Greener practice in primary care nursing
Dr Honey Smith
Dr Honey Smith
BMedSci, BM,BS, MRCGP, DFSRH, PGAMedEd
General Practitioner,
Richmond Medical Centre, Sheffield
Director, Greener Practice CIC
Alison Robson
RGN,MSc ,OStJ
Advanced Nurse Practitioner,
Eric Moore Partnership Warrington
Practice Nurse 2024;54(6):12-15
As primary care clinicians we have an important role in reducing our carbon impact and other environmental damage, and the climate emergency means there is no time to waste in achieving environmentally sustainable clinical practice
The Climate and Ecological Emergency (CEE) is a health emergency, encompassing all the health effects of global overheating, biodiversity loss, ocean and water harms, air pollution and land misuse. The NHS contributes 4-5% of the UK’s carbon emissions.2 Of this, 23% is attributable to primary care,3 and 60% of this 23% is due to clinical activity. As primary care clinicians we have an important role in reducing our carbon impact and other environmental damages which often operate in tandem. The NHS has committed to ‘net zero’ direct carbon emissions by 2040 and indirect (supply chain) emissions by 2045, and there is no time to waste in achieving environmentally sustainable clinical practice.2
The good news is that the vast majority of the actions we can take for planetary benefit have massive co-benefits for patients, and often also save money for the NHS and beyond.
Greener Practice Community Interest Company (CIC) is a primary care network and virtual hub, set up in 2017, to support and enable primary care action on the CEE, and to share our understanding of these win-win solutions. Our website offers information and ideas to support sustainable quality improvement activity.4 We have an extremely active and supportive network of over 30 groups across the country and eight national WhatsApp groups, where ideas and initiatives are enthusiastically shared. We have achieved considerable expertise in primary care actions to improve our environmental impact. The principles of sustainable clinical practice are:
1. Disease/morbidity prevention and health promotion/creation
2. Patient empowerment
3. Lean pathways (prevention of duplicate/unnecessary activity)
4. Low carbon alternatives
General practice nurses (GPNs) are well placed to play a key role in many of these areas. Here are some suggestions of actions for maximum impact.
CONSULTATIONS WITH PATIENTS
GPNs perform the majority of chronic disease management (CDM) reviews, and have a key role in patient empowerment, morbidity prevention and health promotion. Arranging CDM reviews together, so that patients make one journey to the surgery, reduces patient travel and can encourage a holistic approach to comorbidities. Make every conversation count, and consider integrating sustainability into all reviews.
Lifestyle Advice
Nurses are well versed in offering lifestyle advice, such as encouraging exercise, healthy eating and smoking cessation. Baby checks or immunisation clinics can be a good time to talk about reusable nappies and wipes. Depression reviews could signpost patients to therapies such as outdoor activity or gardening. Exercise in nature offers additional benefits over other forms of exercise, and there are huge financial benefits to the NHS and the UK from a Natural Health Service.11 Advice on healthy eating could include information on the benefits of a plant-forward, whole food diet low in ultra-processed foods (UPF), benefitting cardiovascular and bowel health. NICE guidance supports offering advice on air pollution during asthma consultations. Air pollution is implicated in heart disease, COPD, strokes, dementia, poor pregnancy outcomes, childhood obesity, and child brain, vascular and lung development, so advice on air pollution reduction (e.g. by active travel, and reducing indoor air pollution) could be incorporated routinely into consultations, while acknowledging that some air pollution exposure is sadly unavoidable. Here, as health professionals, we can be effective campaigners for active travel infrastructure and for clean energy to improve public health.
Asthma
Asthma is a key focus in sustainability work. It is estimated that 13% of the NHS’s direct carbon emissions comes from pressurised metered dose inhalers (pMDIs) alone.12 In addition, poorly controlled asthma has a high patient and planetary cost due to hospital admissions, extra appointments and rescue medications. Compared with the rest of Europe, the UK has particularly poor outcomes for asthma.13 A focus on ensuring that asthma patients get the right medicine to the right place in their airways will improve asthma outcomes as well as reduce the carbon footprint from pMDIs.
