COVID-19: Managing patients with symptoms in the community
NICE rapid guideline (NG163) 17 April 2020
NICE rapid guideline (NG163) 17 April 2020
This guideline was developed to provide recommendations for the management of patients with COVID-19 symptoms in the community, including at the end of life. In this rapidly evolving situation, it is based on existing national and international guidance and the advice of specialists working in the NHS with expertise and experience of treating patients during the pandemic
The key symptoms of COVID-19 are cough, fever, breathlessness, anxiety, delirium and agitation, and may also include fatigue, muscle aches and headache. Mild symptoms are likely to improve in a week.
Patients whose symptoms get worse should contact NHS 111 online
Minimise face-to-face contact
Face-to-face contact should be minimised, by:
- Offering telephone or video consultations whenever possible. See Changing the way we work: virtual consultations now and in the future {{2047}}
- Cutting non-essential face-to-face follow-up
- Using electronic prescriptions rather than paper
- Using alternative ways to deliver prescriptions such as pharmacy deliveries, postal services, NHS volunteers or drive through pick up points.
Treatment and care planning
Discuss the risks, benefits and possible outcomes of treatment options so patients can express their preferences about treatment and escalation plans – these discussions may need to take place remotely.
Put treatment escalation plans in place because patients may deteriorate rapidly and need urgent hospital admission.
Find out if patients with pre-existing advanced comorbidities have advance care plans or advance decisions to refuse treatment, including ‘do not attempt resuscitation’ decisions. Take account of these in planning care.
Consider:
- Not all patients with symptoms will have COVID-19
- The patient’s underlying health conditions, severity of the acute illness, and polypharmacy
- Older patients with comorbidities such as COPD, asthma, hypertension, cardiovascular disease and diabetes may have a higher risk of deteriorating and may need more intensive management, including hospital admission.
- Patients with severe symptoms may deteriorate rapidly and need urgent admission.
Managing cough
Older patients or those with comorbidities, frailty, impaired immunity or a reduced ability to cough and clear secretions are more likely to develop severe pneumonia, which could lead to respiratory failure and death.
Encourage patients with cough to avoid lying on their back which makes coughing ineffective.
Use simple measures first, e.g. a spoonful of honey. Consider short-term use of codeine linctus, codeine phosphate tablets or morphine sulfate oral solution to suppress coughing if it is distressing.
Managing fever
Fever is most common 5 days after exposure to infection. Patients should be advised to drink fluids regularly to avoid dehydration. Do not use antipyretics with the sole aim of reducing fever – but if patients have fever and other symptoms e.g. headache, myalgia advise them to take paracetamol in preference to NSAIDs such as ibuprofen.
Continue paracetamol (not exceeding recommended dose) only while fever and other symptoms are present.
Managing breathlessness
Severe breathlessness often causes anxiety, which can make breathlessness worse. Supportive care measures to help manage breathlessness include:
- Keeping the room cool; improve air circulation by opening a window. Do not use a fan, which may spread infection
- Encouraging relaxation and breathing techniques; changing body positioning:
- Relaxing and dropping the shoulders
- Sitting upright to improve ventilation and reduce airway obstruction
- Leaning forward with arms bracing a chair or knees and upper body supported can improve ventilatory capacity
- When available, consider a trial of oxygen therapy and assess whether breathlessness improves
For patients with signs or symptoms of pneumonia, see NICE COVID-19 rapid guideline on managing suspected or confirmed pneumonia in adults in the community
Identify and treat reversible causes of breathlessness, e.g. pulmonary oedema
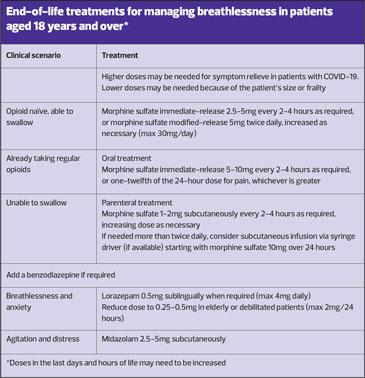
Consider an opioid and benzodiazepine combination for patients with COVID-19 who:
- Are at the end of life
- Have moderate to severe breathlessness
- Are distressed.
This combination is unlicensed in the UK. See the General Medical Council’s updated advice on off-label prescribing of opioids and benzodiazepines during the pandemic. Do not withhold sedation and opioids because of fear of causing respiratory depression.
Managing anxiety, delirium and agitation
Address and treat reversible causes of anxiety, delirium and agitation e.g. hypoxia, urinary retention and constipation. Consider trying a benzodiazepine to manage anxiety or agitation.
Reference
NICE NG163. COVID-19 rapid guideline: managing symptoms (including at the end of life) in the community; updated 17 April 2020