Improving the management of respiratory conditions
DAVE EDWARDS
DAVE EDWARDS
BPharm PGCE DipEd SP IP
Respiratory Pharmacist, South Pembrokeshire Cluster, Hywel Dda University Health Board
Practice Nurse 2022;52(6):10-13
Recent figures show that asthma continues to cause close to 1,500 deaths a year, and the picture for COPD is not much better. But many deaths, attacks and exacerbations are preventable with high quality care: this is how I set about improving my own practice
There are approximately 5.4 million people in the UK living with asthma, which is about 1 in 11 of the population. Asthma is an inflammatory condition that affects the airways causing variable symptoms of cough, wheeze and breathlessness. Asthma often co-exists with other conditions including eczema, allergies and allergic rhinitis. The aim of asthma treatment good control. We define good control of asthma to be no daytime symptoms, no night time symptoms, no limitation on activity and very little need for any rescue medications, including reliever inhalers.1
Recent research by Asthma+Lung UK tells us that someone could be having an asthma attack every 3 seconds, which means 10 million asthma attacks a year, an average of almost two attacks per year per patient with asthma.2 This is higher than previously thought. Every asthma attack is potentially life threatening: there were over 77,000 hospital admissions and 1,484 deaths due to asthma attacks in 2017.3
Chronic Obstructive Pulmonary Disease (COPD) affects an estimated 1.2 million people in the UK,4 and is one of the top three causes of death worldwide. COPD represents an important public health challenge that is both preventable and treatable. Many people suffer from this disease for years before dying prematurely from it or it’s complications.5 COPD is irreversible but patients’ lives can be improved. The aims of treatment are to improve day-to-day symptoms and limit exacerbations which will lead to a greater quality of life.
The Royal College of Physicians (RCP) report, Why asthma still kills: National Review of Asthma Deaths (NRAD), highlighted shortcomings in the management of asthma that contributed to patients’ deaths. These included failures in medical and professional care, prescribing and medicines use as well as patient factors and perception of risk.6 The report made recommendations to improve care, including:
- All asthma patients who have been prescribed 12 or more short-acting reliver inhalers in the previous 12 months should be invited for an urgent review of their asthma control, with the aim of improving their asthma control through education and change of treatment if required
- A more structured asthma review should be developed to improve the documentation in medical notes which will aid the audit of asthma care
- Structured asthma reviews should be undertaken a by a healthcare professional with a specialist training in asthma
- All people with asthma should be provided with written guidance in the form of a personal asthma action plan
- All patients to have inhaler technique checked at regular intervals
- Patient self-management should be encouraged
- Parents and children, and those who care for or teach them, should be educated about managing asthma
Following the report, the national asthma guidelines changed. However, different guidelines give conflicting advice and have the potential to confuse. In Wales, national evidence based All Wales guidelines in Asthma and COPD were developed. In the rest of the UK, NICE and BTS/SIGN have announced that they are making progress towards producing a Joint Guideline for the Diagnosis, Monitoring and Management of Chronic Asthma.
However, data from the National Asthma and COPD Audit Programme (NACAP) and Asthma+Lung UK show that the situation since the NRAD report hasn’t really improved much.3,7 I wondered if I could make a difference.
THE SITUATION LOCALLY
I work for South Pembrokeshire Cluster in Hywel Dda University Health Board in West Wales, and we face similar challenges with respiratory management to other areas of the country. We also have an inspirational, far sighted Respiratory Clinical Nurse Specialist called Debbie Hartman. For years Ms Hartman has been the Lead Respiratory Nurse in Glangwilli Hospital in Carmarthen. She recognised that the standard of respiratory condition management in Primary Care could be improved and that she could help. She arranged a secondment to improve practice, with outstanding results. I spent a few days with her and, with her encouragement and guidance, realised that I could do something similar.