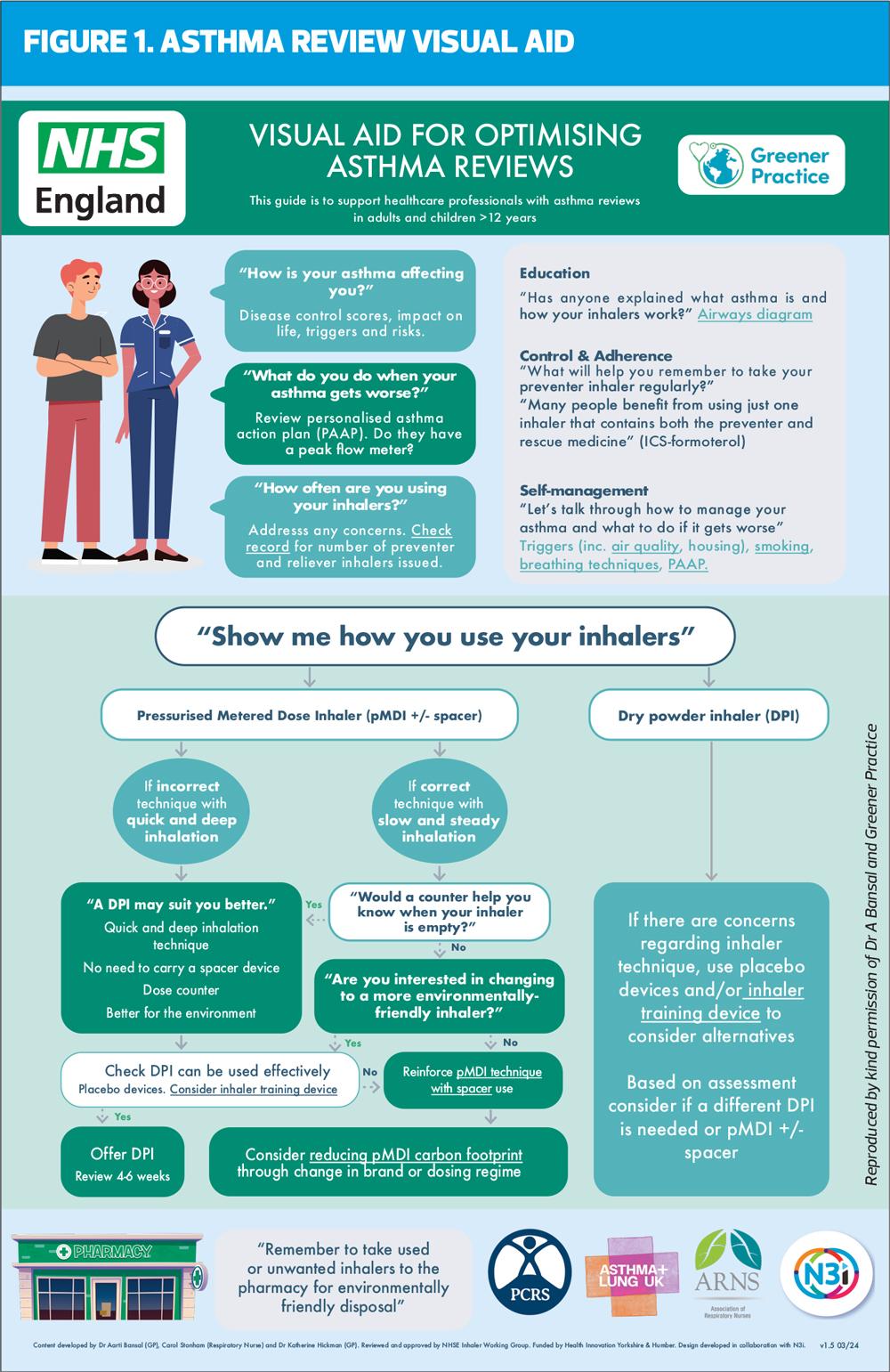
Bansal et al’s article on the asthma consultation gives an excellent overview of key areas for focus,14 and the Greener Practice website has step-by-step resources in our asthma quality improvement toolkit, including an Asthma Review visual aid (see Figure 1) to support patient education and good conversations about inhalers, also available at https://www.greenerpractice.co.uk/wp-content/uploads/Asthma-Visual-Guide-V1.5.2.pdf.
