QOF: Past headline its sell-by date but lingering
Dr Ed Warren
Dr Ed Warren
FRCGP, FAcadMEd
Despite Government pledges to scrap the Quality and Outcomes Framework, work is underway to develop new indicators for next year’s contract. We look at what is planned and whether the proposals make any clinical sense
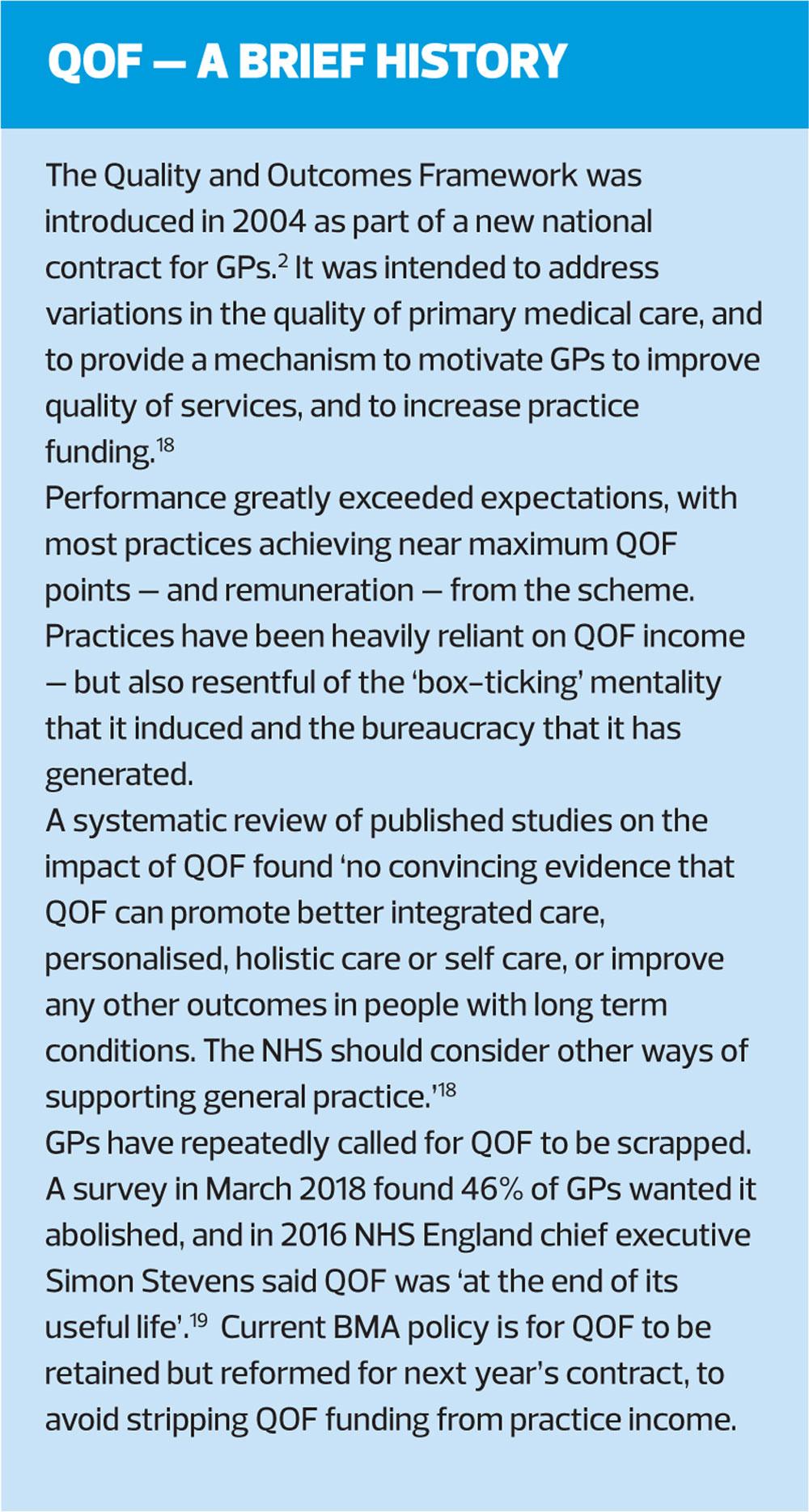
Announcements of the death of the Quality and Outcomes Framework (QOF) have proved premature, at least in England. Scotland has already abolished the QOF. In Wales practices only have to prove that they have registers of patients with specified clinical conditions. In at least one area of England (Leeds) 80% of QOF recording was temporarily suspended in 2017 to cope with winter workload pressures.1 But yet, like the Black Knight from Monty Python and the Holy Grail, the QOF stumbles on sans arms, sans legs, sans credibility.
