Holistic care for patients with a cancer diagnosis
Jenny Aston
Jenny Aston
FRCGP (Hon), ALPN, RCNT, RN, QN
Advanced nurse practitioner, Cambridge
RCGP AHP/Nurse champion
Practice Nurse 2023;53(6):21-24
In addition to addressing the specific needs of patients with cancer, it is essential to ensure that other concurrent health conditions such as diabetes or menopause, are not neglected and that general practice nurses deliver comprehensive and patient-centred care
When a cancer diagnosis is made, much of the care understandably becomes centred around the patient’s hospital treatment, sometimes to the detriment of the management of other conditions. Taking a proactive approach means that we can manage these existing conditions effectively alongside treatment for cancer.
When referring a patient with a possible diagnosis of cancer it is really important to keep in touch with the patient soon after diagnosis, if only to say ‘we are still available to help’, even if most of their care will be carried out at the hospital. Offering to be a contact and to check in with them from time to time can be a real comfort to the patient.
In my experience, patients undergoing the process of a cancer diagnosis and going through treatment really appreciate knowing that you will keep in contact to see how they are doing and perhaps answer any questions they may have. Treatment for cancer can be all-consuming – patients need to know that they are also able to access the holistic care they need in the management of other conditions. As nurses in primary care, we can provide the care and reassurance that they need.
A TRUSTED VOICE
To your patient, everything at the hospital can be unfamiliar and scary, on top of the psychological effect of coming to terms with a cancer diagnosis. Patients may not understand the system and can be too frightened to ask, or do not want to ‘bother’ the hospital staff. The perception that hospitals and their staff are really important and that their time should not be wasted often leads to unnecessary worries. All of the medical terminology that they are newly faced with can be confusing and may need explaining before patients really take in what is happening. In my experience, patients often seem much more reassured by having things explained to them by someone they already know and trust, such as their general practice nurse (GPN).
MAKING LIFE EASIER
There is an understandable focus on the patient’s cancer treatment and really effective multi-disciplinary working provides continuity around management of a patient’s cancer, however other health issues may get forgotten. Patients often have really good support from their clinical nurse specialists (CNSs), but CNSs may lack knowledge of the patient’s other health conditions – for example diabetes, other long term conditions or the menopause. For the patient, regular contact with their GPN or simply the knowledge that they can book a call with them when they need support helps to remove the extra stress of trying to get a GP appointment.
Because the cancer treatment dominates everything, regular care of other health issues can get side tracked and attending appointments at the GP surgery may be hard to fit around hospital appointments. Screening, immunisations and annual long-term condition reviews often get missed; patients may be too tired due to their cancer treatment or feel unable to face the telephone system to book an appointment. Many patients may also be fearful of catching viruses in the waiting room due to their compromised immune system.
It requires understanding and some degree of flexibility to provide appointments, bearing in mind the patient’s concerns. Perhaps offering an appointment at the end of a clinic rather than in the middle may give a patient more confidence to attend. Providing good ongoing holistic care of their existing conditions can help to ensure that your patients are in the best physical health to cope with all the cancer treatment and to help with their recovery.
Other common ailments such a urinary infections or gynaecological issues can be very troubling for patients, so it is really important to make it easy for patients undergoing cancer treatment to access care.
