A team approach to getting the basics right in asthma management
Darush Attar-Zadeh
Darush Attar-Zadeh
BPharm MFRPSII
PCRS Executive Committee Member
Barnet CCG, RPS-LNW & RightBreathe Respiratory Lead Pharmacist
Practice and community pharmacists can play an integral role in the multidisciplinary team and contribute to the provision of optimal care to people with asthma, from demonstrating inhaler technique to leading education initiatives in schools
People living with long term conditions including cardiovascular diseases, cancer, chronic kidney disease (CKD), arthritis, chronic respiratory diseases (such as chronic obstructive pulmonary disease [COPD] and asthma) require appropriate care and management.
The most recent Asthma UK survey highlighted that 60% of patients with asthma don’t receive basic asthma care, which should include an inhaler technique check, an up to date Personal Asthma Action Plan (PAAP) and an annual asthma review.1
People living with asthma can lead normal productive lives, but not if their asthma isn’t well controlled, when it can lead to day and night time symptoms, interference with school or work activities and an increased reliance on short acting B2 agonists (SABA), as well as having a profound impact on the individual’s mental health.
Studies show that 40-80% of medical information provided by healthcare practitioners is forgotten immediately. The greater the amount of information presented, the lower the proportion correctly recalled; furthermore, almost half of the information that is remembered is incorrect.2
People with asthma may require several educational contacts with different health care providers to accompany a co-created PAAP to aid them better manage their condition.
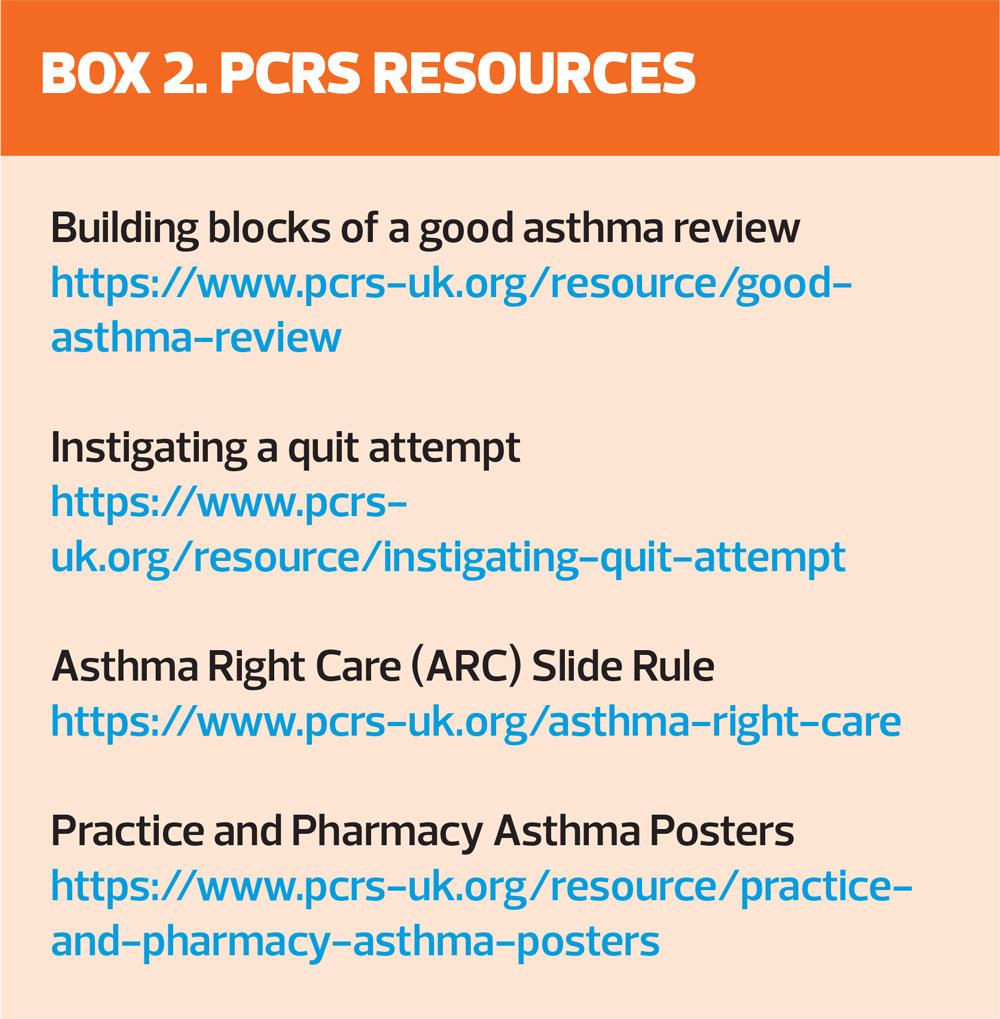
This article will focus on examples of how collaboration can work in practice. It will also highlight a number of Primary Care Respiratory Society (PCRS) resources that can help clinical team members with an interest in respiratory diseases learn more and build up their competency, knowledge and skills to safely care for patients.