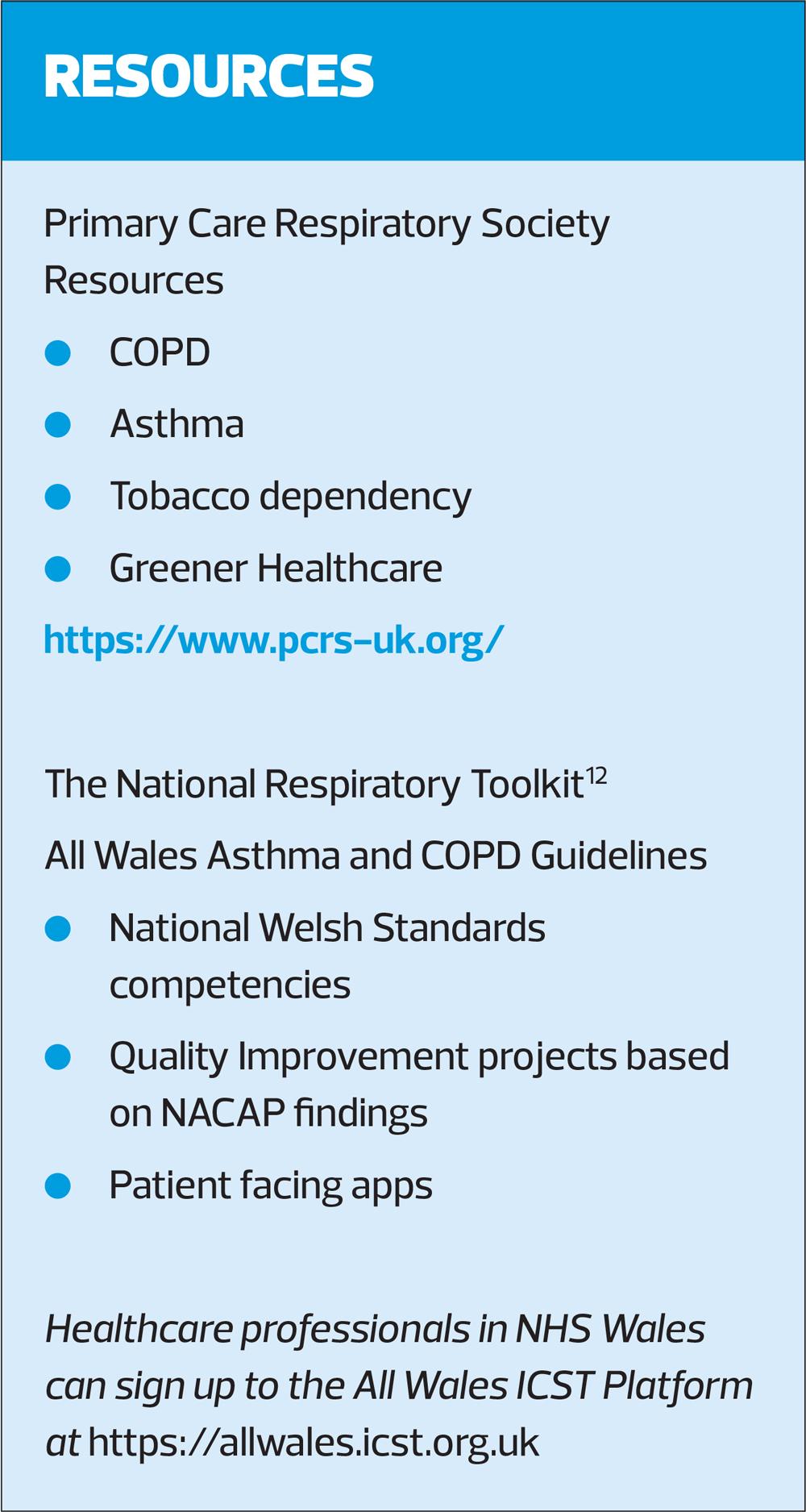
To improve my skills, I attended the Primary Care Respiratory Society Conference and availed myself of the excellent resources on their website. I also used the Welsh ‘National Respiratory Toolkit,’ an integrated system to support NHS Wales to improve respiratory care. It links the All Wales guidelines with a learning package and basic competencies, the National Welsh Standards. It contains Quality Improvement projects so we can all target the things that really matter and links everything with the patient respiratory apps, which help educate and empower patients to manage their condition safely. This toolkit and resources on the PCRS website provided the framework for me to improve the basic management of respiratory care by concentrating on the high value interventions.
