How should we screen for atrial fibrillation in primary care?
Shona Holding
Shona Holding
RN BSc (Hons), MA
Cardiovascular/arrhythmia Advanced Nurse Practitioner
Affinity Care Group & Westcliffe Community Cardiology Service, Bradford
While there may be benefits in screening for atrial fibrillation to reduce stroke, there are reservations about implementing a national screening programme. We explore the controversies and discuss how screening could be carried out in general practice and what advice we can give to patients who ‘self-diagnose’ the condition
Atrial fibrillation (AF), a major cause of stroke, is more common in older people and a global, ageing population has led to its increased prevalence.1,2 This increasing prevalence has triggered much debate amongst international experts about the benefits (or not) of screening for AF.1
It is widely accepted that AF, whether symptomatic or not, is linked to increased risk of stroke, heart failure, dementia and premature death.3 Approximately 10% of ischaemic strokes occur in people with undiagnosed AF.4 Often it is not until the patient presents with a stroke that AF is confirmed.
Oral anticoagulation is an effective treatment to reduce stroke risk for selected patients in AF.5,6 Direct oral anticoagulants are now more widely available. These are as effective as warfarin, and are safer and require less monitoring, making them much easier to use. They are recommended by NICE and the European Society of Cardiology (ESC).5,6
A number of single lead-I electrocardiogram (ECG) devices are now available at relatively low cost. Their use in detection of AF in the community is increasing and will continue to evolve as new technologies and algorithms develop.1 While there is evidence from both practice and research that screening increases AF detection, and many GP practices have screening protocols in place, there is a lack of quality evidence from randomised controlled trials that AF screening reduces the incidence or severity of stroke. It remains unclear if the stroke risk in screened and unscreened populations is the same.1,7 Clinical trials, aiming to answer these queries are ongoing and recommendations from the UK screening committee are due in the near future.8
PATHOPHYSIOLOGY OF ATRIAL FIBRILLATION AND STROKE
AF is the most common dysrhythmia. It affects 2% of the general population, rising to over 5% in the over-65 age group, with further increase to 9% in over 80-year-olds.9 AF is characterised by an irregular electrical activity in the atria producing a pulse that will feel ‘irregularly irregular’.
Not all the irregularly produced impulses from the atria will pass through the atrioventricular (AV) node. The QRS complexes on the ECG will then occur in an ‘irregularly irregular’ manner, commonly described as varying RR intervals. Diagnosis of AF is confirmed when an irregular pattern, with varying RR intervals and absent P waves, is captured on ECG.3
AF is classified according to presentation and duration of episodes:
- Paroxysmal (self-terminating)
- Persistent (lasts longer than 7 days)
- Permanent (accepted by patient and physician).6
