV node and Purkinje system are capable of generating automatic activity, thus having the potential to act as subsidiary pacemakers where the normal function of the SA node is delayed or absent.2
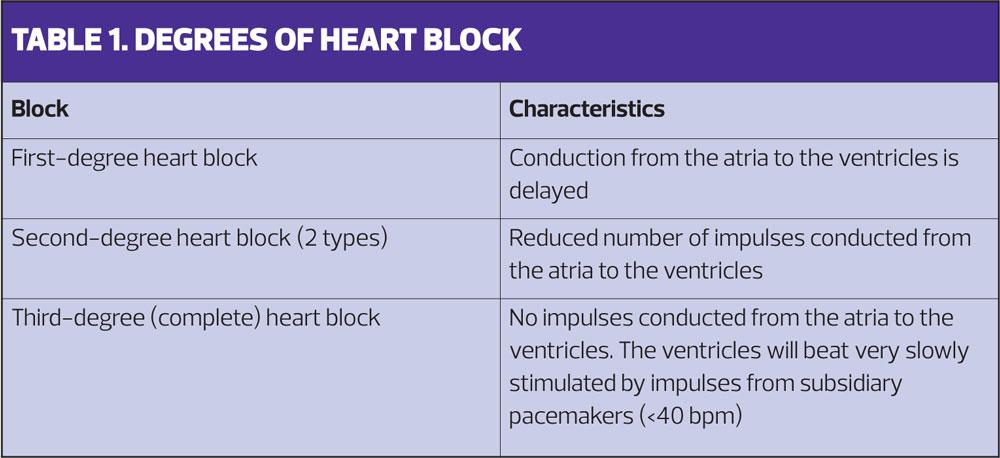
Forms of heart block are expressed as degrees of block and the symptoms and consequences, along with the need and urgency for treatment, usually increase with the severity of the block (Table 1). Symptoms may range from none at all with a first degree block, to sudden loss of consciousness requiring emergency intervention in third degree, or complete, heart block. Patients with second degree or complete heart block will usually require a pacemaker.7
Heart blocks are common in elderly patients due to chronic degenerative scarring of the conduction tissue,7 and may also occur following an acute cardiac event where circulation to the conduction system may have been compromised. Heart block following an acute cardiac event may be transient and resolve without permanent intervention.
TREATMENT OF ARRHYTHMIA
The primary aim of treating arrhythmia is to restore a normal heart rhythm. Where this is unlikely or not possible the aim will be to attain a normal ventricular rate to optimise circulation and reduce symptoms. Treatment options fall into three categories:
- Pharmacological
- Electrical
- Surgical.
The choice and urgency of treatment will usually be directed according to the severity of the patient’s symptoms and the risk of life-threatening events.
Pharmacological Treatments
Pharmacological treatments consist of anti-arrhythmic and rate-limiting agents. Class 1c anti-arrhythmic agents, such as flecainide, are commonly used. For rate control the choices include calcium channel blockers such as diltiazem, or beta-blockers such as bisoprolol.7
Unfortunately there have been no significant improvements in clinical pharmacology for arrhythmias in many years and the available agents can have pro-arrhythmic effects as well as unpleasant side effects. Issues with adherence, as well as efficacy and safety limitations of anti-arrhythmic drugs may well have supported the drive for improvements in non-pharmacological interventions.8
Electrical Treatments
Therapies that involve electrical stimulation to either terminate an abnormal rhythm, or maintain a normal heart rate, include direct current (DC) cardioversion and pacing.
DC cardioversion, using external transthoracic delivery of an electrical current, has been used since the 1950s to ‘jolt’ the heart out of an abnormal rhythm and revert it to normal.9 This procedure may be carried out in an emergency setting if the patient is experiencing, or is at risk of haemodynamic compromise, or as a planned procedure. It usually takes place under light sedation and many patients, particularly those with atrial fibrillation will need to be anticoagulated in advance to reduce the risk of any blood clots that could be dislodged during the procedure. Many hospitals have now established nurse-led cardioversion services for elective procedures.