OUTLINE
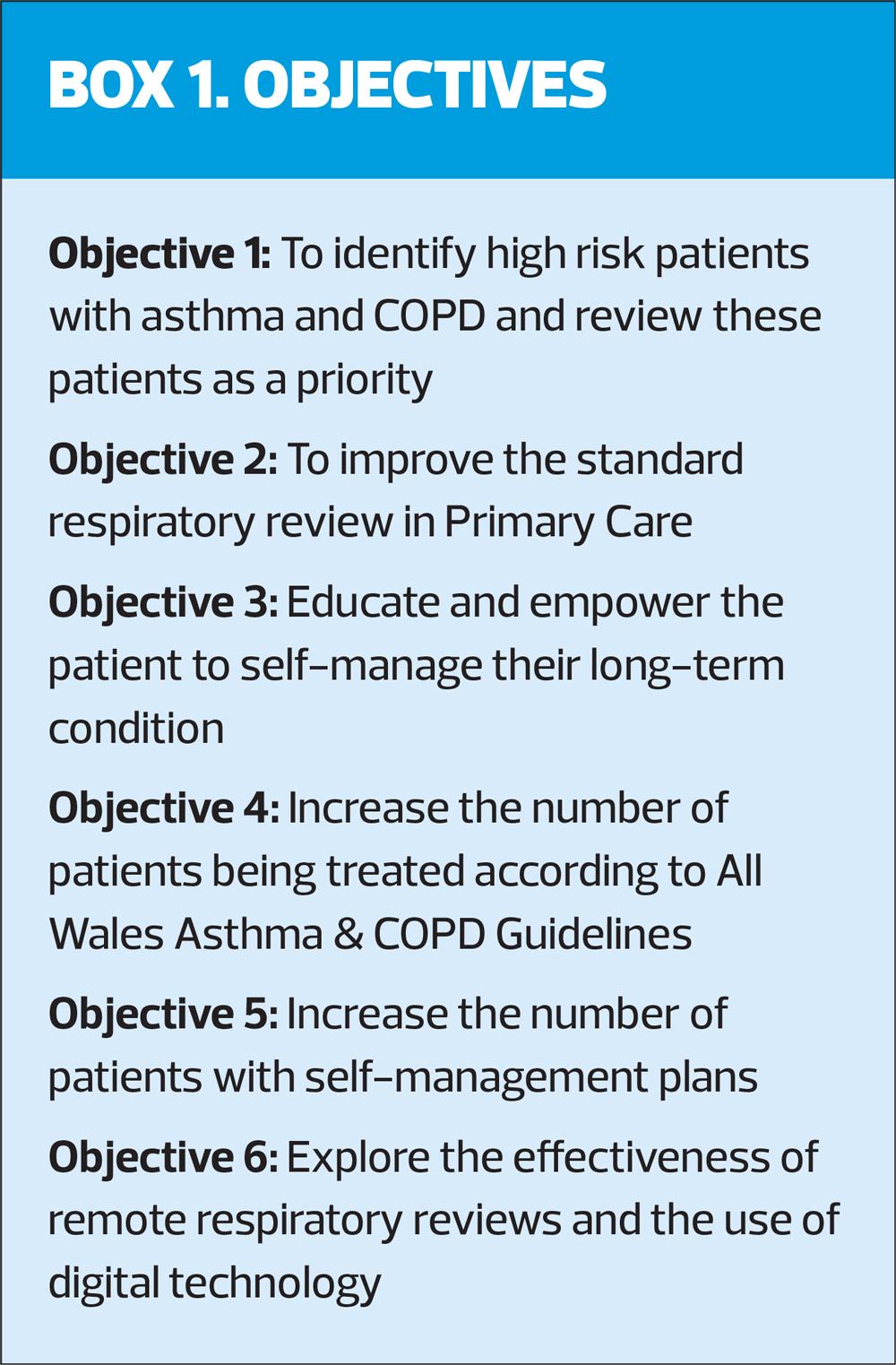
Following Ms Hartman’s lead, my project aimed to show that we can all raise the standard of care in the management of asthma by focusing on doing the basic, but high-value things well. I wanted to move away from the data gathering focus of previous asthma reviews and put the patient at the centre of the consultation. I wanted to educate them about their life-long condition and empower them to self-manage variable symptoms and live well.
The role was to work across four surgeries in South Pembrokeshire cluster.
First, I wanted to identify the patients most at risk and review these patients as a priority.
For asthma, the criteria were:
- Patients issued a high number of reliever inhalers in past 12 month (12 or more initially)
- Patients who had required oral corticosteroids in past 12 months
- Patients who had attended A&E or had been admitted to hospital in past 12 months
- Patients with a diagnosis of asthma not prescribed an inhaled corticosteroid inhaler
For COPD, the criteria were slightly different:
- Patients who continue to smoke
- Patients with a treatment regimen not in All Wales guidelines
- Patients who exacerbate frequently (twice or more in 12 months)
In addition to the above patients I would see any patients referred to me by the GPs or other surgery clinicians.
