The need for awareness of all contraception options
Helen J Knox
Helen J Knox
RGN, PG Dip Social Innovation, Dip DN, A-08, FAETC
Clinical Nurse Specialist in Contraception, Sexual Health, Director of Midnight Learning Ltd – nurse-led education/training company and author of Sexplained® books
Eight out of ten women of reproductive age use regular contraception and the demand for contraceptive services is rising – but local authorities are reducing their spending, meaning general practice is being left to pick up the pieces. So it is more important than ever to be knowledgeable about all the options
According to the FPA (Family Planning Association),1 80% of reproductive age women in the UK using regular contraception and the number of women seeking appointments for contraception has risen in the last year by 37%, but half of local authorities have reduced their spending on contraceptive services.
Sexual health services in England is one of the largest areas of spending of the Public Health grant to local authorities, accounting for 17% (£611m).2 In the financial year 2016-17 local authorities report £174.5m was spent on contraception, of which £71.6m was spent in general practice. However, due to the £200m reduction to the Public Health budget, the Advisory Group on Contraception (AGC) recently reported half of local authorities have had to reduce their spending on contraceptive services over the last year.3
Councils have felt constant financial pressure to cut down their spending of the Public Health grant and as a result over 8 million women of reproductive age are living in an area where there have been significant cuts to contraceptive services. Cuts to these services could affect a woman’s access to a range of contraceptive methods. Data from the NHS on sexual and reproductive health (SRH) services in England, revealed prescriptions of LARC, the most effective and cost-effective methods of contraception, fell by 6% over the last three years.3
Throughout the UK, years of funding for research and increasing awareness of HIV, STI prevention programmes and teenage pregnancies, have resulted in considerably fewer cases with an impressive rate of return on investment. In fact, just £1 spent on contraception, has resulted in a saving of £9 over the last 10 years.2 Experts, however, now fear that a reduction in funding could undo the original hard work. While the cuts mean some women may ‘go private’, the vast majority cannot. Therefore, it is crucial for general practice nurses to be aware of all methods of contraception, to not only help advise correctly, but also reduce the workload of overburdened sexual health services.
CURRENTLY AVAILABLE METHODS
There are at least 15 methods of contraception currently available with most common forms of contraception being the oral contraception pill and barrier methods, such as the male condom. Other forms of contraception include:
- Caps or diaphragms
- Contraceptive implant
- Contraceptive injection
- Contraceptive patch
- Female condoms
- IUD (intrauterine device or coil)
- IUS (intrauterine system or hormonal coil)
- Male and female sterilisation
- Vaginal ring
CONTRACEPTION EFFECTIVENESS
A recent national survey of attitudes and lifestyles has shown that the highest risk of unplanned pregnancy was not – as you might expect – among teenage girls but in women at the beginning and end of the family building cycle.4 This group, 25–35-year olds, is also the age group that most commonly contacts sexual and reproductive health services for contraceptive advice.
According to NICE guidelines, although 88% of women aged 15-44 in a heterosexual relationship report using at least one method of contraception, an estimated 19% of pregnancies are unplanned.5 The contraceptive pill is the most common choice of contraception, however, studies suggest that as many as 47% of women do not take the pill properly.6
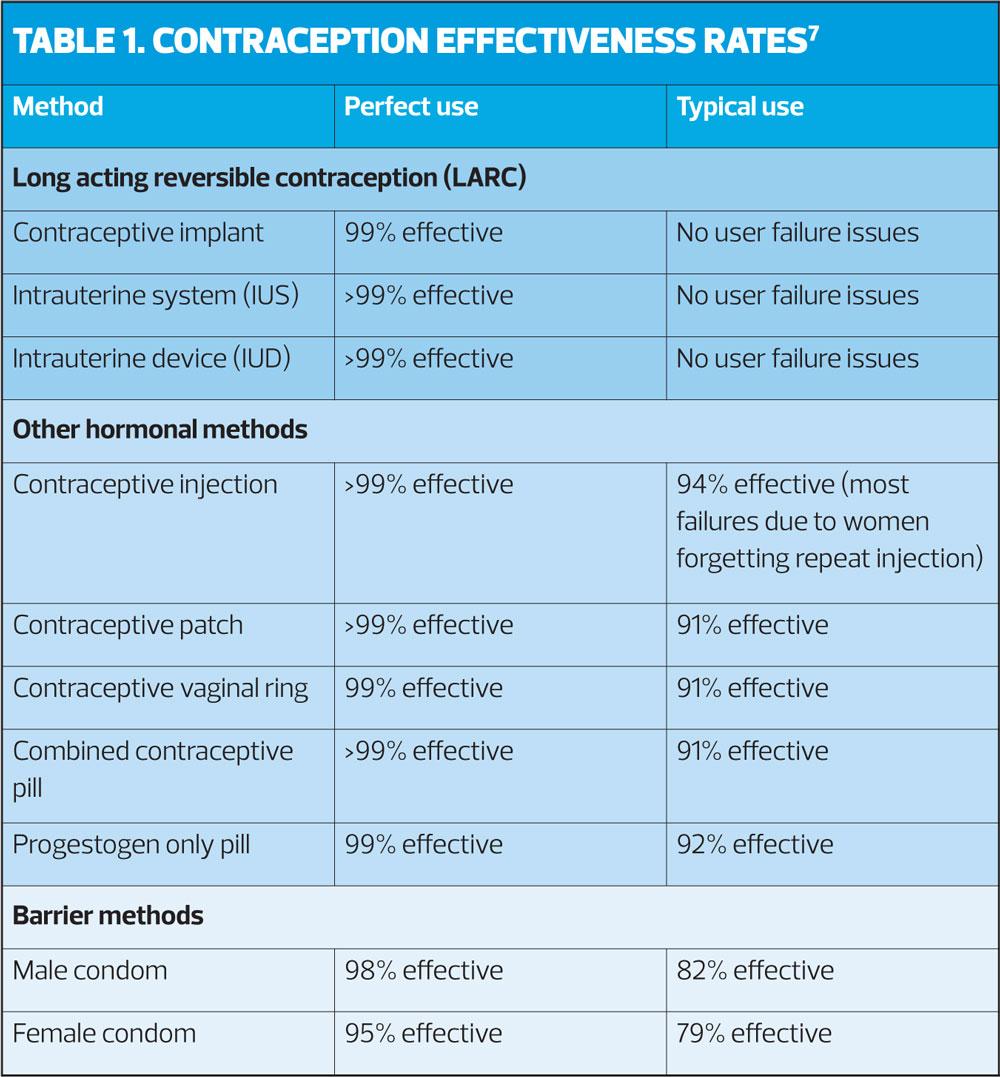