Collaborative working
The NHS Long Term Plan (LTP) encourages more collaboration between GPs, their teams and community services, working as primary care networks (PCNs), to increase the services they can provide jointly, and increase the focus on NHS organisations working with their local partners, as Integrated Care Systems.3
General practice nurses, GPs, GP-based pharmacists, healthcare assistants (HCAs), physician associates, school nurses, community pharmacy teams – all will come in contact with people with asthma and there will always be opportunities to bolster people’s asthma knowledge in addition to the information that some patients may gather online, or by calling the Asthma UK helpline.4
It’s a good idea for practice nurses to get to know their local community pharmacists and discover what respiratory training they have had. The UK Inhaler Group5 uses a framework to set, assess and support the standards of those initiating inhaler therapies and checking inhaler techniques and many pharmacy teams across the country will follow these standards.
HOW COMMUNITY PHARMACISTS CAN GET INVOLVED
Inhaler training workshops
There are many ways in which community pharmacists can get involved in the delivery of care to people with asthma. For example, the Middlesex Group of Local Pharmaceutical Committees (LPCs) has run a series of hands-on inhaler training workshops that cover nine boroughs across London.
Asthma and COPD projects
The Royal Pharmaceutical Society London North West (RPS-LNW) has carried out educational sessions for asthma and COPD patients in 2015 and 2019, which have gained peer recognition for the way the sessions use the multidisciplinary workforce.6
Of the 135 patients in the COPD project, 75 patients received inhaler technique coaching and 88 were offered medicines use reviews. Pulmonary rehabilitation was discussed with 104 patients. Before the intervention, inhaler technique and adherence in this patient group had been identified as poor and only 24% of the patients reported having previously been offered pulmonary rehabilitation. Of the 39 smokers in the patient group, 32 were referred to smoking cessation services.6
Data for the 2019 asthma project have not yet been fully analysed, but interim findings suggest that the proportion of patients presenting at the first consultation with a PAAP is very low (provisionally less than 15%), that a high proportion valued the opportunity to talk to a pharmacist, and there was qualitative evidence of good patient engagement levels. The proportion of current smokers was about 19%. Virtually all the patients had their inhaler use checked, with support provided as needed.6
Inhaler technique is of paramount importance because the way a patient uses a device is proportional to the amount of drug they will deposit in their lungs, which in turn has a direct correlation with poor respiratory disease control and emergency hospital attendance.7
Medicines Optimisation (MO) Teams
Good value comes when you can achieve good health outcomes at the lowest possible cost. In 2018, Barnet CCG spend on medicines for respiratory conditions reduced by 15.79% to £4.16 million compared with 2016. The average drop in spend for England was 12.45% over the same period.8 These savings are used to further enhance the on-going CCG education programme. All the PCNs in Barnet are assigned a MO pharmacist who is a key player in making practices aware of areas of local improvement where medicines can potentially be harmful or of low value. These can usually be identified by searching national and local databases such as the NHS Business Services Authority ePACT2.8
Asthma-friendly schools education
Asthma is the most common chronic health condition in children, causing significant illness and death. It affects 9% of UK primary school children (roughly 3 children in every classroom).9 Training sessions in Barnet are delivered by a local GP, practice nurse, local public health stop smoking manager, paediatric respiratory consultant and Asthma Right Care (ARC)10 respiratory lead pharmacist. The fun and interactive, hands-on session covers topics such as What is asthma?, Triggers (including passive smoking), How to recognise signs of an attack, Inhaler technique for emergency inhalers and spacers, and How to manage an asthma attack. Each session also provides resources that can then be rolled out to the rest of the staff in the school. One event in 2019 attracted teaching staff from 45 schools in Barnet, with a reach of 20,000 children.
