Checking for head and neck cancers: a guide for GPNs
Michelle Vickers
Michelle Vickers
CEO Head & Neck Cancer Foundation
Practice Nurse 2021;51(10):12-14
With the current lack of training and awareness surrounding head and neck cancers, it is more important than ever for us to grow the wider diagnosis team to encompass general practice nurses
Every day in the UK, 34 people receive the devastating news that they have been diagnosed with a head and neck cancer.1 This is one of the fastest growing cancer types, accounting for 3-4% of all cancers and is the eighth most common type. Despite this, head and neck cancers are lesser known and largely ignored when compared to more prolific cancer groups such as breast cancer.
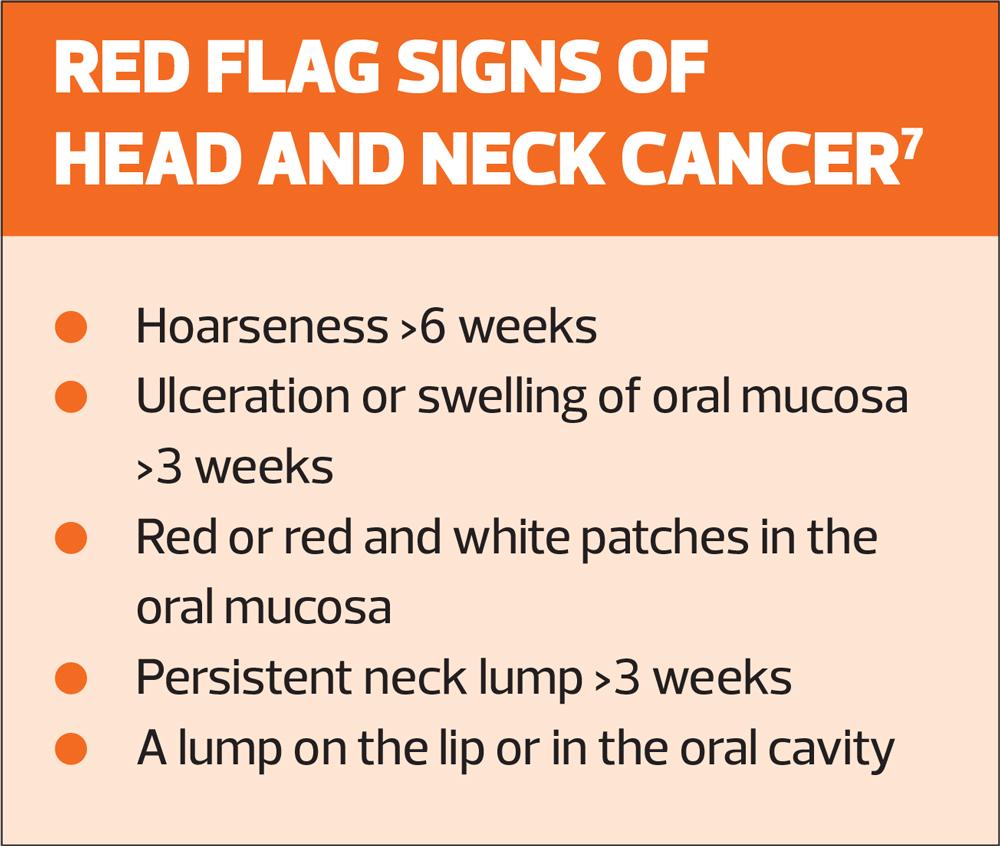
Because of this, the public and medical professionals alike are much less educated on the signs of head and neck cancers. In fact, one of the issues in the medical field that can lead to a late diagnosis is the general lack of training in spotting these signs among dentists, practice nurses, GPs and other medical professionals. This is so important because an early diagnosis of head and neck cancers can increase survival rates of patients by up to 95%.
On behalf of the Head & Neck Cancer Foundation (HNCF) I want to call for more action among the medical community to train staff in spotting these signs to increase the overall diagnostic team and improve outcomes for patients. I feel this is especially important now following the COVID-19 pandemic. The patient backlog and huge number of missed cancer diagnoses that have built up due to coronavirus mean that many of those with undiagnosed head and neck cancers will be verging further away from an early diagnosis every day. It is important now more than ever that all medical professionals learn how to spot the signs of these types of cancers to allow for better survival rates.
The Head & Neck Cancer Foundation was set up to improve outcomes for patients with head and neck cancers. We have two main goals: to fund the technology and training needed to implement groundbreaking new treatments, and to raise general awareness of these cancers and how to check for them. So far we have accomplished amazing things such as pioneering and funding equipment for Sentinel Node Biopsy, which is a now-widespread treatment and can save over 70% of patients from enduring a neck dissection. Throughout our time in operation, however, it has come to light that there is a worrying lack of awareness and training in spotting the signs of head and neck cancers among all key parties, including nurses, dentists and GPs.