The key messages in the management of established asthma are:
- Prioritise addressing short acting beta agonist (SABA) over-reliance and over-ordering
- Use airways diagrams to explain underlying airway inflammation and how inhalers work
- Consider using combination ICS/formoterol Maintenance and Reliever Therapy (MART) and Anti-Inflammatory Reliever (AIR) regimes. These have been shown to reduce the risk of asthma attacks, are often easier for patients to understand and use, and usually obviate the need for SABA rescue medication.15
- Ask patients to demonstrate their inhaler technique and match the inhaler to the patient’s technique and needs. For adolescents and adults this often means a dry powder inhaler (see Figure 1).
- Use dry powder inhalers (DPIs) first line where clinically appropriate (many areas, such as Sheffield, now have excellent guidelines15 where these are first line)
- Educate patients to return all unused or empty inhalers to the pharmacy for safe disposal and possible recycling.
Frailty
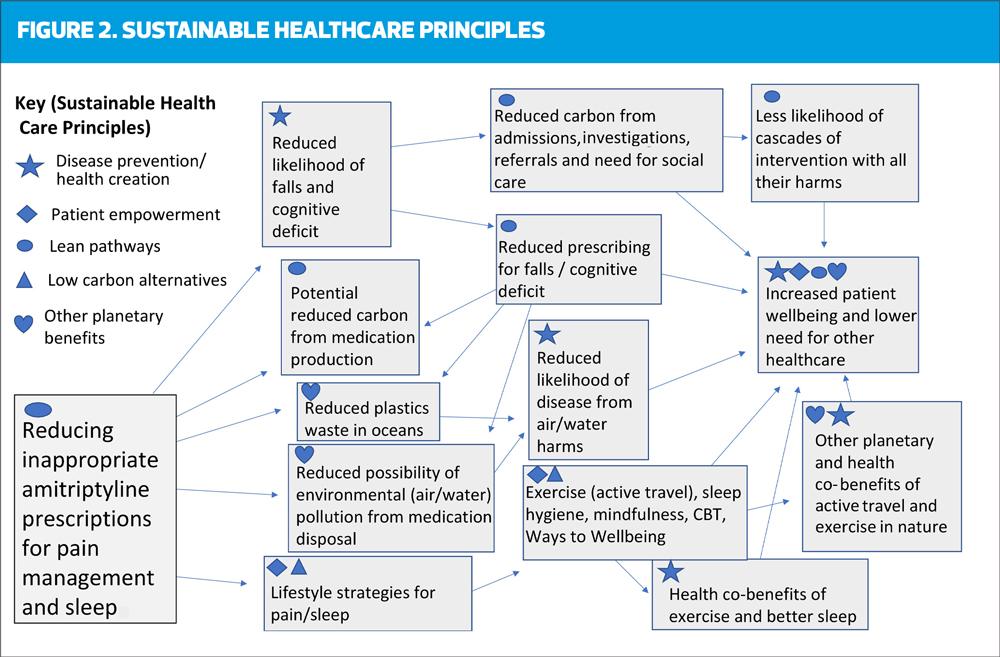
Nurses are ideally positioned to notice and address increasing frailty; a simple quantifying tool is the Rockwood Frailty Score.5 Scores of 5+ could prompt reconsideration of the appropriateness of prescribing, and of strict adherence to guidelines that were designed for people who do not live with frailty. Blood pressure naturally drops in the last 10-15 years of life;6 tight hypertension control and polypharmacy in older people living with frailty increases the risk of postural hypotension and falls. The benefit risk ratio of statins in the over 85s is unclear,7 unless there has been a recent cardiac event. Tight glycaemic control in older patients may be disadvantageous.8 Anticholinergic burden (ACB) scoring9 (Figure 2) helps address significant potential harm to patients, and highlighting this to clinical pharmacists or doctors focusses minds on ACB reduction with huge benefits to patients and planet.10
Contraception
Contraception and sexual health conversations could include discussions about sustainable period products and long-acting contraception. For patients on injectable contraception, self-injectable products are convenient and reduce the need for appointments and patient travel.