Different methods of contraception have different rates of efficacy, of which all nurses should be aware. The effectiveness of a contraceptive method depends on whether it is used correctly. Therefore, it is essential that nurses are aware of all forms of contraception where effectiveness is not dependent on user action, such as long-acting reversible contraception (LARC), which includes subdermal implants, intrauterine devices and intrauterine systems. Although progestogen-only injections do not require daily action, and (depending on the product) can last up to 13 weeks, this method does require the woman to remember to her repeat injection. LARC methods, progestogen-only injections and vaginal rings offer women more choice to fit around their lifestyles, which could improve adherence and therefore effectiveness.
Pearl Index
The most widely used system to measure the effectiveness of contraception is the Pearl Index. The lower the Pearl Index, the safer the method of contraception. The technique can also be used to compare different methods of contraception. Normally, results are shown as either ‘perfect use’, which is when the contraception has been used correctly or ‘typical use’. This is when the form of contraception has not been used correctly, for example, the missing of a pill.
No method of contraception is 100% effective, however as LARC methods require no daily action, their efficacy remains high. Effectiveness rates, according to the NHS,7 are shown in Table 1.
FSRH GUIDANCE
The Faculty of Sexual and Reproductive Healthcare has recently updated its guidance on use of the most commonly used form of contraception, the combined oral contraceptive pill (COC), in the light of research that revealed a withdrawal bleed of seven days is not medically necessary.8 COC regimens were originally designed to follow the same pattern as a women’s 28-day menstrual cycle. For 21 days active hormones are released, followed by 7-day rest period where a withdrawal bleed takes place and no pills or placebo pills are taken.9
While there is limited evidence of the long-term health effects of extended COC regimes, a Cochrane review concluded that extended regimens have similar safety profiles, participant satisfaction and participant adherence as the original dosing cycle.9 Nurses should therefore be aware that it is not medically necessary to have a break when taking the COC pill. It is also worth noting the possible advantages for taking COC continuously.
Taking the combined pill continuously reduces the frequency of HFI (hormone-free interval) bleeds. When the HFI is eliminated, it could reduce the risk of escape ovulation if not restarted promptly, and potentially contraception failure.8 During HFI, symptoms such as bloating, headaches and menstrual pain can appear more frequently, and studies have shown that extending COC regimens can help to reduce these symptoms. 9 Furthermore, bleeding patterns have been seen to be favourable with extended regimes, with most studies showing an overall decrease. Nurses should be aware that initial breakthrough bleeding may occur and seek guidance on how to handle this if unsure.
LARC METHODS
Long-acting, reversible contraception is a safe and effective way to control fertility, enabling women to have the sex life they want without the risk of pregnancy. An increase of LARC use could both reduce the number of unplanned pregnancies as well as ease the workload of overburdened sexual health services.
Over recent years LARC methods have slowly begun to increase in popularity. By 2013-14, 31% of women who spoke to a sexual health care professional, enquired about long-acting reversible contraception.5
LARC methods may be better suited to some women as the efficacy of oral contraception pills and barrier methods depend on their correct use every day or each time the person has sex, whereas LARC efficacy does not rely on it being correctly used every day.