I also aimed to follow up all patients who had been seen in secondary care respiratory clinics.
Following the NRAD and National Asthma and COPD Audit Programme recommendations, I introduced a more comprehensive review for both asthma and COPD patients. In each review I would look at:
- Confirming the diagnosis with a clear history and objective testing
- Educating the patient about their condition and any associated condition that would empower them to manage their health more safely and effectively
- Optimising both non-pharmacological and pharmacological treatment according to guidelines
- Educating the patient about the action and use of their medication, including inhaler technique
- An explanation of the aims of the treatment and what good control looks like
- Issuing a written worsening symptom management plan and ensuring the patient had the knowledge and understanding to use it
- Improving the documentation in the patient’s notes including diagnostic certainty and treatment rationale.
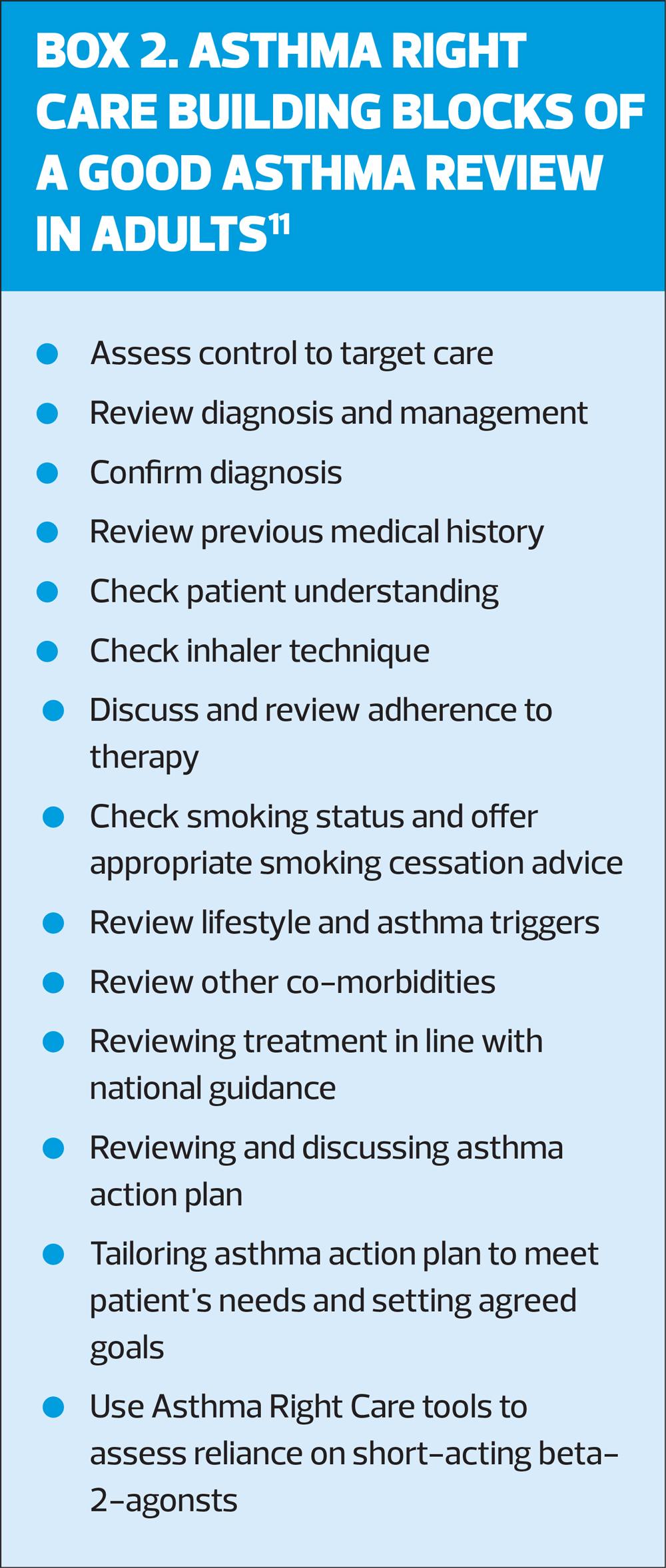
This approach also reflects the Asthma Right Care Building Blocks of a Good Asthma review. See Box 2.
OUTCOMES
As evidence for my outcomes I looked at prescribing data and feedback forms from the patients and from the surgeries.