THE QOF AND NICE
The very first instalment of the QOF in 2004 was, quite frankly, a bit of a dog’s breakfast. It formed part of the New GMS Contract,2 and came together with another book (remember when you got paper to read from?) called Supporting Documentation.3 The Supporting Documentation gave details of the 76 clinical indicators and 70 other indicators which were to be used to quality-control and micromanage general practices. Money was to be taken away from practices, but then the money could be earned back by fulfilling the QOF indicators. So it was financially a high-stakes enterprise for general practice, and yet the Supporting Documentation was very thin on actual support: the evidence given offered little support for the indicators. There were a few references to guidelines and research, but not nearly enough to convince most practitioners that the project had been well thought-through or that the indicators were likely to be at all relevant to improving patient care. There was even less to convince that using the QOF would make the life of general practice any easier, in fact just the reverse.
Cognitive dissonance, doing things that you don’t believe in or you think are inappropriate, is not comfortable, yet general practices were forced to engage with the QOF just to balance the books. The government has had its own guidelines-maker, the National Institute for Health and Care Excellence (NICE) since February 1999, so it made sense to involve NICE in the development of QOF indicators, particularly the clinical ones. This marriage of convenience was consummated in 2009.
It works like this. At least twice a year there is a meeting of NICE’s independent Primary Care QOF Indicator Advisory Committee. This committee currently has 18 members chaired by a Professor of Cardiothoracic Surgery. There are twelve doctors, of whom seven are GPs; two lay members; a practice manager; an Accountable Officer; a Director of Nursing and a GP pharmacist.4 Taking advice from other organisations, the committee’s remit is (among other things) to recommend new QOF indicators. They work to ensure that the recommended indicators are evidence-based, a process that takes about two years.5 The committee’s recommendations are then subject to negotiation between the British Medical Association (BMA) and the Department of Health/NHS Employers. You will notice that no nursing organisations are involved in these negotiations, which I think is a shame.
NEW FOR 2019?
At present the NICE website lists 113 QOF indicator recommendations,6 some of which have already been incorporated into the QOF. A recent report in the GP press7 suggests that for April 2019 nine new indicators are to be put forwards for negotiation: eight to do with diabetes, and one about atrial fibrillation.
NM157*
’The percentage of patients with diabetes without moderate or severe frailty, on the register, in whom the last IFCC-HbA1c is 58 mmol/mol or less in the preceding 12 months’.
The NICE HbA1c default target for adults with type 2 diabetes (T2D) is 48 mmol/mol for those taking medication not associated with hypoglycaemia (such as biguanides, e.g. metformin), and 53 mmol/mol for those taking drugs associated with hypoglycaemia (such as sulfonylureas e.g. gliclazide).8 It is not clear where this alternative figure of 58 mmol/mol comes from (there is no supporting evidence offered), but it represents a relaxation from the rigorous target suggested in the guidance. Even for well controlled T2D patients it would be unusual for successive HbA1c readings to be identical, and some fluctuation is inevitable. So since the proposed QOF indicator specifies that only the last reading should be monitored, then the relaxation give practices some latitude.
The NICE guidelines already say that targets can be relaxed on a case-by-case basis, so that a QOF indicator specifying 58 mmol/mol actually gives less flexibility than the NICE guidance. Another option would have been for a primary care clinician to indicate for each patient what the target HbA1c should be, and use this as the QOF target. But the QOF is as much about controlling primary care as it is about patient quality of life, and presumably such a flexible target would be considered open for ‘gaming’, encouraging practices to set a slack target just to get the QOF points. Heaven forefend that highly trained clinicians and professionals should be left to do their best for their patients without interference. However, the QOF depends on having targets, numbers that can be measured, so it is perhaps understandable that the QOF indicator is framed in the way that it is.
