Practice Nurse bite-sized learning: Understanding heart failure management
Joanne Haws
Joanne Haws
RN MSc
Clinical Director, Learn With Nurses
Michaela Nuttall
RGN MSc
Founder & Director, Learn With Nurses
Practice Nurse 2024;54(5):10-11
INTRODUCTION
There are an estimated 1 million people currently living with Heart Failure in the UK. Heart failure (HF) is a life limiting condition, with around half of patients dying within the first year of diagnosis,1 and it also has a significant impact on quality of life. Like most cardiovascular disease, significant health inequalities exist with patients from black and minority ethnic backgrounds, with women and the most socioeconomically deprived being affected at a far younger age.1
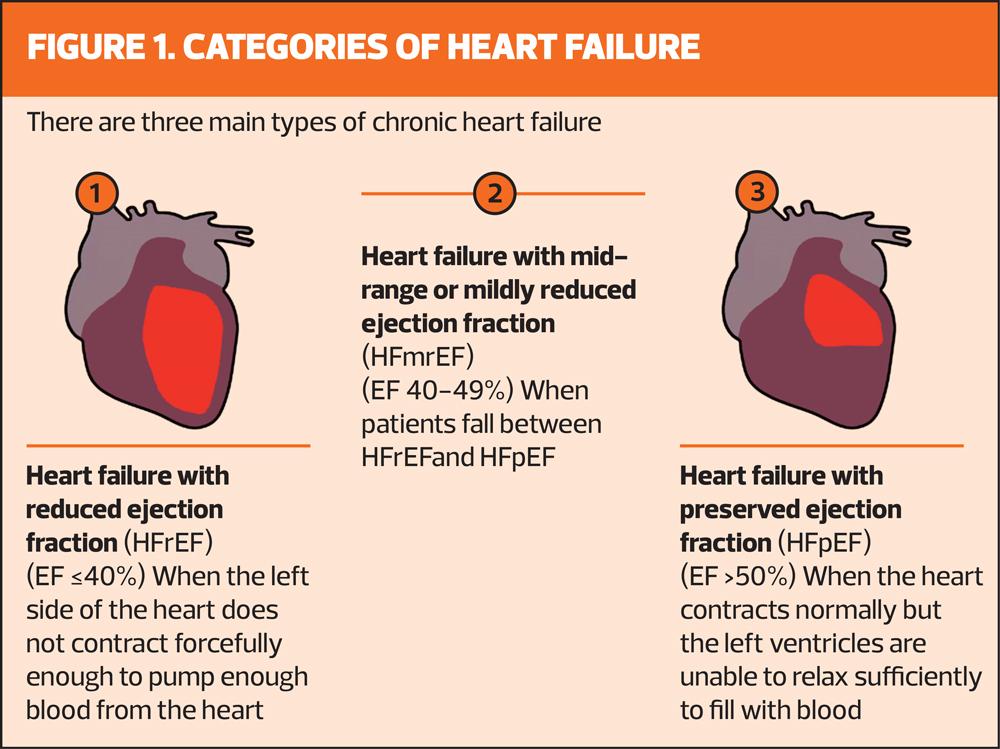
There are three types of HF that describe how the heart is affected, and each has specific diagnostic criteria (Figure 1) and management. For further information on the diagnostic pathway, see Practice Nurse 2023;53(5).