Diabetes
Patients starting insulin in primary care should be considered for a reusable pen device as first line, and choice of blood glucose testing device might be influenced by recycling schemes at disposal.
REDUCE, REUSE (RECYCLE)
Most health professionals abhor waste, and we at Greener Practice have found reduction in health care waste to be a shared aspiration across the wider health care community, and an important morale-boosting activity for those teams that do it.
Reduce
Consider whether couch roll is necessary for all examinations. Couch roll only needs to be under (and over, for intimate examinations) the exposed body part rather than over the whole couch. Glove use reduction campaigns have been highly successful at Great Ormond Street Hospital,16 where improved primacy of good hand washing reduced infection rates. Consider whether gloves are needed unless for intimate examinations or where there is a significant risk of body fluid contact, following the aphorism ‘If it’s wet and sticky and not yours, wear gloves!’17 The use of gloves for venepuncture has crept in without adequate evidence of their usefulness; the current thinking in many Infection Prevention and Control (IPC) teams is that experienced practitioners can risk assess for themselves whether gloves are of benefit.18 The risk of blood contact is small and glove use may increase the likelihood of failed procedures, while doing nothing to reduce the risk of needlestick injury.
Reuse
The NHS is tremendously wasteful in its use of single use instruments and equipment. We must reverse this trend if the NHS is to reach its net zero commitments. Reusable, wipeable tourniquets are now widely available and represent a real advance in reducing plastic waste. In some areas, sterilisation services may be available allowing for the use of reusable metal speculums (well tolerated by patients if warmed first).19
Recycle
Recycling is a tiny part of the solution to the CEE – recyclable materials contribute a very small percentage to the carbon emissions of health care – but for some people, it can be the starting point of action. Unfortunately, the cost of domestic recycling for small businesses can act as a disincentive to this activity.
WASTE
Segregation of clinical waste is a key area of focus. Waste disposal of orange bags (clinical infectious) has double the carbon impact of that of tiger bag (clinical offensive) waste and both have a higher impact than black bag (domestic) waste.20 Strict adherence to appropriate segregation, with labelling of bins and the potential for auditing of bin usage, decreases the carbon impact of waste substantially, and for some practices will save money too. Tiger bags should now be available to all practices, so if you do not yet have tiger bags/bins ask your practice manager to contact your waste management services. Nurses’ rooms need orange, tiger and black bins, whereas doctors’ rooms probably only need tiger and black bins. Hormone products (e.g. removed hormonal intrauterine devices and implants) should be disposed of in purple topped sharps bins to avoid hormonal environmental harms.
Encourage patients to return all unused and unwanted medication to the pharmacy for safe disposal, because significant water harms are caused by medications placed in domestic waste or flushed down toilets.21 It is particularly important that inhalers are returned to community pharmacists, either for recycling if a scheme is available locally, or for incineration, to reduce the ongoing impact of the greenhouse gases in pMDIs. The Greener Practice website has a medicines wastage video which practices can add to their waiting room loop.
TEAMWORK AND COMMUNICATION
One of the most effective actions that healthcare professionals can take is to talk about the CEE. The more the crisis is in peoples’ consciousness, particularly if they understand the co-benefits of action and the hopeful narrative that emerges, the more likely teams are to come on board with a shared approach, which is key to success.
