Hypertension
INTRODUCTION
Almost a third of men and over a quarter of women in the UK have high blood pressure, and important risk factor for increased risk of cardiovascular disease. Accurate diagnosis and appropriate treatment are essential components of a strategy to reduce cardiovascular morbidity and mortality, together with the identification and management of other cardiovascular risk factors.
LEARNING OBJECTIVES
On completion of this module you will be better able to:
- Make a diagnosis of hypertension
- Identify patients who require antihypertensive treatment
- Reduce risk of cardiovascular morbidity and mortality by lowering blood pressure
- Identify appropriate blood pressure lowering drugs for people with hypertension
This resource is provided at an intermediate level. Read the article and answer the self-assessment questions, and reflect on what you have learned.Complete the resource to obtain a certificate to include in your revalidation portfolio. You should record the time spent on this resource in your CPD log.
Contents
Hypertension
Almost one third of men and over a quarter of women in the UK have high blood pressure/hypertension.
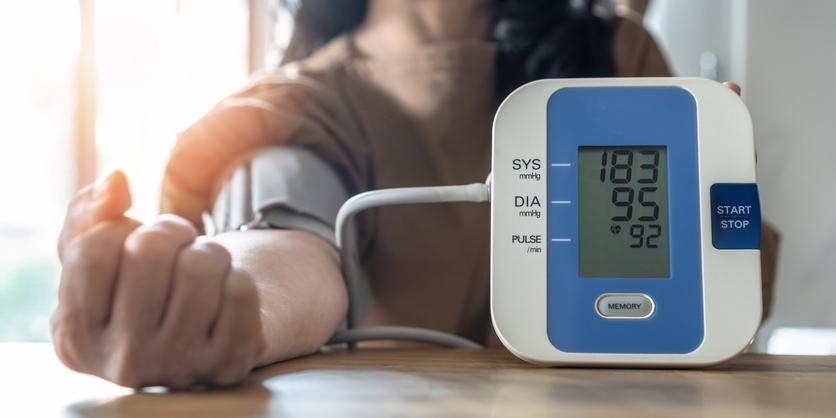
Hypertension is defined as persistently raised arterial blood pressure.
Hypertension is important as any increase in blood pressure is associated with an increase in cardiovascular disease risk.
The current standard threshold for suspecting hypertension is clinic systolic blood pressure sustained above or equal to 140 mmHg, or diastolic blood pressure sustained above or equal to 90 mmHg, or both. The diagnosis is then confirmed with ambulatory blood pressure monitoring (ABPM) or home blood pressure monitoring (HBPM).
Hypertension is classified according to severity:
- Stage one hypertension — clinic blood pressure at least 140/90mmHg, and subsequent ABPM daytime average or HBPM average at least 135/85mmHg.
- Stage two hypertension — clinic blood pressure at least 160/100mmHg, and subsequent ABPM daytime average or HBPM average is at least 150/95mmHg.
- Severe hypertension — clinic systolic blood pressure at least 180mmHg or clinic diastolic blood pressure at least 110mmHg.
Primary hypertension has no identifiable cause and is present in about 90% of people with hypertension.
Secondary hypertension, which affects 10% of people with raised blood pressure, is the result of a known underlying cause such as Conn's adenoma, renovascular disease, or phaeochromocytoma.
'White coat' hypertension is raised blood pressure when measured during consultations with clinicians, but normal when measured in other 'non-threatening' situations. 'White coat' hypertension occurs in approximately a third of people with mildly elevated blood pressure (140–159mmHg systolic and/or 90–99mmHg diastolic) measured in a clinical consultation.
RISK FACTORS
According to Public Health England the following are risk factors for hypertension
- Age – blood pressure tends to rise with advancing age.
- Gender – Up to about 65 years, women tend to have a lower blood pressure than men. Between 65 to 74 years of age, women tend to have a higher blood pressure.
- Genetic factors – research on twins suggest that up to 40% of variability in blood pressure may be explained by genetic factors.
- Social deprivation – people from the most deprived areas in England are 30% more likely to have hypertension than those from the least deprived.
- Lifestyle – smoking, excessive alcohol consumption, excess dietary salt, obesity, and lack of physical activity are associated with hypertension.
- Ethnicity – people of Black African and Black Caribbean origin are more likely to be diagnosed with hypertension. It is not known why this is the case.