Teach-the-teacher group workshops
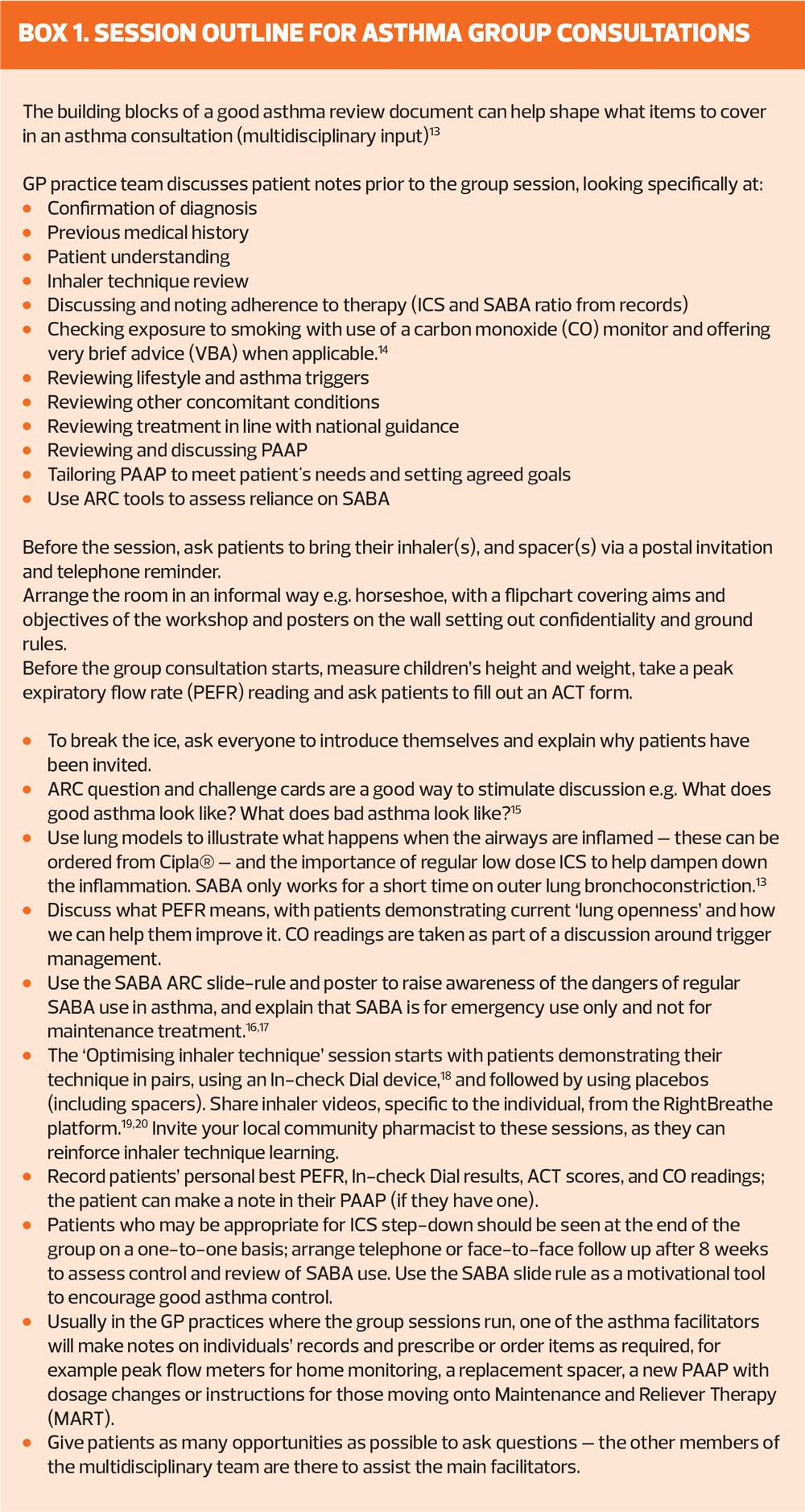
Patients with asthma who are at risk of future asthma attacks e.g. over-reliant on SABA, not attending an annual asthma review, no evidence of a PAAP, on high doses of ICS or who have received oral steroids for asthma, were invited to group consultations and followed up afterwards by skilled respiratory GP practice team members.11
In one GP practice, with 403 patients on its asthma register in 2019, high dose inhaled corticosteroid (ICS) prescribing was reduced by 12% in 3 months with no deterioration in asthma control test (ACT)12 scores on follow-up visits. This has involved a dedicated team including the lead GP, CCG pharmacist, practice nurse, HCA and GP-based pharmacist/data analyst. Local community pharmacy and GP practice staff are welcomed to sit in on the sessions to learn and interact too.11
Patient feedback included comments such as:
- ‘First time anyone has explained to me how to take the inhaled medication’
- ‘Good to learn together’
- ‘Had not realised how important the technique is’
- ‘So good to have proper time and be able to ask questions’.11
Following the success of these one-hour group educational sessions in adults, the children and young person’s lead for the CCG co-ordinated group consultations following a similar format (Box 1).