The first item on the management agenda in the NICE Diabetes guidelines is headed ‘Individualised care’,8 and dealing with individual patients is the very stuff of general practice. Not all patients are the same, and do not necessarily behave in the way that the textbooks say they ought to. Many run into problems with their treatment, particularly when this involves changes to lifestyle.
Any target HbA1c is all well and good, but one size does not fit all and for some patients slavish attention to a target will lead to over-treatment: either they will have a problem tolerating the medication, or blood sugars may be rendered sufficiently labile that episodes of hypoglycaemia occur. In diabetes care it is easy to be seduced into thinking that hyperglycaemia is more of a problem, but hyperglycaemia does not make you fall over like hypoglycaemia does.
Patients who have multimorbidity and the inevitable multiple medications that go with this, are particularly vulnerable. Also, patients already dealing with lots of illnesses at once may be nearing the twilight of their years anyway and are unlikely to get much benefit from the longer-term advantages of tight glycaemic control.
NM158
‘The percentage of patients with diabetes with moderate or severe frailty, on the register, in whom the last IFCC-HbA1c is 75 mmol/mol or less in the preceding 12 months.’
Much as you would not wish any T2D patient to fall over because of hypoglycaemia, you would wish a frail patient with T2D to fall over even less. Any fall is likely to be more damaging in the context of pre-existing frailty. A further relaxation of target HbA1c is therefore to be welcomed. Conversely it is of interest that even for a patient with frailty a target minimum HbA1c is not specified: using a range as a target would make more clinical sense.
A target HbA1c of 75 mmol/mol is over half as high again as the NICE default target in the absence of frailty. Having spent years believing that in T2D as far as glucose is concerned, lower is better, this represents a bit of a wake-up. There is no indication as to why the number 75 has been chosen: elevated blood sugars have a linear relationship with conferred risk, so that there are no obvious thresholds.
How do you assess ‘frailty’? The suggested QOF indicators do not give details. Frailty is becoming popular as a diagnosis, and is said to affect 10% of people over 65 and between 25% and 50% of those over 85.9 A diagnosis of frailty is often a bit ‘soft’ as there are invariably multiple causes. Frailty is characterised by a tendency to fall, and by a much-reduced resilience to even minor medical or environmental adverse events. The British Geriatrics Society, in collaboration with the RCGP, has developed guidance entitled ‘Fit for Frailty’, which records seven different tests of frailty.10 Some of these are questionnaires and some are formal mobility tests (walking a set distance, standing from sitting and walking across the room). Probably the two most manageable are:
- Ask your patient: ’How would you rate your health on a score of 0 to 10?’ A score of less than six suggests frailty.
- A GP (or GPN) thinks that the patient is frail.
NM159
‘The percentage of patients with diabetes without moderate or severe frailty, on the register, in whom the last blood pressure reading (measured in the preceding 12 months) is 140/80 mmHg or less’.
According to the NICE guidelines, a blood pressure of 140/80 mmHg is the suggested target for all patients with T2D, and 130/80 mmHg for those with kidney, eye or cerebrovascular damage.8 This means that the QOF indicator and the NICE guidance would suggest an identical target, with no relaxation of the target for the QOF indicator. This is slightly odd as blood pressure is always more labile than blood glucose, in that it can go up and down quickly over the course of seconds. An episode of hypotension is another good way of leaving your patients flat on their faces, and to be avoided. The co-existence of frailty would add to the overall clinical risk and consequences of a fall. It appears that as far as NICE is concerned, in people with T2D, blood pressure control is more important than blood glucose control.
Within the QOF there is a mechanism for ‘exception reporting’, which effectively removes an individual patient from the reckoning when QOF points entitlement is being calculated. I suspect (but I could find no evidence to confirm this assertion) that the most common reason why a patient is excepted is, to use the wording from the GMS contract: ‘Where a patient has not tolerated medication’.11 This could refer either to a specific medication, or where using medication has led to hypotensive episodes.