Around 25,000 people in the UK have a permanent pacemaker fitted each year.10 The majority are implanted to stimulate an optimal heart rate in bradyarrhythmias such as heart blocks. In an emergency situation transcutaneous pacing can be achieved, using pads applied externally to the chest, as a temporary measure to stabilise the haemodynamically-compromised patient. Temporary transvenous pacing is an invasive method also used to treat patients requiring urgent intervention, either as a bridge to permanent pacing or while recovering from an acute event.11
Where there is a history, or risk, of potentially life-threatening tachyarrhythmias, such as ventricular tachycardia or fibrillation, it is usually recommended that patients receive an implantable cardioverter defibrillator (ICD), either with or without an inbuilt pacemaker to continuously monitor their heart rate and rhythm and provide pacing or an emergency shock if required.7
Surgical Treatments
Ablation therapy is a surgical procedure that uses radiotherapy or cryotherapy to destroy abnormal conduction pathways or areas of conductive tissue in the heart that facilitate arrhythmias.7 The availability of ablation therapy, and the technique, is continuously improving and many patients are benefitting as a result.
MONITORING
Patients with implanted devices will usually be monitored on a long-term basis by the implant centre, who will keep the patient’s GP updated with any changes. Patients with arrhythmia may have underlying cardiovascular disease and/or other long term conditions and be on the practice register for routine recall and review, but there may be some with primary rhythm disorders that do not fall into this group. Some will remain under the care of a cardiologist but it is worth considering how patients with arrhythmias are supported and monitored in primary care, particularly those without established disease that may fall outside of the clinical indicator requirements for the Quality and Outcomes Framework (see activities).
As with all long term conditions, regular monitoring provides the opportunity to not only perform appropriate tests and record information, but to give the patient the opportunity to access information and support to manage their own condition, which they will be doing for the majority of the time.
SUMMARY
The subject of cardiac arrhythmias can seem complex and daunting, particularly for healthcare practitioners who have not had any specialist training or experience in cardiology. As diagnosis and intervention often happens in either secondary or tertiary care, the role of primary care, particularly of general practice nurses, may be seen as unclear. However, given their role in long-term conditions management, screening, health checks and health promotion, primary care nursing teams are ideally placed to identify patients who may have a cardiac arrhythmia.
In recent years the profile of atrial fibrillation has been significantly raised in primary care, with nursing teams routinely checking pulses in ‘at risk’ groups, performing and interpreting 12 lead ECGs and undertaking stroke risk assessments. This progress has undoubtedly reduced strokes and saved lives, and can be built upon to improve the detection and management of other arrhythmias to further enable patients to access appropriate treatments, leading to longer and healthier lives.
REFERENCES
1. Mitchell B. Overview of Arrhythmias. 2017 MSD Manual Professional Version
2. Antzelvitch C, Burashnikov A. Overview of Basic Mechanisms of Cardiac Arrhythmia. Cardiac Electrophysiological Clinics 2011; 3(1):23-45
3. NHS Choices. Arrhythmia. 2018 https://www.nhs.uk/conditions/arrhythmia/
4. Ismail H, Lewin B. Evaluation of the BHF Care Co-Ordinator Awards. British Heart Foundation/University of York. 2010
5. Department of Health. National Service Framework: Coronary Heart Disease – Chapter Eight: Arrhythmias and Sudden Cardiac Death. London: NHS. 2005
6. Opie L. Heart Physiology From Cell to Circulation. 4th Edition. Philadelphia; Lippincott Williams & Wilkins: 2003.
7. Kirby M. Beating Arrhythmias. British Journal of Primary Care Nursing. 2006;3(5):239-243
8. Gheorghe-Andrei D, Martinez-Rubio A, Agewall S, et al. Anti-arrhythmic drugs – clinical use and clinical decision making: a consensus document from the European Heart Rhythm Association (EHRA) and European Society of Cardiology (ESC) Working Group on Cardiovascular Pharmacology. EP Europace 2018; 20(5):731-732
9. Cakulev I, Efimov IR, Waldo AL. Cardioversion: past, present, and future. Circulation 2009;120:1623–32
10. British Heart Foundation. Focus on: Pacemakers. Heart Matters. 2018 https://www.bhf.org.uk/informationsupport/ heart-matters-magazine/medical/pacemakers
11. Barron A, Grocott-Mason R, Dubrey S. Experience of temporary transvenous pacing in a District General Hospital. British Journal of Cardiology 2010;17:32-33
Related articles
View all Articles