Although AF is not always life threatening, left untreated or undetected it is associated with serious complications, particularly ischaemic stroke.3 A state of hypercoagulation develops during AF, due to stasis and turbulence in the atria. This can lead to the development of clots which go on to cause thromboembolic events.3 The correlation between the timing of AF and stroke is complex and not well understood, and is currently being researched in people with pacemakers in situ.10 However, the risk for thromboembolism is regarded as the same despite temporal pattern and whether or not the individual is symptomatic.5
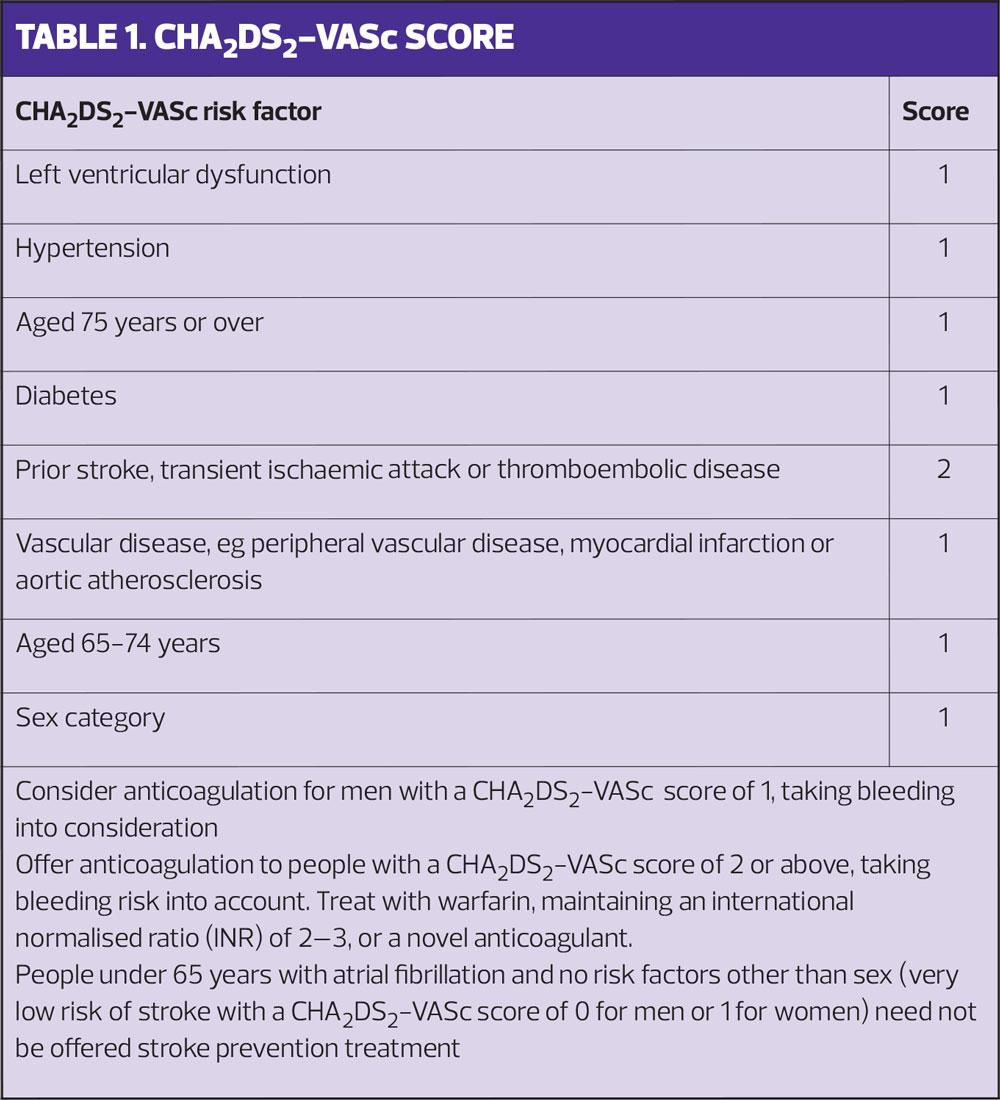
Strokes caused by AF tend to be more severe and are associated with increased mortality.1 Stroke risk is increased five-fold in those with AF and this risk increases further with age and other co morbidities, such as hypertension, diabetes, vascular disease and heart failure.2 It is well documented that the risk of stroke can be significantly reduced with anticoagulation treatment and this is recommended for those at moderate or high risk, (CHA2DS2VASc = 1 or above if male, >2 if female)(Table 1).3,5,6
According to the UK database, there has been an increase in the uptake of oral anticoagulation in those with CHA2DS2VASc=2 or above.1 However, there is still concern that approximately 30-50 % of eligible patients with AF are either inappropriately treated with aspirin, or are not receiving any form of treatment.6 Both undetected and undertreated AF is thought to contribute to a substantial proportion of all strokes, and these are potentially preventable with screening strategies.6 The Sentinel Stroke National Audit Programme (SSNAP) shows that the number people admitted with a stroke, known to have AF and who are not taking appropriate anticoagulants, has reduced from 36% in the first year of SSNAP reporting to a current figure of 15%, but there is still room for improvement.11
CURRENT GUIDANCE
Effective screening programmes depend on cost effective screening techniques with high positive predictive value.11 Targeting high risk populations will increase screening yield.11
In the SAFE study, opportunistic (pulse and ECG) or systematic (postal invitation for ECG) screening both resulted in increased AF prevalence among patients 65 years and older in both clinic and community settings.12 The study reported that 83% of those identified through opportunistic screening, and 78% of those identified through systematic screening had a CHA2DS2VASc score of 1 or above and were considered suitable for oral anticoagulation.12
The current NICE guidance recommends manual pulse checks in patients presenting with following symptoms:
- Breathlessness/dyspnoea
- Palpitations
- Syncope/dizziness
- Chest discomfort
- Stroke/TIA.5
The ESC guidelines, however, recommend opportunistic pulse-taking or ECG rhythm strip in the over-65 age group or high risk sub-groups, whether symptomatic or not.6 It also recommends 72 hour ECG monitoring after transient ischaemic attack or stroke, and longer term monitoring should be considered. The ESC guidelines suggest consideration of systematic screening in patients over 75 years or those at high risk of stroke.6 Currently, only some GP practices are screening for AF, however this is not done systematically and the practice is not widespread.8
HOW SHOULD WE SCREEN?