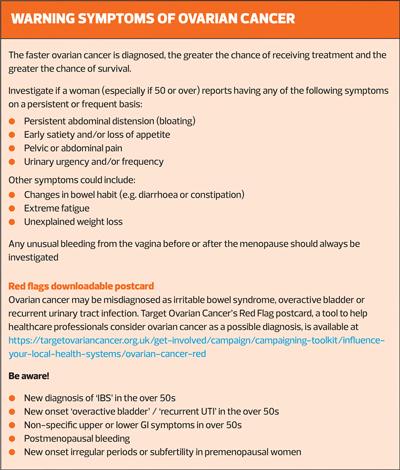
There may also be issues related to cancer treatment which need special consideration, for example, the physical and psychological effects of the ‘crash’ menopause which can be brought on by surgery and treatment for gynaecological cancers such as ovarian cancer.1 Alongside treatment, women need emotional support to cope with all the physical and psychological impact of surgically-induced menopause. Target Ovarian Cancer’s latest Pathfinder report found that 67% of women with ovarian cancer would have liked support dealing with surgical/early onset menopause.2 More than six in ten (62%) of those who said they would have liked support with menopause said that was not discussed with them, and almost the same number (63%) told the charity that they did not receive any treatment to ease their menopause symptoms.2
CASE STUDY: LACK OF SUPPORT FOR SURGICALLY-INDUCED MENOPAUSE
At 32 years old, Claire McKay went to see her GP after developing a new and persistent pain in her side. Alongside this pain, she was bloated and generally wasn't feeling well. Gynae cancer wasn't on her radar, she didn't know anything about ovarian cancer or its symptoms but as someone with type 1 diabetes she could recognise that something wasn't right. Since her diagnosis of stage I ovarian cancer and surgery in 2014, Claire has been campaigning for more awareness and support for women who have surgically induced menopause
‘At the age of 33 I had undergone a radical hysterectomy. I would never be pregnant, and I was faced with early onset menopause. My world was turned upside down.
‘It soon became apparent that I really did not fit the mould of someone experiencing menopause, something that has continued through the whole of my journey. After a week in hospital I was discharged on the promise I would be seen in three months to discuss HRT. I had very little understanding of the menopause at this point. I was experiencing debilitating side effects and went to the GP with what I thought was a heart attack. I feel very lucky that I had the support of my GP but it did feel like I had fallen off a cliff. Although the physical recovery wasn’t too bad, mentally it was much harder. The emotional impact of being so young and going through the menopause was painful: children had never been a priority for me but I felt I’d had the decision taken away from me. That was hard.
‘That’s why I now work with charities such as Target Ovarian Cancer – the charity has given me a voice and helped me turn a traumatic situation into one where I feel I am making a difference.’
In the primary care setting, group menopause clinics can be effective in supporting women. For women who are facing being plunged into early menopause due to surgery or treatment for ovarian cancer for example, it can be a very traumatic experience on top of their cancer diagnosis with its range of debilitating side-effects. Group menopause clinics can offer a lifeline to women as people feel more confident and comfortable when they’re in a group going through similar experiences, in a safe and supportive clinical environment.
A STRUCTURED APPROACH TO FOLLOW UP
To ensure that women going through cancer treatment while trying to manage other conditions don’t get ‘lost in the system’, I set myself scheduled tasks to follow up with my patients. For example, in a case of diabetes management, you could consider setting reminders to send follow up texts to the patients to check on how they are doing. Sometimes it’s easier to do it by phone, however I suggest speaking to them in the initial consultation to ask how they would prefer to be contacted.
Think about what suits your patient best, for example: ‘If I can't get hold of you by phone, can I send you a text and you can reply to it?’ Texts are minimally intrusive, can be replied to if they have any concerns (so they have a reliable point of contact), and help you to ensure that management of existing conditions doesn’t fall by the wayside of the all-consuming cancer treatment. It’s very important that as GPNs we help patients undergoing cancer treatment to understand that they will feel better overall if we can manage their other health conditions as well.
GPNs also have an important role helping patients to maintain a healthy lifestyle, as this will be a real help with coping with, and possibly having better response to, treatments.
IN SUMMARY
GPNs have the unique opportunity to guide patients through their cancer journey while addressing other health conditions they may face, such as diabetes and menopause. By staying informed, coordinating care, and offering emotional support, you can significantly improve the quality of life for these women and empower them to navigate the complex landscape of their health.
Being a point of contact, someone who your patient recognises as someone who is on their side, can make all the difference in their lives by providing them with the comprehensive care they need during their most vulnerable moments. Even once the initial cancer treatment is over, it is important that, as nurses, we are available to listen to patient concerns and that we follow up in the ways I have described above. We know that patients really value and remember kindness and being listened to, as much as good clinical care.
REFERENCES
1. Maggie’s Cancer Centre. Menopause - an overlooked side effect of cancer treatment. https://www.maggies.org/about-us/cancer-and-crash-menopause/
2. Target Ovarian Cancer. Pathfinder 2022: faster, further, fairer;2022. https://targetovariancancer.org.uk/sites/default/files/2022-10/Target%20Ovarian%20Cancer%20Pathfinder2022.pdf
Related articles
View all Articles