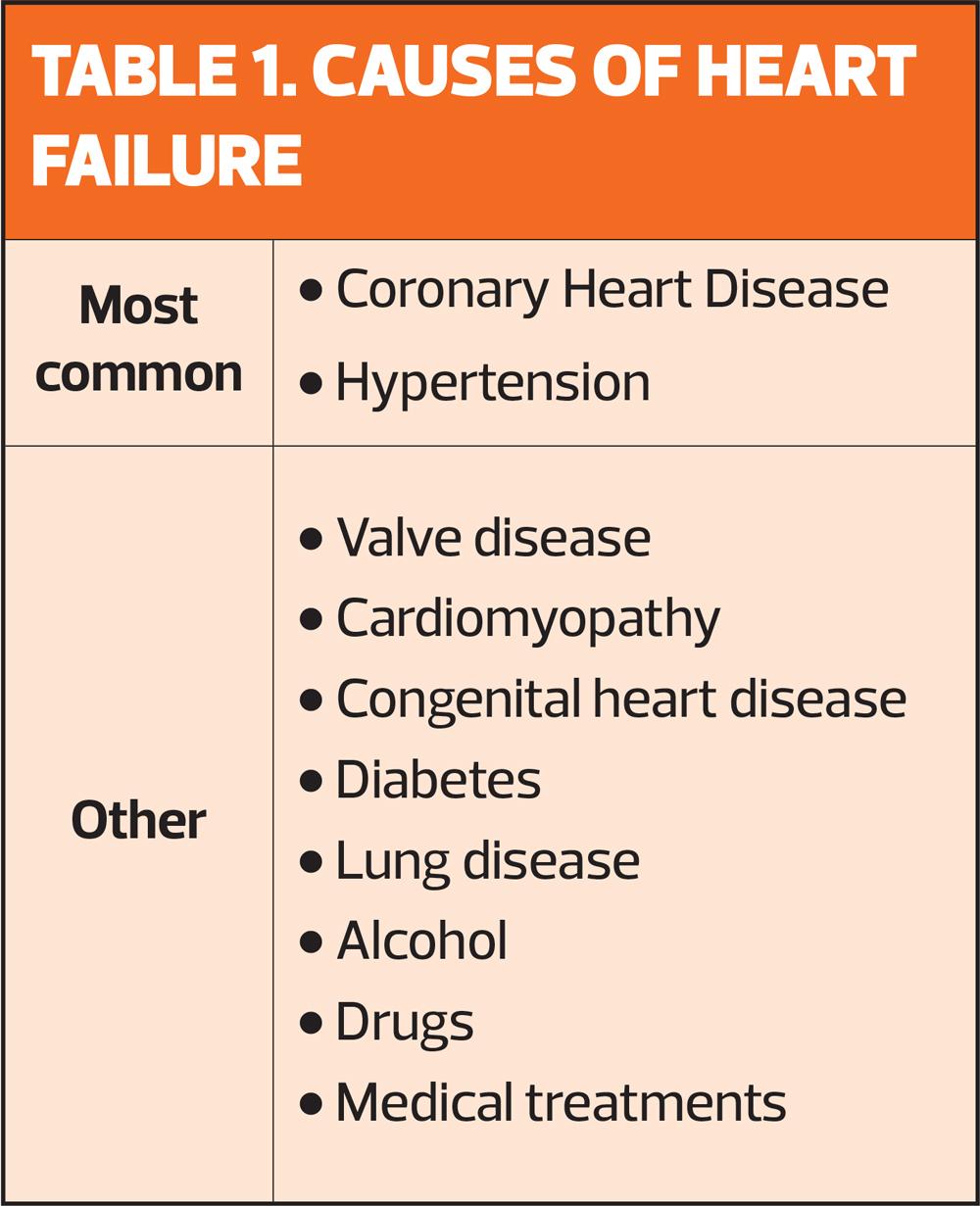
Most common |
|
Other |
|
SYMPTOM RELIEF
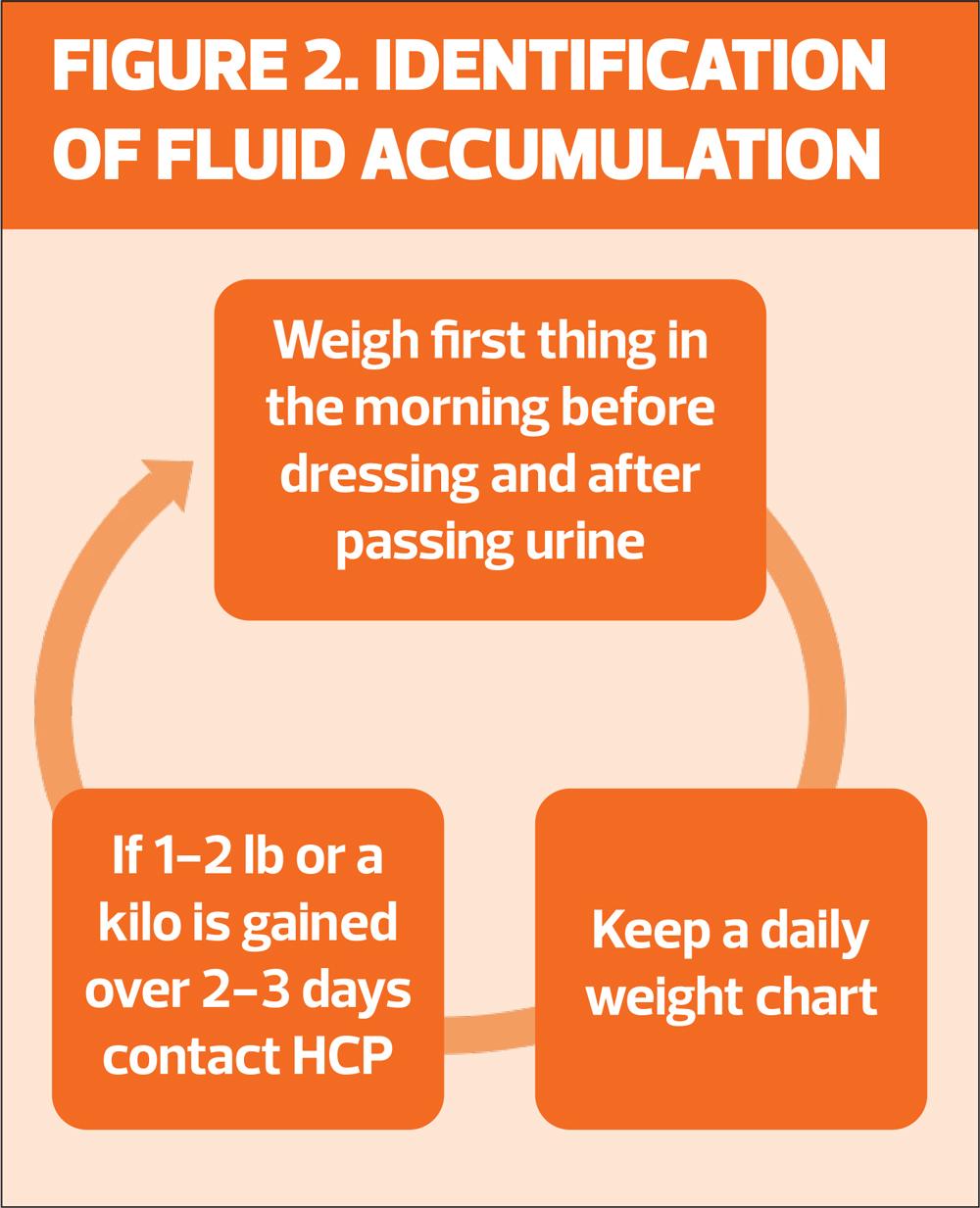
Symptoms of fluid congestion should be managed with diuretics in all types of heart failure, and these should be titrated as necessary throughout the patient’s journey.2 Renal function should be closely monitored, particularly after dose changes. Patients should be advised to monitor their weight on a daily basis for early identification of fluid accumulation (Figure 2). Minimising salt intake will help reduce fluid retention though fluid restriction is not routinely needed unless the patient is drinking excessive amounts.