Screening techniques
Pulse palpation is a simple and quick assessment tool conducted during many patient consultations. Practice nurses are in prime position to perform opportunistic screening simply by performing and recording a manual pulse, both rate and rhythm. Opportunistic screening is now common practice with alerts being set up on those with additional comorbidities, such as hypertension, vascular disease, diabetes or heart failure.
Innovative technology has led to availability of various screening devices such as oscillometric blood pressure monitors that have an AF detection function based on pulse irregularity. With high sensitivity and specificity they are superior to pulse palpation and can be used by all health care workers. There is also a range of handheld single lead-I screening devices with high specificity for AF detection. They can be used at the time an irregular pulse is detected or in place of pulse palpation.11
When an irregular pulse is detected, an electrocardiogram is required to confirm AF diagnosis, either with 12 lead or single lead-I device.5
Single lead-I devices
Although a 12 Lead ECG is an essential part of the work up, it may not be available on the same day, by which time the AF may have reverted back to sinus rhythm if it is paroxysmal. Using a single lead-I device at the time an irregular pulse is detected would confirm the arrhythmia at that time. However, further evidence is needed to determine if the use of lead-I devices on those with symptoms of AF or irregular pulse impacts on increased detection of atrial fibrillation. NICE suggests data are collected to show how many of these follow up ECGs are normal and the time lapse between the single lead-I and 12 lead ECG.13
Most hand-held lead-I devices have automated algorithms which are more accurate than pulse palpation.13 They are non-invasive, re-useable, and been shown to be cost effective for AF screening and, it is argued, reduce workload.1,13
Alivecor, (Kardia) is a CE (Conformité Européenne) marked lead-I ECG device that works with a free app in conjunction with a smart phone. Two fingers are placed on the Kardia mobile to record the ECG, which is sent wirelessly to the device hosting the Kardia app. Length of recording can be set at 30 seconds and up to 5 minutes. The ECG trace can be emailed to a secure email address that complies with data protection and can then be attached to the notes.13
My Diagnostic Stick (Applied Biomedical Systems) is a CE-marked handheld lead-I ECG device that produces and interprets an ECG trace. The ECG is generated by holding metal electrodes at each end of the device for 1 minute. A red light is activated if AF is detected and a green light is activated if no AF is detected. The device is connected to a computer via USB to download the ECG for review.13
Zenicor-ECG (Zenicor Medical Systems) is a simple-to-use hand held device. ECGs are recorded by placing both thumbs on the device for 30 seconds. Data is sent to a Zenicor server where the ECG can be viewed and interpreted by authorised clinicians.13
imPulse (Plessey Semiconductors) is a CE-marked lead-I device which is provided with downloadable software, which has to be installed on a personal computer or table. ECGs are taken by holding the device in both hands and placing each thumb on a separate sensor for a pre-set period. Data are sent to the hardware hosting the software, and the recorded ECG trace is displayed in real time, analysed and AF reported as unlikely, possible or probable. The algorithm should not be used to definitively diagnose AF.13
CONTROVERSIES
Although devices are easy to use, successful screening will be enhanced with health care training.2 Data from an Australian community based study, called GP-SEARCH, provides useful information around user-confidence with iPhone devices among GPs, nurses and receptionists.14 The study recruited from three primary care practices. Nurses and receptionists used the phone device to screen patients over 65 years and GPs were responsible for interpreting the data. Unsurprisingly, nurses were more confident with the screening process than reception staff. Interestingly, the GPs tended to rely on their own interpretation rather than relying on the automated algorithm and found they picked up abnormalities other than AF.