Ease of use is key to contraceptive compliance and patients trust nurses to offer advice on the best choices for them depending on their lifestyle and priority of use, as well as helping them to understand how to use their chosen method effectively.
However, in light of the recent cuts more training is needed for nurses to help with the fittings of LARC methods. Self-fitting LARC-like methods require less training and fewer clinic appointments.
Vaginal rings
While some women would prefer to eliminate their menstrual bleed, others prefer for their contraception to mimic their natural cycle. Women looking for contraception that offers a menstrual bleed should be made aware of vaginal rings. They work like the COC but instead of taking the pill every day, the vaginal ring is used for 3 weeks in a row and then removed for one week to allow withdrawal bleeding. However, if no withdrawal bleed is desired, the FSRH states that vaginal rings can also be used continuously, with no need for an HFI.
A new vaginal ring, SyreniRing® became available last year. It releases a small amount of two female sex hormones, etonogestrel and ethinylestradiol, at a lower dose than the contraceptive pill or patch, resulting in fewer oestrogen-related side effects. The hormones prevent the release of an egg cell from the ovaries. Unlike the COC, the effectiveness of this method is not affected by vomiting or diarrhoea, but like the COC, may also help to ease premenstrual symptoms.
The clear flexible ring is easy to insert, in a similar way to a tampon and sits in the same place. The ring remains in place during sexual intercourse.
Women should also be made aware of the fact, that unlike other hormonal vaginal rings, SyreniRing® does not need to be refrigerated, which means that a 12-month supply can be issued at a time, helping to reduce return visits by 75% per year.
SyreniRing® also works out as cheaper for the NHS at £7.92 for one month, compared with other vaginal rings such as NuvaRing® at £10.73 per month.10
Women who are wanting to travel should also be aware of more convenient methods of contraception. Women travelling through different time zones who take the COC pill, should be reminded that they must take their pill approximately 24 hours after their most recent pill. Using the time zone in which the last pill was taken as a reference point. If a COC pill is not taken in the 24-hour period after it should have been taken, it is known as a missed pill. Several missed pills could increase the risk of ovulation. However, less thought is involved for women travelling and using vaginal rings or LARC methods.
CONCLUSION
In a time of cuts and lack of investment in sexual health services, a new method entering the market may help to reduce the need for so many return visits. Women should therefore be advised about the wider choices of contraception available, such as LARC methods, and she is suitable for combined hormonal contraception, vaginal rings.
However, more training options should be in place to help nurses to be able to advise on all methods of contraception and correctly fit LARC methods. Furthermore, nurses should suggest a method of contraception that suits a woman’s lifestyle. This may help to achieve perfect use, and ultimately reduce the risk of unwanted pregnancy.
REFERENCES
1. Family Planning Association (FPA). Contraception: Patterns of use factsheet. FPA Factsheet, 2007 https://www.fpa.org.uk/factsheets/contraception-patterns-use
2. Jayatunga W. Contraception: Economic Analysis Estimation of the Return on Investment (ROI) for publicly funded contraception in England. London: PHE publications; 2018
3. Faculty of Sexual and Reproductive Healthcare (FSRH). More than 8 million women of reproductive age are now living in an area where cuts to contraception budgets have taken place. FSRH Press Releases and Statements; 2018 https://www.fsrh.org/news/fsrh-press-statement-more-than-8-million-women-of-reproductive/
4. Wellings K, Jones KG, Mercer CH, et al. The prevalence of unplanned pregnancy and associated factors in Britain; findings from the third National Survey of Sexual Attitudes and Lifestyles (Natsal-3). Lancet;2013;382(9907);1807-1816. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3898922/
5. NICE QS129. Contraception, 2016 https://www.nice.org.uk/guidance/qs129/resources/contraception-pdf-75545366974405
6. Molloy GJ, Graham H, McGuinness H. Adherence to the oral contraceptive pill: A cross-sectional survey of modifiable behavioural determinants. BMC Public Health [Internet]. 2012 Oct [cited 2019 Feb 12];12(838):1-8. Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-12-838
7. NHS. How effective is contraception at preventing pregnancy? NHS, 2017. https://www.nhs.uk/conditions/contraception/how-effective-contraception/
8. Faculty of Sexual and Reproductive Healthcare. Combined Hormonal Contraception, 2019. https://www.fsrh.org/standards-and-guidance/documents/combined-hormonal-contraception/
9. Edelman A, Micks E, Gallo MF, et al. Continuous or extended cycle vs. cyclic use of combined hormonal contraceptives for contraception. Cochrane Database Syst Rev 2014;:CD004695. doi:10.1002/14651858.CD004695.pub3
10. Regional Drug and Therapeutics Centre (RDTC). Cost Comparison Charts [Internet]. Newcastle; RDTC; 2018 [cited 2019 Feb 12]. 75p. Available from http://gmmmg.nhs.uk/docs/cost_comparison_charts.pdf
Related articles
View all Articles