In one practice, where nine children with asthma were seen with their parents, 100% said they would recommend group consultations to a friend. The session was designed to be fun with facilitators wearing Asthma Right Care T-shirts, using question and challenge playing cards and issuing badges and certificates to all children with their CO test readings.
Conclusion
Involving practice-based or local community pharmacists in the care of patients with asthma can help to reinforce education on inhaler technique and over-reliance on SABA, and contribute to improving outcomes for the patients, in terms of asthma control, and the practice and wider NHS, in terms of medication costs. Inviting pharmacists to participate in group consultations for asthma patients can also increase capacity to answer patients’ questions and ensure that they find the experience rewarding.
Acknowledgements
With thanks to Christine Heading PhD, RPS-LNW, for assistance with the preparation of data for the RPS project, and this article. Also to Colin Daff and other members of the Medicines Optimisation and Barnet CCG team; Dr Joanna Yong, GP and CYP lead, Barnet CCG; Dr Karen Grossmark, GP and PHGH team; Stephanie Bancroft RPS-LNW lead; Marsha Alter from the LPC; and PCRS colleagues
REFERENCES
1. Asthma UK. 2020. Annual asthma survey 2018. https://www.asthma.org.uk/support-us/campaigns/publications/survey/
2. Kessels RCP. Patients’ memory for medical information J Royal Society of Medicine 2003 96(5) 219-222. DOI: 10.1258/jrsm.96.5.219
3. NHS. The NHS Long-term plan – a summary. 2019 https://www.longtermplan.nhs.uk/wp-content/uploads/2019/01/the-nhs-long-term-plan-summary.pdf
4. Asthma UK. 2020. Asthma UK Helpline. https://www.asthma.org.uk/advice/resources/helpline/
5. UK Inhaler group. 2020. UKIG standards. https://ukiginhalerstandards.educationforhealth.org/ukig-standards/
6. Research award for North West London Local Practice Forum. The Pharmaceutical Journal October 2017; DOI: 10.1211/PJ.2017.20203774
7. Murphy A. How to help patients optimise their inhaler technique. The Pharmaceutical Journal July 2016;297(7891): DOI: 10.1211/PJ.2016.20201442
8. NHS Business Services Authority. ePACT2. https://www.nhsbsa.nhs.uk/epact2
9. Healthy London Partnership. Ask about asthma. https://www.healthylondon.org/our-work/children-young-people/asthma/askaboutasthma/
10. Asthma Right Care (ARC) https://www.pcrs-uk.org/asthma-right-care
11. PHGH Doctors Clinics and Services. 2020. https://www.phgh.co.uk/clinics-and-services.aspx?t=1
12. American Thoracic Society. Sleep related questionnaires : Asthma control test. 2020. https://www.thoracic.org/members/assemblies/assemblies/srn/questionaires/act.php
13. Primary Care Respiratory Society. The building blocks of a good asthma review in adults. https://www.pcrs-uk.org/sites/pcrs-uk.org/files/Building_blocks_good_
asthma_review.pdf
14. Primary Care Respiratory Society. Instigating a quit attempt. July Year? https://www.pcrs-uk.org/resource/instigating-quit-attempt
15. Primary Care Respiratory Society. Question and challenge practice. July Year? https://www.pcrs-uk.org/resource/question-and-challenge-practice
16. Primary Care Respiratory Society. Asthma Right Care (ARC) Slide Rule. https://www.pcrs-uk.org/asthma-right-care
17. Primary Care Respiratory Society. Practice and pharmacy asthma posters. https://www.pcrs-uk.org/resource/practice-and-pharmacy-asthma-posters
18. Clement-Clarke International. 2020. In-Check DIAL G16 https://shop.clement-clarke.com/ProductDetails/tabid/122/
ProductID/84/Default.aspx
19. RightBreathe. 2020 https://www.rightbreathe.com/
20. Attar-Zadeh D. What is Rightbreathe and how might patients benefit from it? Independent Nurse July 2018 http://www.independentnurse.co.uk/clinical-article/what-is-rightbreathe-and-how-might-patients-benefit-from-it/176417/
Related articles
View all Articles