In the UK, however, it is widely accepted many primary care professionals will not be confident diagnosing AF on an ECG and final analysis must rely on clinical judgement and not the inbuilt analysis tool which provides 3 options – possible atrial fibrillation, unclassified or normal. Access to trained clinicians who can accurately detect AF on either a 12 -lead or single lead ECG, would need to be factored in to a community based AF detection scheme.1 This could also reduce the number of false negatives and false positives.15
Lead-I ECG technology is continually developing and clinicians will be faced with its use more and more. Appropriate training and correct support with interpretation will increase user confidence. However, AF screening can only be effective if clinical pathways are in place to ensure appropriate anticoagulation treatment is implemented.2
Consideration should also be given to the potential harms of AF screening. For example, if someone has asymptomatic AF and is at low stroke risk then they would not need treatment but would still be labelled as having a serious health problem, which may impact on any application for life or travel insurance.1 Patients will need to be made aware of the consequences of being screened – as they should be with any screening programme.
The increased risk of bleeding associated with anticoagulant therapy is another, important consideration. Careful assessment and discussion of the pros and cons with the patient is essential.1
Finally, workload in general practice is ever increasing and the sustainability of an AF screening programme will need some consideration.15
SELF-DIAGNOSED AF: WHAT DO WE ADVISE THE PATIENT?
The availability of wearable devices, such as the Apple Watch, which has been shown to have high positive predictive value, is likely to result in increased numbers of self-diagnosed cases of AF.16 Preliminary findings from The Apple Heart study (AHS), which enrolled over 420,000 people within a year, found the Apple Watch to have a positive predictive value of 84% and that it can assist in detecting AF.17 Furthermore, 20% of AF detected had a duration of 24 hours or more. However, The Food and Drug Administration (FDA) recommends it for consumer-use only. Likewise NICE does not recommend its use in the clinical setting, but accepts that findings from a consumer device is one of many things that may prompt an individual to seek advice from a health care professional.13 As the public embrace this technology we will see more people attending our clinic with self-diagnosed AF. So, what advice can we provide?
Despite a high predictive value revealed in the AHS, the study design has been challenged. Enrolling criteria for AHS applied to those who could afford to buy a smart watch paired with an iPhone. The demographics were therefore made up of the young and affluent, with an interest in gadgets. Of those enrolled, 80% were 55 years or younger and only 13% of participants had a CHA2DS2VASc of 2 or more.17
Consumer devices which lead to self-diagnosis may not always be in the patient’s best interest. However, patients will use them, and therefore should be encouraged to seek advice if data on their Apple Watch show AF.16 Clinicians should then consider further assessment for someone with a suspicion of having AF, with good history taking, cardiovascular examination and assessment of risk factors.16 Given the younger age group seen in the study it is likely that many individuals will be at low risk of stroke and can be reassured that treatment is not indicated at this stage, even if AF is confirmed. Furthermore, the patient may well decline further investigations to avoid being labelled with a serious condition at an early age.
UNDERTREATED AF
As well as detecting asymptomatic AF, capturing ‘undertreated’ AF is equally important. It is estimated there are approximately 147,000 people in England with AF who are still not receiving appropriate treatment. Up to half of those with AF who suffer a stroke were not taking anticoagulants prior to their stroke.18
NHS England has recently launched a £9 million investment to fund a scheme to trial new ways of improving uptake of treatment in those with AF.18 Patients – or their records – will be reviewed by a specialist nurse or pharmacist, and then treatment recommendations will be conveyed to the GP. Recommendations may be delivered face to face or via a virtual clinic. The GP can then discuss treatment options with the patient and together, they can make a joint decision on best course of action.
So far, 23 CCGs have agreed to participate in the programme. The specialist pharmacist and anticoagulation nurses will be responsible for collecting data from their clinics. This will be collated and anonymised by the CCG on a quarterly basis and sent off for analysis and interpretation.
The pilot will run until 2020, and if successful the programme will be implemented across more CCGs in the future. Training and education support for the virtual clinic will be delivered by the Academic Health Science Networks (ANSNs).
The programme links into the NHS long term plan which aims to prevent 150,000 heart attacks, strokes and dementia cases over the next 10 years.