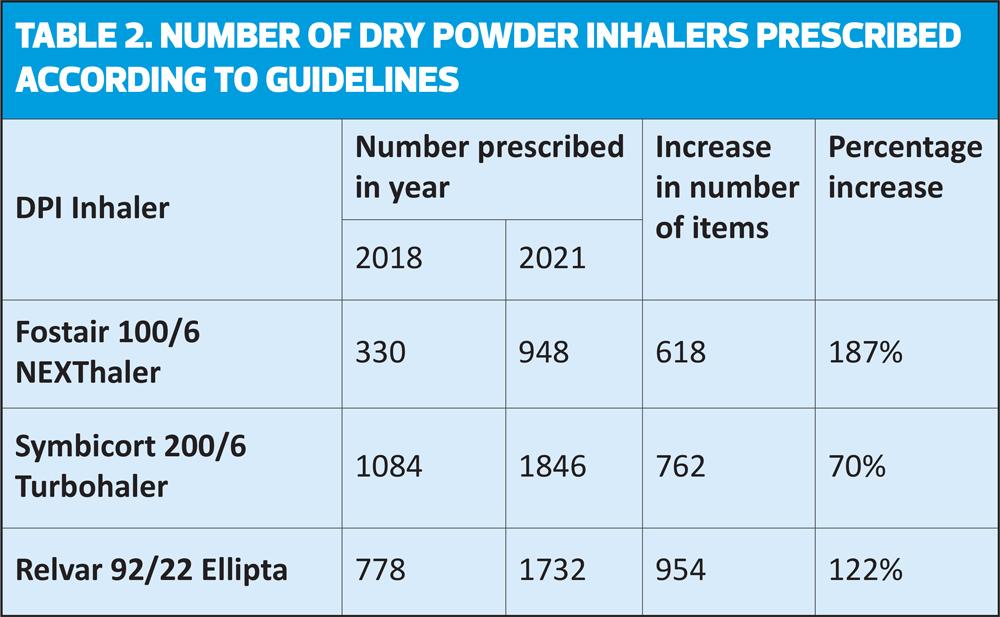
In every consultation, I tried to match the patient to an inhaler regime that they could and would use. All things being equal, my default device was a dry powder inhaler. I was always careful to give the patient a choice of devices and regimes and I explained the pros and cons of each. Every choice for the patient was a trial, not everyone gets on with every inhaler. I followed every patient up at least once to check their understanding of the regime and that they were happy with any changes.
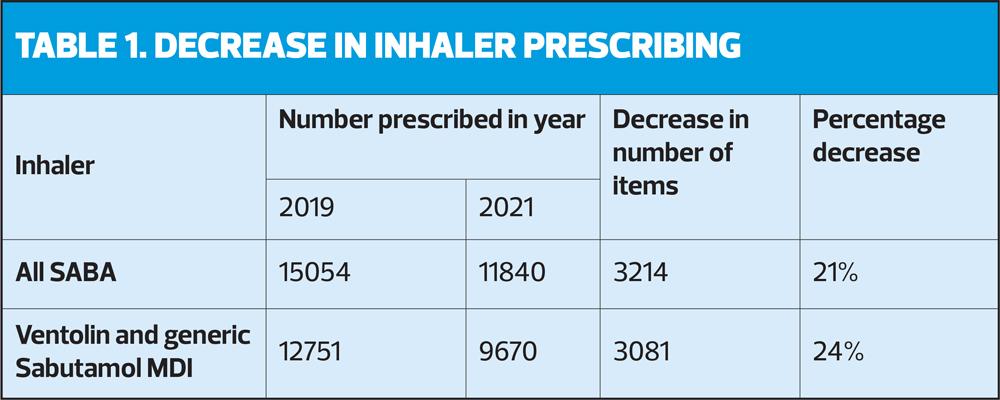
The prescribing data show an increase in prescribing according to guidelines and a significant reduction in SABA usage (Table 1 and 2).
SABA prescribing dropped by over 20% in the two years of the project. The decline was most marked in SABA MDI’s.
There was an increase dry power inhaler prescribing which aligns with the Greener Healthcare agenda. My patients also told me they found these inhalers easier to operate.
There was an increase in inhalers recommended in the All Wales guidelines, so increased prescribing of Fostair and Symbicort as MART regimes, along with a decrease in non-guidelines inhalers, so fewer long acting muscarinic antagonists (LAMA) prescribed as a single agent and a decrease in older combination inhalers.