NM142
‘The percentage of patients with type 1 diabetes who are aged over 40 years currently treated with a statin’.
The NICE guidance on cardiovascular risk12 is quite clear that patients with T1D aged over 40 or who have had T1D for more than 10 years (which is not improbable – T1D often starts in childhood) should be on a statin. Diabetes of any type is a significant risk for cardiovascular disease (CVD), so enthusiastic primary prevention is appropriate. However, not everyone can get on with taking a statin,13 so that a little judicious exception reporting may occasionally be needed. Diabetes as such rarely kills patients. What kills patients is the long-term risks, especially the CVD risk, that having diabetes confers. The diabetes makes your life miserable, but it is the heart attacks that kill you.
NM160
‘The percentage of patients aged 25–84 years, with a diagnosis of type 2 diabetes, without moderate or severe frailty, not currently treated with a statin, who have had a consultation for a cardiovascular risk assessment using a risk assessment tool agreed with the NHS Commissioning Board in the last 3 years’.
For people without diabetes the NICE threshold for assessing CVD risk is age over 40,12 so this indicator is an acknowledgement that patients with T2D are at increased risk of CVD events at a younger age. The inclusion of an upper age limit is not explained. However, few trials have been done on the use of treatment for increased CVD risk in the very elderly, so the use of age 84 may just be a pragmatic recognition of this.
The NICE guidance suggests using QRISK2 as the CVD risk tool of choice in T2D.12 I have no idea whether QRISK2 has been agreed with the NHS Commissioning Board, but it is probably the most widely used CVD risk assessment tool in UK general practice, and indeed is often installed onto practice software. QRISK2 takes diabetes into account when assessing risk.14 There is now also a QRISK3, which may well take over, and presumably this is why the tool has to have been agreed in the last three years. It would be just like the QOF to change the assessment tool with little warning so that practices would either miss their QOF points, or have to work to reset their practice software.
NM161
‘The percentage of patients with a diagnosis of type 2 diabetes and a recorded CVD risk assessment score of ≥10% (without moderate or severe frailty), who are currently treated with a statin (unless there is a contraindication or statin therapy is declined)’.
This is a logical consequence of the previous indicator. Doing a CVD risk assessment it is a waste of time unless you are going to do something useful with the result. Accordingly there will be points on offer both for doing the CVD risk assessment and also for starting the statin.
NM162
‘The percentage of patients with diabetes aged 40 years and over, with no history of CVD and without moderate or severe frailty, who are currently treated with a statin (excluding patients with type 2 diabetes and a CVD risk score of <10% recorded in the preceding 3 years)’.
This is a follow-on from NM160, but just worded in a different way to confuse us. I think this means that patients with T2D and a low QRISK2 score do not need to take a statin, but those with a risk of over 10% over 10 years do need to take a statin. Work may need to be done on the wording to stop GPNs and GPs getting a headache.
NM163
‘The percentage of patients with diabetes and a history of CVD (excluding haemorrhagic stroke) who are currently treated with a statin’.
It is not clear what this indicator is trying to achieve. For patients who have proven CVD you move from a primary prevention to a secondary prevention situation. Taking a statin is a good idea irrespective of any diabetes. Haemorrhagic stroke is more closely related to blood pressure than to assessed CVD risk.
NM164
‘The contractor establishes and maintains a register of patients with atrial fibrillation, including patients with ‘AF resolved’.
The ‘contractor’ is presumably the practice. You would have thought, once their atrial fibrillation (AF) had gone away, that the risk of a patient having a stroke would go back to normal. A recent paper in the BMJ confirmed that this is not the case.15 Patients with ‘AF resolved’ are certainly less likely to have a stroke than people with current AF, but the risk is not completely abolished – hence the need to keep track of your patients who have had AF in the past.
CONCLUSION
Dear old NICE is still plugging away, trying to make the QOF more acceptable to the scientifically minded, despite the evidence that even into its 15th year it has not made a lot of difference.16 The QOF is getting smaller rather than larger, and certainly is less important to practice finances than it used to be.