THE FOUR PILLARS OF HF MANAGEMENT
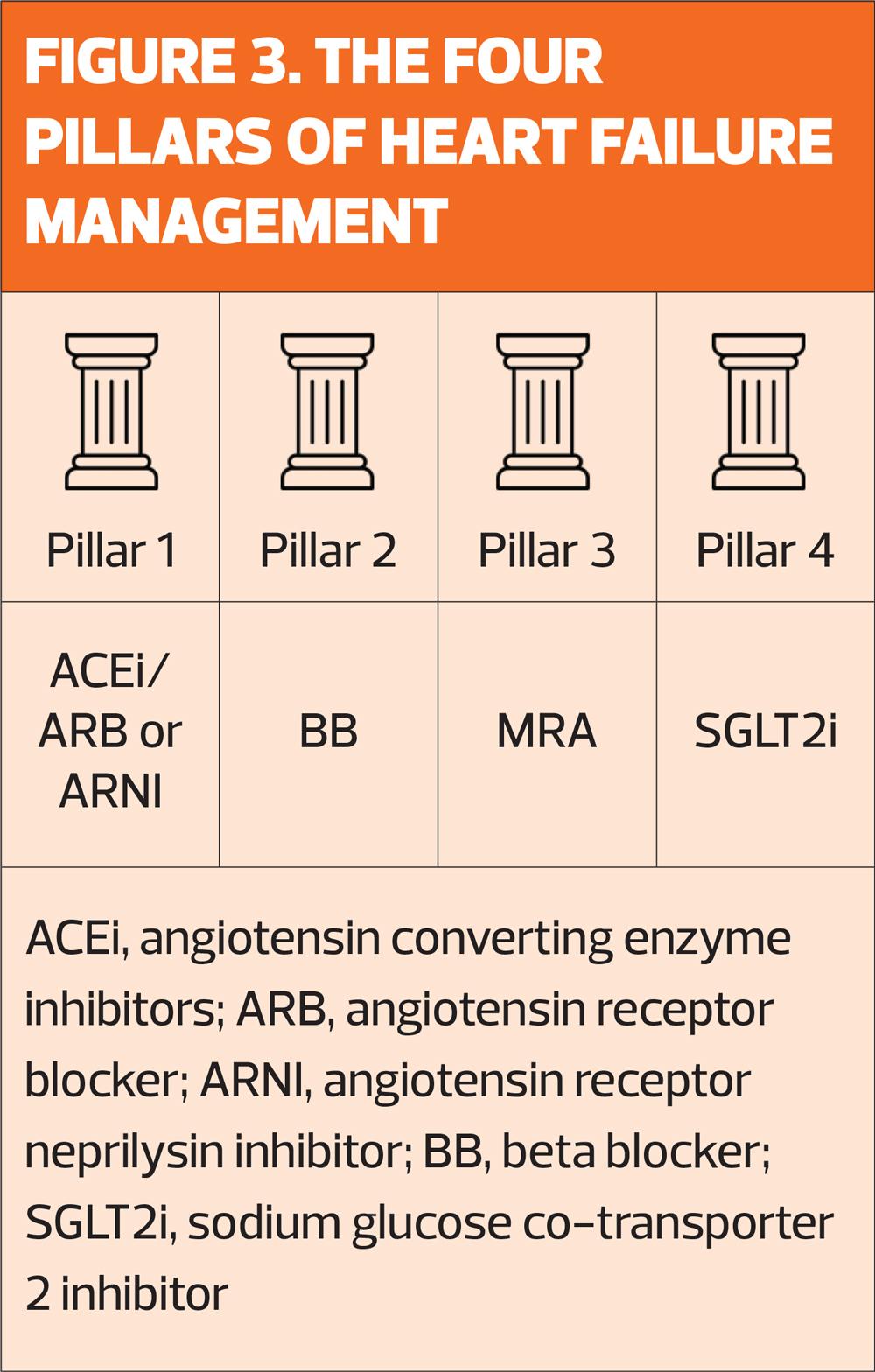
SGLT2 inhibition with dapagliflozin or empagliflozin is now recommended for all types of heart failure.3 The remainder of the ‘four pillars’ of heart failure therapies are indicated for HFrEF (Figure 3) with the focus for patients with preserved ejection fraction largely focussed on the management of comorbidities such as hypertension, diabetes and chronic kidney disease. Titration of therapies can be a complex process and, where available, may be supported by Heart Failure Specialist Nurses or other members of the specialist team.