We know that patients with an asthma or COPD management plan are less likely to require unscheduled care appointments, attend A&E or be admitted to hospital;7,8 the Respiratory Health Implementation Group (RHIG) for Wales also tell us that nearly 50% of the increased hospital admissions during the winter period is due to those with an existing respiratory condition. NRAD identified that only 23% of the patients they reviewed had been issued with an asthma action plan. During my many consultations and conversations with patients not one admitted to having a management plan issued in primary care. I gave every patient either a written management plan, information enabling them to access a digital management plan, or both. I used the Asthma+Lung UK or BLF COPD self-management plan for the paper copies. I used the NHS Wales Asthmahub or COPDHub apps for the digital plans.
There has been an increase in the number of patients referred directly to the smoking cessation and COPD+ services. COPD+ is a service we offer in Hywel Dda as a pre–pulmonary rehab, a ‘pre hab’ if you like. A feature of the COPD+ service is that patients can attend with an MRC of 1 or 2, so before they become too breathless, and an early intervention here could stop or slow down worsening symptoms.
The patient feedback forms told me that the patients benefited from the reviews. Almost all reported improved symptoms and quality of life, more so those with asthma than COPD, all reported a better understanding of their condition, medication and improved confidence in managing worsening symptoms.
The surgeries reported benefits too. I started with my own lists of patients for review, but these were soon added to by the GPs and other clinicians.
I liaised frequently with the respiratory nurse and consultants in secondary care, usually by email. This saved time for me, for secondary care clinics and the patient.
So, from every aspect, this project to improve the management of asthma and COPD in Primary Care can be deemed a success.
- Patients’ lives were improved, their symptoms were reduced and they felt empowered to manage any worsening symptoms.
- The surgeries valued the project and recognised the benefit to their patients and themselves
- The prescribing data shows increased use of guideline-recommended inhalers and less use of reliever medications
CONCLUSION
Nothing I have done is difficult. I followed the example of Ms Hartman’s practice and used available resources. Across the UK we have the PCRS and Asthma Right Care resources which include videos, webinars, posters, slide rules, airway models, and the examples of many GPs, nurses, pharmacists and others who share a common goal, to improve the lives of patients with a respiratory condition. Here in Wales we also have the National Respiratory Toolkit, which provides a dynamic, standardised approach to delivering respiratory services across Wales. See Resources.
My advice to any general practice nurse looking to improve the management of asthma and COPD in their surgery would be to seek out these resources and like-minded individuals, allow them to share their best practice and then implement these in your own consultations.
Steps to improve asthma and COPD care
1. Educate yourself using the resources available through PCRS, Asthma Right Care or the All Wales Institute of Clinical Science and Technology (ICST) platform10-12
2. Draw on the knowledge and advice of your local experts
3. Prioritise your most at risk patents for review
4. Review according to Asthma Right Care/NRAD/NACAP recommendations
5. Educate and empower the patient during the review
6. Treat according to guidelines agreed in your surgery
7. Ensure patients have an inhaler they can and will use
8. Consider the Green Agenda
9. Issue every patient with a worsening symptom self-management plan.
By following simple steps and using the resources available it is possible for all of us to dramatically improve the management of asthma and COPD for our patients.
REFERENCES
1. Asthma UK. https://www.asthma.org.uk/advice/manage-your-asthma/
3. Asthma UK. https://www.asthma.org.uk/about/media/facts-and-statistics/
4. British Lung Foundation. https://statistics.blf.org.uk/copd
5. Global Initiative for Chronic Obstructive Lung Disease (GOLD); Pocket Guide to COPD Diagnosis, Management and Prevention; 2022. https://goldcopd.org/2022-gold-reports-2/
6. Royal College of Physicians. Why asthma still kills: the National Review of Asthma Deaths (NRAD) Confidential Enquiry report. London: RCP; 2014
7. National Asthma and COPD Audit Programme (NACAP). https://www.nacap.org.uk/nacap/welcome.nsf/reportsSC.html
8. NICE QS25. Asthma. https://www.nice.org.uk/guidance/qs25/chapter/quality-statement-2-written-personalised-action-plan
9. NHS Wales, Respiratory Health Implementation Group; The Respiratory Winter Plan, Winter 2019/20
10. Asthma Right Care; The building blocks of a good asthma review in adults; https://www.pcrs-uk.org/resource/good-asthma-review
11. Primary Care Respiratory Society. https://www.pcrs-uk.org/
12. Institute of Clinical Science and Technology. https://allwales.icst.org.uk