CONCLUSION
It is evident that before a national screening programme is launched, more robust evidence from randomised control trials is needed to determine if AF screening will reduce cardiovascular morbidity and mortality.1 We await results of ongoing research to provide clarity. In the meantime, with increased availability of oral anticoagulants as well as innovative ECG devices that are easy to use, cost effective and reduce workload, we should take advantage of the opportunities to screen for AF in the community. Clinicians should be guided by current national and European guidelines advocating screening in a target population, 65 years or above, or those with symptoms. Updated clinical pathways should be available to maximise effects of screening.
Due to the increased use of wearable devices, such as the Apple Watch, we are likely to encounter more patients self-diagnosing and seeking advice from a clinician.
Finally, primary care, as the first port of call for patients, has a vital role to play in helping detect undiagnosed AF in the community, as well as ensuring that those diagnosed are appropriately treated. Primary care has a vital role in ensuring the success of NHS England’s national project to improve uptake of treatment in undertreated AF,18 thus helping to prevent up to 700 strokes and approximately 200 deaths.
REFERENCES
1. Lown M, Moran P. Should we screen for atrial fibrillation. BMJ 2019;64:143 https://www.bmj.com/content/364/bmj.l43.full
2. Fay M, Fitzmaurice D, Freedman B. Screening for older patients for atrial fibrillation in general practice; Current evidence and its implications for future practice; Eur J G Pract 2017;23(1):246-253
3. Zelniker TA, Giugliano RP. Which patients with atrial fibrillation should receive anticoagulation? American College of Cardiology and Medscape. Medscape 29 March 2018. https://www.medscape.com/viewarticle/894235
4. Science Daily. BMJ. Should we screen people for irregular heartbeat? Science daily 13 February 2019. https://www.sciencedaily.com/releases/2019/02/190213192500.htm
5. NICE CG180. Atrial Fibrillation: management, 2014. https://www.nice.org.uk/guidance/cg180/evidence
6. Kirchhof P, Benussi, S, Kotecha D, et al. ESC guidelines for management of atrial fibrillation developed in collaboration with EACTS: Eur Heart J 2016;37: 2893-2962
7. Svennberg E, Engdahl J. Why should we screen for atrial fibrillation? Heart 2017;103:6-7
8. Nuffield Department of Primary Care Health Sciences. Can screening for AF prevent stroke? 16 May 2018. https://www.phc.ox.ac.uk/news/new-research-to-investigate-whether-screening-can-prevent-one-in-ten-strokes
9. Marini C, DeSantis F, Sacco S, et al. Contribution of atrial fibrillation to incidence and outcome of ischaemic stroke: results from a population-based study. Stroke 2005; 36(6): 1115-1119
10. Freedman B, Camm J, Calkins H, et al. Screening for atrial fibrillation: a report of the AF-Screen international collaboration. Circulation 2017;135(19):1851-67
11. Sentinel Stroke National Audit Programme. Clinical Audit April 2013- March 2018. Annual Public Report. National Results, June 2019. https://www.strokeaudit.org/Documents/National/Clinical/Apr2017Mar2018/Apr2017Mar2018-AnnualReport.aspx
12. Fitzmaurice DA, Hobbs FDR, Jowett S, et al . Screening verses routine practice in detection of Atrial fibrillation in patients aged 65 or over: cluster randomised controlled trial. BMJ 2007:335(7616):33
13. NICE Diagnostics guidance (DG35). Lead-I ECG devices for detecting symptomatic atrial fibrillation using single time point testing in primary care, May 2019. https://www.nice.org.uk/guidance/DG35
14. Orchard J, Freedman B, Lowres N, et al. iPhone ECG screening by practice nurses and receptionists for atrial fibrillation in general practice: the GP-SEARCH qualitative pilot study. Aust Fam Physician 2014;43(5):315-9
15. Mandrola M, Foy A. Downsides of detecting atrial fibrillation in asymptomatic patients: Am Fam Physician 2019;99(6):354-355
16. Hughes S. Apple Watch helps detect AF: is this the future? 27 March 2019. Medscape https://www.medscape.com/viewarticle/910509
17. Apple Heart study: Preliminary results. 2019 https://med.stanford.edu/news/all-news/2019/03/apple-heart-study-demonstrates-ability-of-wearable-technology.html
18. NHS England. Atrial fibrillation demonstrator site programme https://www.england.nhs.uk/ourwork/clinical-policy/cvd/af-demonstrator-site-programm
Related articles
View all Articles