- Anxiety and emotional stress – can raise blood pressure due to increased adrenaline and cortisol levels
COMPLICATIONS OF HYPERTENSION
Hypertension increases the risk of a number of conditions including:
- Heart failure.
- Coronary artery disease.
- Stroke.
- Chronic kidney disease.
- Peripheral arterial disease.
- Vascular dementia.
Hypertension is the single biggest risk factor for cardiovascular disease and related disability.
At least half of all heart attacks and strokes are associated with hypertension.
The risk associated with increasing blood pressure is continuous, with each 2mmHg rise in systolic blood pressure associated with a 7% increased risk of mortality from ischaemic heart disease and a 10% increased risk of mortality from stroke.
HOW TO MAKE A DIAGNOSIS OF HYPERTENSION
In order to accurately assess blood pressure remember that:
- Blood pressure should be measured in both arms. If the difference in readings between arms is more than 20 mmHg, repeat the measurements. If the difference in readings between arms remains more than 20mmHg on the second measurement, measure subsequent blood pressures in the arm with the higher reading.
- Automated devices may not measure blood pressure accurately if there is pulse irregularity (for example, due to atrial fibrillation). Palpate the radial or brachial pulse before measuring blood pressure. If pulse irregularity is present, measure blood pressure manually using direct auscultation over the brachial artery.
- If blood pressure measured in the clinic is 140/90mmHg or higher, take a second measurement during the consultation. If the second measurement is substantially different from the first, take a third measurement. Record the lower of the last two measurements as the clinic blood pressure.
The diagnosis of hypertension is likely if a patient’s clinic blood pressure is 140/90mmHg or higher.
Isolated systolic hypertension should be suspected in a person (especially over the age of 60 years) with systolic pressure of at least 160 mm Hg and diastolic pressure below 90mmHg.
The diagnosis should be confirmed with ambulatory blood pressure monitoring (ABPM), or home blood pressure monitoring (HBPM) if ABPM is not tolerated.
When using ABPM, ensure that at least two measurements per hour are taken during the person's usual waking hours and use the average value of at least 14 measurements.
When using home blood pressure monitoring (HBPM), ensure that:
- For each blood pressure recording, two consecutive measurements are taken, at least 1 minute apart and with the person seated.
- Blood pressure is recorded twice daily, ideally in the morning and evening.
- Blood pressure recording continues for at least 4 days, ideally for 7 days — discard the measurements taken on the first day and use the average value of all the remaining measurements.
SEVERITY OF HYPERTENSION
The severity of hypertension can be classified as follows
- Stage one hypertension — clinic blood pressure at least 140/90 mmHg, and subsequent ABPM daytime average or HBPM average at least 135/85 mmHg.
- Stage two hypertension — clinic blood pressure at least 160/100 mmHg, and subsequent ABPM daytime average or HBPM average is at least 150/95 mmHg.
- Severe hypertension — clinic systolic blood pressure at least 180 mmHg or clinic diastolic blood pressure at least 110 mmHg.
- Accelerated hypertension — clinic blood pressure usually higher than 180/110 mmHg with signs of papilloedema and/or retinal haemorrhage.
HOW TO MANAGE A PATIENT WITH HYPERTENSION
The management of hypertension is aligned with severity.
If the patient has severe hypertension, consider starting antihypertensive drug treatment immediately, before obtaining results of ambulatory blood pressure monitoring (ABPM) or home blood pressure monitoring (HBPM).
Examine the fundi for evidence of hypertensive retinopathy.
Refer the patient for same-day specialist care if they have:
- Accelerated hypertension – blood pressure higher than 180/110 mmHg with signs of papilloedema and/or retinal haemorrhage (accelerated hypertension).
- Suspected phaeochromocytoma (labile or postural hypotension, headache, palpitations, pallor, and diaphoresis).
For all other patients with hypertension:
Assess cardiovascular risk by
- Arranging measurement of serum total cholesterol and HDL cholesterol.
- Estimating the person's 10-year risk of developing cardiovascular disease (CVD) using the QRISK®3 https://qrisk.org
Carry out investigations for target organ damage and secondary causes of hypertension:
- Arrange 12-lead electrocardiography — to assess cardiac function and detect left ventricular hypertrophy.
- Test for haematuria, and arrange measurement of urine albumin: creatinine ratio, plasma glucose, electrolytes, creatinine, and estimated glomerular filtration rate— to exclude adrenal disease, chronic kidney disease, and diabetes.