The charity’s GP Champion actually experienced the consequences of this lack of training first hand, with his own mother. Despite years of medical training, he missed his own mother’s oral cancer despite her asking his opinion of her symptoms as the training did not cover these signs and their relation to oral cancer. Her diagnosis was then delayed further due to an incorrect referral by her dentist. This experience opened his eyes to how many patients may be at risk due to the fact that the key signs of these cancers are simply not taught. He is now running a training programme with the charity’s Founder, Professor Mark McGurk, in hopes to educate more GPs on how to carry out simple mouth checks and identify any areas of concern.
Many nurses will be familiar with the signs of breast and prostate cancer, however may have little to no knowledge on head and neck cancers. This is why we want to educate nurses to become part of the wider diagnostic team, enabling them to carry out quick checks on concerned patients, point out anything of concern or identify any issues as potential cancer symptoms.
The most common type of head and neck cancer is squamous cell carcinoma. About 9 out of 10 head and neck cancers (90%) start in squamous cells.2 Squamous cells line the mouth, nose and throat. Mouth cancer is where a tumour develops in the lining of the mouth. This may be on the tongue, the insides of the cheeks, the roof of the mouth, or on the lips or gums. In other words, there are many areas that tumours can develop which are difficult for sufferers to spot on their own. While squamous cell carcinoma is the most common form, the type of mouth cancer depends on which cell the cancer starts from.
EXTERNAL CHECK
I believe that all medical professionals should know how to do a quick and easy check that saves lives. There are some signs that can be spotted externally that all medical professionals should know, however the main thing is that they are able to carry out a quick and thorough check if a patient raises a concern. This first check allows nurses to examine a patient for external signs of cancer should they have a concern. While carrying out each of these steps, it is important to talk through what you are doing with the patient so that they can learn how to check themselves and increase the chances of spotting something.
Look at the face
The first place to examine on a patient is their face: any unusual swelling can be an initial sign of cancer. Communication is key as the patient will know what is normal for them. Next, the skin can be examined for any moles that have become larger or started to itch or bleed. While carrying out this check, asking the patient to turn their head will stretch their skin over the muscles and make it easier for lumps and abnormalities to be spotted.
Feel the neck
Next on the list is to feel their neck and the best way to do this is to run the fingers under the patient’s jaw and feel along the large muscle either side of the neck using the balls of the fingers.
Again, the aim of this is to check for any lumps or swollen areas and that everything feels the same on both sides.
Mouth check
After checking the face and neck, performing a quick mouth check will allow the examiner to cover all bases. The steps below can all be done by either a medical professional or the patient themselves. This check is best done regularly so the key thing is to reiterate how important it is for patients to take home this knowledge and regularly check themselves. The more frequently these checks are done, the more a person will become familiar with their unique mouth, leading to faster identification of issues and ultimately an earlier diagnosis.
We have also created a video that works as a great resource to share with nurses and patients alike, which can be viewed at https://www.youtube.com/watch?v=t-GeHCIL7-A&t=2s. The video is two minutes long and has been viewed over three million times across YouTube and social media, undoubtedly saving lives.
Check the lips
The next step is to feel around the inside of the lips and along the gum line. Any ulcers or lumps that have been present for more than two weeks or that have changed in texture should be a concern. This step is best done frequently so it is a good idea to encourage patients to check their lips every two to three weeks as they brush their teeth, and much more often if they identify something that concerns them. This way patients will understand what is normal in their mouth and when to contact a medical professional.
Feel the cheeks
Next, either the patient or nurse can check the cheeks depending on what the patient is comfortable with. Both the inside and outside of the cheeks need to be felt, and they should feel the same on both sides. It is important to get as good of a look as possible too. Items of concern include red or white patches, lumps, ulcers or tenderness.
Examine the roof of the mouth
This next step is best carried out once a week so it is important to reiterate this to the patient. Look for ulcers or changes in colour and texture in the roof and inside of the mouth. The best way to do this is to ask the person you are examining to tilt their head back and open their mouth wide. This can also easily be done themselves by looking in the mirror and should form a weekly routine, which will allow them to familiarise themselves with what is normal within their mouth.
Check the tongue
When it comes to risk areas, the tongue is also a place of concern. Check both sides of the tongue carefully and the floor of the mouth for any abnormalities as these are the areas of the mouth that are most at risk. Abnormalities can include red or white patches, or lumps or numb spots.
Other signs to look out for include loose teeth, halitosis, numbness or unusual feeling on the lip or tongue and any unexplained change in speech, such as a lisp, all of these present a concern and are worth referring on, so that a cause can be determined.
If you spot anything at all that concerns you during an examination, or if you are unsure about a potential sign it is imperative that you refer to a GP, dentist or specialist straight away. Utilising medical connections is so important. I have seen first hand how easily the signs can slip past busy medical professionals. In this current state where there is a lack of training and awareness surrounding head and neck cancers, it is more important than ever for us to grow the wider diagnosis team to encompass nurses and other medical team members.