DEVICE THERAPY
Device therapies, including implantable cardioverter defibrillators (ICD) and/or cardiac resynchronisation therapy (CRT), play an important role in the management of patients with advanced heart failure. Clinical pathways must ensure that appropriate patients are identified and referred for specialist assessment.4
LIFESTYLE MODIFICATION
Stable patients should be encouraged to be physically active and undertake a programme of personalised cardiac rehabilitation where possible.2 Patients should also be offered information and access to:
- Stop smoking support (where appropriate)
- Dietary advice
- Alcohol advice (those with alcohol-related HF should be encouraged to abstain)
- Immunisation against influenza, pneumococcal disease and COVID-19
REVIEW
Once optimised on medication, stable patients should be reviewed on at least a six-monthly basis in primary care.2
Review all of the following:
- Symptoms
- Pulse rate and rhythm, blood pressure, weight and BMI
- Renal function (including urinary albumin creatinine ratio), lipid levels and HbA1c
- Medication, including adherence
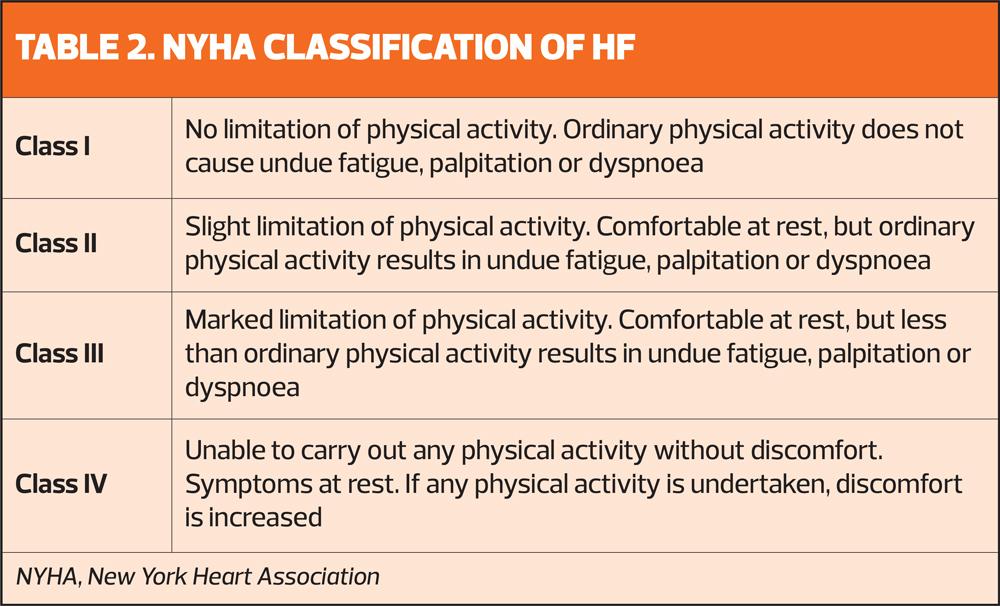
- Functional capacity using New York Heart Association Scale (Table 2)
- Lifestyle factors and self-management strategies including daily weighing and fluid balance, salt intake and physical activity
- Overall health and wellbeing, including mental health
END OF LIFE CARE
Symptoms of advanced heart failure can come and go, making it hard to know when the patient is moving towards the end of their life. People with heart failure are also at risk of dying suddenly so it is important that conversations regarding their wishes for care are had at an early stage.
REFERENCES
1. British Heart Foundation. UK Factsheet; 2024. https://www.bhf.org.uk/-/media/files/for-professionals/research/heart-statistics/bhf-cvd-statistics-uk-factsheet.pdf
2. NICE Guideline (NG106). Chronic heart failure in adults; 2018. https://www.nice.org.uk/guidance/ng106
3. NICE Clinical Knowledge Summary. Heart Failure – chronic. 2024 https://cks.nice.org.uk/topics/heart-failure-chronic/prescribing-information/sglt-2-inhibitors/
4. Ponikowski P, Voors AA, Anker SD; et al. ESC Scientific Document Group. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016 Jul 14;37(27):2129-2200
Related articles
View all Articles