- Consider the need for specialist investigations in people with signs and symptoms suggesting target organ damage or a secondary cause of hypertension.
Offer lifestyle advice on:
- Diet and exercise. Discourage excessive consumption of coffee and other caffeine-rich products. Encourage people to keep their dietary sodium intake low, either by reducing or substituting sodium salt.
- Stress management. Smoking — if the person smokes, offer support to help them stop.
- Alcohol consumption — encourage reduced intake if the person drinks excessively.
Offer information leaflets on hypertension and lifestyle advice
Management of hypertension – a stepwise and stage related approach
For patients with stage 1 hypertension (clinic blood pressure at least 140/90mmHg, and subsequent ABPM daytime average or HBPM average at least 135/85mmHg.)
For people aged under 40 years with no evidence of target organ damage, cardiovascular disease, renal disease, or diabetes, consider seeking specialist evaluation of secondary causes of hypertension and a more detailed assessment of potential target organ damage.
- Offer antihypertensive drug treatment to people aged under 80 years who have one or more of the following:
- Target organ damage
- Established cardiovascular disease
- Renal disease
- Diabetes
- A 10-year cardiovascular risk equivalent to 20% or greater
Management of hypertension – a stepwise and stage related approach
Offer antihypertensive drug treatment to people of any age with stage 2 hypertension (clinic blood pressure at least 160/100mmHg, and subsequent ABPM daytime average or HBPM average is at least 150/95mmHg).
Management of hypertension – a stepwise and stage related approach
Step 1 treatment
Offer people aged under 55 years treatment with an angiotensin-converting enzyme (ACE) inhibitor. If an ACE inhibitor is not tolerated (for example, because of cough), offer a low-cost ARB. Do not combine an ACE inhibitor with an ARB to treat hypertension.
Do not routinely prescribe ACE inhibitors or ARBs to pregnant women.
Offer people aged over 55 years, and black people of African or Caribbean origin of any age, treatment with a calcium-channel blocker (CCB). If a CCB is not suitable, for example because of oedema or intolerance, or if there is evidence of heart failure or a high risk of heart failure, offer a thiazide-like diuretic, such as chlortalidone (12.5–25.0 mg once daily) or indapamide (1.5 mg modified-release once daily or 2.5 mg once daily). When deciding on treatment, take into account any co-morbidities, especially in people aged over 80 years.
Beta-blockers are not a preferred initial therapy for hypertension. However, beta-blockers may be considered in younger people, particularly those with an intolerance or contraindication to ACE inhibitors and angiotensin II receptor antagonists, women of child-bearing potential, or people with evidence of increased sympathetic drive.
Note: if the person is already taking a beta-blocker for another indication (such as symptomatic angina or previous myocardial infarction), consider continuing the beta-blocker and adding new antihypertensive drugs as required using this stepwise approach.
If a beta-blocker and a second drug are required, add a calcium-channel blocker rather than a thiazide-like diuretic to reduce the person's risk of developing diabetes.
Step 2 treatment (if blood pressure is not controlled by step 1 treatment):
Offer treatment with a CCB in combination with either an ACE inhibitor or an ARB.
If a CCB is not suitable, for example because of oedema or intolerance, or if there is evidence of heart failure or a high risk of heart failure, offer a thiazide-like diuretic.
For black people of African or Caribbean family origin, consider an ARB in preference to an ACE inhibitor, in combination with a CCB.
Step 3 treatment (if blood pressure is not controlled by steps 1 or 2):
Step 3 treatment consists of a combination of an ACE inhibitor or angiotensin II receptor blocker, a calcium-channel blocker, and a thiazide-like diuretic.
Note: before considering step 3 treatment, review medication to ensure that the person is concordant with step 2 treatment and that it is at optimal or best tolerated doses.
Step 4 treatment (if clinic blood pressure remains higher than 140/90mmHg after ensuring that the person is concordant with treatment and that it is at optimal or best tolerated doses used in step 3 treatment):
Consider adding a fourth antihypertensive drug and/or seeking expert advice. Options for drug therapy include:
Low-dose spironolactone (25mg once daily) if the blood potassium level is 4.5mmol/l or lower (off-license use — informed consent should be obtained and documented). Use particular caution in people with a reduced estimated glomerular filtration rate because of increased risk of hyperkalaemia.