In July 2018 it was reported that there are other plans for the QOF. The headline message was that up to a quarter of the indicators could be retired.17 This sounds wonderful until you recall that when indicators have been retired in the past there remained an expectation that the targets would continue to be achieved, but without the resources to do the work. Other changes are also in the pipeline. Exception reporting is to be updated.17 The indicators discussed above may well be incorporated. The wording of some existing indicators could be altered, which could well cause as much disruption and work as introducing the new indicators.
The QOF may be mortally wounded but it refuses to lie down.
*NICE descriptor and not the number of the indicator if it is incorporated into the QOF
REFERENCES
1. Bostock N. QOF suspended across Leeds to ease 'incredible strain' on GP practices. https://www.gponline.com/qof-suspended-across-leeds-ease-incredible-strain-gp-practices/article/1422925
2. The NHS Confederation. BMA. New GMS Contract. May 2003
3. The NHS Confederation. BMA. New GMS Contract. Supporting documentation. May 2003.
4. NICE. Indicator Advisory Committee members https://www.nice.org.uk/get-involved/meetings-in-public/indicator-advisory-committee-iac/iac-members
5. Stokes T, Bent N. NICE-led QOF process will help to deliver improved indicators https://www.guidelinesinpractice.co.uk/nice-led-qof-process-will-help-to-deliver-improved-indicators/312287.article
6. NICE Quality and Outcome Framework indicator. https://www.nice.org.uk/standards-and-indicators/qofindicators
7. Anon. NICE backs new QOF targets to deliver 'personalised care' for diabetes https://www.gponline.com/nice-backs-new-qof-targets-deliver-personalised-care-diabetes/article/1496429
8. NICE NG28. Type 2 diabetes in adults: management https://www.nice.org.uk/guidance/ng28/chapter/1-Recommendations#hba1c-measurement-and-targets
9. Kernick D, Chew-Graham CA & O’Flynn N. Clinical assessment and management of multimorbidity. Br J Gen Pract May 2017;67:235-6.
10. BGS. Recognising frailty. https://www.bgs.org.uk/resources/recognising-frailty
11. 2018/19 General Medical Services (GMS) contract Quality and Outcomes Framework (QOF) Guidance for GMS contract 2018/19 April 2018 http://www.nhsemployers.org/-/media/Employers/Documents/Primary-care-contracts/QOF/2018-19/2018-19-QOF-guidance-for-stakeholders.PDF
12. NICE. Cardiovascular disease: risk assessment and reduction, including lipid modification https://www.nice.org.uk/guidance/cg181/chapter/1-recommendations#lipid-modification-therapy-for-the-primary-and-secondary-prevention-of-cvd-2
13. Warren E. Prescribing lipid-lowering drugs. Practice Nurse 2018;48(9):22-25.
14. ClinRisk. The QRISK®2-2017 cardiovascular disease risk calculator https://qrisk.org/2017/
15. Adderley NJ, Nirantharakumar K & Marshall T. Risk of stroke and transient ischaemic attack in patients with a diagnosis of resolved atrial fibrillation: retrospective cohort studies BMJ 2018;361:k1717
16. NHS. Report of the Review of the Quality and Outcomes Framework in England. https://www.england.nhs.uk/wp-content/uploads/2018/07/quality-outcome-framework-report-of-the-review.pdf pp25-28
17. Bostock N. QOF overhaul could see quarter of indicators scrapped. https://www.gponline.com/qof-overhaul-quarter-indicators-scrapped/article/1486950
18. Forbes LJL, Marchand C, Doran T, Peckham S. The role of the Quality and Outcomes Framework in the care of long term conditions: a systematic review. Br J Gen Pract 2017;67(664):e775-784
19. Mahase E. Nearly half of GPs think it is time to get rid of the QOF. Pulse, 6 March 2018. http://www.pulsetoday.co.uk/your-practice/qof/nearly-half-of-gps-think-it-is-time-to-get-rid-of-the-qof/20036142.article
Related articles
View all Articles