PREVENTING HEAD AND NECK CANCERS
While I do believe that all nurses should be taught how to spot the signs of head and neck cancers, I think that the education shouldn’t stop there. One of the most effective defences we have against cancers is prevention, and there are a few ways that head and neck cancers can be prevented about which I think nurses should know. The first is the role of the HPV vaccination in preventing these types of cancers. It is important to remember that HPV can lead to not only cervical cancer in women, but also to oral or oropharyngeal cancer.3,4
A large percentage of these cancers are caused by HPV so encouraging uptake in the vaccine is a great way to prevent these types of cancers.
Other factors that can worsen a person’s chances of developing a cancer in the mouth or throat are alcohol use and smoking tobacco. The risk for developing squamous cell carcinoma is worsened by roughly ten times for smokers compared to non-smokers. With this information nurses will be able to offer better advice and support to smokers and heavy drinkers. A great way to help a person quit or reduce their levels of smoking is to redirect them to services such as an NHS stop smoking service or to resources such as Smokefree (https://smokefree.gov) so that they can reduce their risk of developing cancer.
SUPPORTING PATIENTS
On the other side of prevention is supporting the patients who are already going through treatment. These types of cancers can be especially difficult as treatment can lead to disfigurement in the face, a loss of senses such as taste, smell, sight and feeling in the face, as well as a loss of certain functions such as speech or eating. This can be particularly hard on patients, and nurses play a key role in offering support.
Many oral cancer patients who undergo radiotherapy treatment will suffer a loss in taste and commonly used ingredients may burn their mouths. This can lead to many oral cancer patients choosing to eat alone, due to their special dietary requirements. Because of this, we have created a bank of recipe videos curated by Dr Phillipe Katz, a specialist in the examination of salivary glands, and a passionate cook. These recipes are specially designed for cancer patients and their families to enjoy together. There are also many other resources that can be shared with patients, such as the Life Kitchen cookbook, that was created by the amazing Ryan Riley to benefit these patients.5
In addition to this, we have created an online patient support group which takes place on Facebook and has proven beneficial for hundreds of head and neck cancer patients. This offers patients a feeling of community and understanding that no medical professional is able to offer, and members will often give each other support or share tips that helped them cope. It is essential for nurses to know of these kinds of resources and to be able to share them with cancer patients because they really do make a difference for somebody who is struggling.
CONCLUSION
Head and neck cancers are a group of cancers that are lesser known and sometimes forgotten or ignored; however, they are so common and can have such an impact on a person’s life, often resulting in facial disfigurement and loss of senses, that it is vital to improve early diagnosis. Nurses participate in a high level of patient interaction and therefore can play a key role in the wider diagnosis team. You have a unique chance to identify and examine signs of head and neck cancers, knowledge really is power and I believe that all nurses should know how to perform a quick and easy mouth check. I hope that reading this has helped you and I encourage you to put a mouth check into practice, either on yourself, a colleague or friend. Sharing this knowledge is the best way that we can reach more early diagnoses and improve patient outcomes.
I also want to encourage you to take a quick look at our website, which hosts a bank of resources that can be used to educate yourself and share with patients. This includes resources on performing a mouth check, oral cancer patient-friendly recipes, self-diagnosis information and links to our patient community. You can view our website at https://hncf.org.uk.
REFERENCES
1. Cancer Research UK. Head and neck cancers statistics. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/head-and-neck-cancers#heading-Zero
2. Johnson DE, Burtness B, René Leemans C, et al. Head and neck squamous cell carcinoma. Nature Reviews Disease Primers 2020;6:92 https://www.nature.com/articles/s41572-020-00224-3
3. Agalliu I, Gapstur S, Chen Z, et al. Associations of oral a-, b, and y-human papilloma types with risk of incident head and neck cancer. JAMA Oncol 2016;2(5):599-606
4. Schlecht NF, Masika M, Diaz A, et al. Risk of oral human papilloma virus infection among sexually active female adolescents receiving the quadrivalent vaccine. JAMA Netw Open 2019;2(10):e19114031. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2753522?utm_source=F
5. Riley R, Duke K. Taste & Flavour – Digital book. https://lifekitchen.co.uk/product/taste-flavour-digital-book/
6. Silva P, Harker N. Head and neck cancer: early diagnosis and treatment are key. Guidelines in Practice: 2018. https://www.guidelinesinpractice.co.uk/cancer/head-and-neck-cancer-early-diagnosis-and-treatment-are-key/453995.article
7. NICE CKS. Head and neck cancers: recognition and referral; 2021. https://cks.nice.org.uk/topics/head-neck-cancers-recognition-referral/
Related articles
View all Articles