Higher-dose thiazide-like diuretic treatment if the blood potassium level is higher than 4.5 mmol/l. When using further diuretic therapy, monitor blood sodium and potassium and renal function within 1 month, and repeat as required thereafter.
An alpha- or beta-blocker if further diuretic therapy is contraindicated, not tolerated, or ineffective.
If blood pressure remains uncontrolled with the optimal or maximum tolerated doses of four drugs, seek expert advice if this has not yet been obtained.
Monitoring response
Use clinic blood pressure measurements to monitor the response to treatment or lifestyle modifications:
- For people who are being treated with lifestyle measures only, follow up every 3 or 4 months, until blood pressure is well controlled, or antihypertensive drug treatment is started.
- For people who are starting antihypertensive drug treatment, follow up after at least 4 weeks for treatment effects to stabilize (unless blood pressure needs to be lowered rapidly).
Aim for a target clinic blood pressure below 140/90mmHg in people aged under 80 years with treated hypertension.
Aim for a target clinic blood pressure below 150/90mmHg in people aged 80 years and over with treated hypertension.
For people identified as having a 'white-coat effect', consider ABPM or HBPM as an adjunct to clinic blood pressure measurements to monitor the response to treatment. When using ABPM or HBPM to monitor response to treatment, aim for a target average blood pressure during the person's usual waking hours of:
- Below 135/85mmHg for people aged under 80 years.
- Below 145/85mmHg for people aged 80 years and over.
Follow-up of patients with hypertension
At annual review, the following assessments should be undertaken
Discuss the person's lifestyle, symptoms, and medication, including any adverse effects.
If necessary, use interventions to overcome medication non-adherence, such as suggesting the recording of medicine-taking, encouraging monitoring of the condition, simplifying the dosing regimen, and/or using a multi-compartment medicines system.
Check clinic blood pressure. If blood pressure is above the target range, confirm that it is persistently raised by:
- Either, rechecking blood pressure on 2–3 occasions over the next few weeks or months depending on clinical judgement.
- Or, if a 'white coat effect' is suspected, consider ambulatory blood pressure monitoring (ABPM) or home blood pressure monitoring (HBPM).
If blood pressure is persistently raised above the target range, ensure that secondary causes for hypertension have been excluded, and consider additional antihypertensive drug treatment.
If blood pressure is within the target range but adverse effects of the current antihypertensive drug treatment are unacceptable, consider an alternative treatment.
If treatment is well tolerated, either, review the person in a further 12 months, or, consider a trial of stopping or reducing antihypertensive drug treatment.
Check renal function annually by measuring serum creatinine, electrolytes, and estimated glomerular filtration rate (eGFR), and dipstick urine to check for proteinuria.
If proteinuria is present, consider checking the urine albumin: creatinine ratio (ACR), ideally tested on a first-void morning urine sample.
If the eGFR is < 60 mL/min/1.73 m2 and/or the urinary ACR is ≥3mg/mmol, this is evidence of chronic kidney disease (CKD).
For people who are not on an antiplatelet drug or statin reassess their cardiovascular disease risk using the current QRISK® assessment tool.
Consider offering details of organisations where people with hypertension can share views and obtain information, such as the Blood Pressure Association — www.bpassoc.org.uk.
Causes of secondary hypertension
Approximately 10% of patients with hypertension have an identifiable cause. This is secondary hypertension.
There are many causes of secondary hypertension, the most common group relates to renal causes
Renal causes of secondary hypertension include
Chronic pyelonephritis – usually detected unexpectedly on ultrasonography when investigating hypertension.
Diabetic nephropathy – indicated by microalbuminuria or proteinuria.
Glomerulonephritis – often indicated by microscopic haematuria.
Polycystic kidney disease – suggested by an abdominal or flank mass, microscopic haematuria, or family history.
Obstructive uropathy – the person may have an abdominal or flank mass.
Renal cell carcinoma – classically the person may have haematuria, loin pain and a loin mass, but increasingly asymptomatic renal cell carcinoma is being picked up on ultrasonography or CT scan.
Causes of secondary hypertension
Other cause of secondary hypertension include:
- Vascular disease
- Endocrine
- Medication
- Miscellaneous other disease
Taking each of these in turn,
Vascular disorders that cause hypertension include:
- Coarctation of the aorta, which usually results in upper-limb hypertension. There can be a significant difference in blood pressure between the left and right arms. Other signs include absent or weak femoral pulses, radio-femoral delay, palpable collateral blood vessels in the back muscles, and a suprasternal murmur radiating through to the back.
- Renal artery stenosis – suspect this if the person has peripheral vascular disease and an abdominal bruit, or if blood pressure is resistant to treatment. Most cases are clinically silent (other than hypertension), but the condition should be suspected if the plasma renin level is increased.
Endocrine disorders that cause hypertension include:
- Primary hyperaldosteronism – probably the most common curable cause of hypertension. People usually present with hypokalaemia, alkalosis (elevated bicarbonate level), and plasma sodium level greater than 140 mmol/L, or a larger than expected decrease in serum potassium when using a low-dose thiazide-type diuretic. The symptoms may be non-specific, but rarely it may present with tetany, muscle weakness, nocturia, or polyuria. Treatment with a calcium-channel blocker can mask the features of primary hyperaldosteronism. After identification of a possible adrenal adenoma on computed tomography or magnetic resonance imaging, tertiary referral is required for confirmation of unilateral aldosterone excess and possible laparoscopic adrenalectomy.
- Phaeochromocytoma – people can present with intermittently high or labile blood pressure, or postural hypotension, headaches, sweating attacks, palpitations, or unexplained fever and abdominal pains. Alternatively, it can be asymptomatic. It is the rarest but most important cause of hypertension to diagnose, because malignant transformation or catastrophic haemorrhage from the tumour can be fatal.
- Cushing's syndrome – suspect this when clinical features are present (for example, truncal obesity and striae). It rarely presents as hypertension alone.
- Acromegaly – suspect this if clinical features are present (for example, enlargement of hands and feet, facial changes, sweating).
- Hypothyroidism – hypertension may result from altered levels of renin, angiotensin and aldosterone, and is associated with an increased diastolic blood pressure. Clinical features may include fatigue, weight gain, dry skin and hair loss, constipation, and muscle weakness.
- Hyperthyroidism – increased systolic blood pressure may result. Clinical features may include tremor, anxiety, sweating, weight loss, diarrhoea, and heat intolerance.
Drugs and other substances that can cause hypertension include:
- Alcohol – misuse of alcohol may be the most common individual secondary cause of hypertension. Features include variable hypertension that is resistant to commonly used drugs and that disappears within a week or two of complete abstinence.
- Nonsteroidal anti-inflammatory drugs
- Cocaine and other substances of abuse
- Combined oral contraceptive
- Corticosteroids
- Erythropoietin
- Leflunomide
- Liquorice
- Ciclosporin
- Sympathomimetics – found in some over-the-counter cough and cold remedies (for example ephedrine, phenylpropanolamine)
- Venlafaxine.
Other conditions which can cause hypertension include:
- Connective tissue disorders such as scleroderma, systemic lupus erythematosus, polyarteritis nodosa.
- Retroperitoneal fibrosis
- Obstructive sleep apnoea
Summary
During this module you have learned how to:
- Make a diagnosis of hypertension
- Identify people who require antihypertensive treatment
- Reduce their risk of cardiovascular morbidity and mortality by lowering blood pressure
- Identify appropriate blood pressure lowering drug treatments for people with hypertension
Audit suggestions
- Run a report on all patients in the practice with a BP reading over 140/90mmHg and who do not have a diagnosis of hypertension.
- Call these patients in for review and BP measurement.
- For those patients who have a further BP measurement over 140/90mmHg follow practice guidelines on follow up and review
- Gather data on each patient on further on follow up.
- How many new diagnoses of hypertension were made?
- How many required antihypertensive treatment
- Re-audit in 1 year
Resources
Dena Ettehad, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. The Lancet 2015;387(10022):957-967.
European Society of Hypertension, European Society of Cardiology 2007 guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology. Eur Heart J 2007;28(12):1462-1536.
NICE CG182. Chronic kidney disease (partial update). Early identification and management of chronic kidney disease in adults in primary and secondary care (full guideline), 2014 [Free Full-text]
NICE QS28, Hypertension in adults. 2015 [Free Full-text]
NICE CG127. Hypertension in adults: diagnosis and management, 2016. [Free Full-text]
Public Health England. Tackling high blood pressure: an update, 2018 . [Free Full-text]
Public Health England (2017) Health matters: combating high blood pressure. [Free Full-text]
Prodigy Patient. Information for patients. https://www.prodigy-patient.co.uk/online/
Related modules
View all Modules