Leading by example is a powerful way to influence others without lecturing! Colleagues may notice your own activities to reduce your own carbon footprint, such as active or lower carbon travel to work, and reducing your meat and dairy intake. Talk positively and creatively about the many co-benefits of waste reduction, active travel, health promotion and creation and holistic care. Create an environment where colleagues can enjoy learning together – for example a shared plant-based ‘lunch and learn’ with a clinical learning event incorporating sustainability thinking into the learning. Celebrate your own and your team’s planetary health successes, however small, and suggest the formation of a practice or PCN Green Team.
Encourage trainees and other team members doing clinical or non-clinical quality improvement (QI) work to consider its sustainability aspects. This supports environmentally aware behaviour, increases understanding and may influence future practice. The RCGP’s Green Impact for Health (GIfH) Toolkit22 has many useful actions, and in addition Greener Practice is about to launch a Sustainable QI platform providing easily replicable clinical projects. Reviewing the green impact toolkit and Greener Practice platform as a team can identify areas particularly pertinent to your patient population. For example, a practice with a high percentage of older patients may benefit from focussing on reducing polypharmacy, or an area with a high social deprivation index may wish to prioritise action on fuel poverty.
COMMUNICATION WITH PATIENTS
Use your practice’s social platforms, such as texts, or messages on prescriptions, to communicate both generally, and also with specific patients about, for example, inhaler technique videos, personalised asthma action plans, sick day rules etc. Many clinical template systems include prompts to convey key messages for climate such as air quality discussions.
JOIN GREENER PRACTICE!
Greener Practice welcomes primary care nurses into our community. The network offers support, encouragement and resources, and can suggest actions to aid you on your journey towards environmentally sustainable primary care. Local groups around the country are powerfully supportive, and if you don’t have a group in your area, we are happy to put you in touch with other like-minded practitioners locally who might wish to form a group. Please email contact@greenerpractice.com to join our network, or contact your local group via our website https://www.greenerpractice.co.uk/join-our-network/local-groups/. If you create a formal group, let us know! You will have your own webpage, and chairs of local groups are invited to quarterly National Leads’ meetings and annual or biennial national social events, to connect with other leaders and feel mutually supported by an enthusiastic and hugely encouraging community.
REFERENCES
1. Romanello M, di Napoli C, Green C, et al. The 2023 report of the Lancet Countdown on health and climate change: the imperative for a health-centred response in a world facing irreversible harms. Lancet 2023; 402(10419): 2346–2394
2. NHS England. Delivering a Net Zero National Health Service; 2022. https://www.england.nhs.uk/greenernhs/a-net-zero-nhs/#:~:text=The%20report%20examines%20a%
20number%20of%20the%20areas%20critical%20to
3. Tennison I, Roschnik S, Ashby B, et al. Health care's response to climate change: a carbon footprint assessment of the NHS in England. Lancet Planetary Health 2021; 5(2):e84–e92 DOI: 10.1016/S2542-5196(20)30271-0
4. Greener Practice. https://www.greenerpractice.co.uk/
5. Rockwood Clinical Frailty Scale. https://www.england.nhs.uk/south/wp-content/uploads/sites/6/2022/02/
rockwood-frailty-scale_.pdf
6. Delgado J, Bowman K, Ble A. et al. Blood Pressure Trajectories in the 20 Years Before Death. JAMA Intern Med 2018;178(1):93-99. doi: 10.1001/jamainternmed.2017.7023. PMID: 29204655; PMCID: PMC5833502.
7. Cobos-Palacios L, Sanz-Cánovas J, Muñoz-Ubeda M, et al. Statin Therapy in Very Old Patients: Lights and Shadows. Front Cardiovasc Med. 2021;8:779044. doi: 10.3389/fcvm.2021.779044. PMID: 34912868; PMCID: PMC8667269.
8. Lehman R, Krumholz H M. Tight control of blood glucose in long standing type 2 diabetes BMJ 2009;338:b800 doi:10.1136/bmj.b800
9. ACB Calculator https://www.acbcalc.com/#:~:text=A%20
tool%20for%20finding%20the%20ACB%20Score%20of%20commonly%20prescribed
10. Smith H, Fligelstone H. Reducing patient and planetary harms from high anticholinergic burden medication. BMJ 2024; 384 :e075708 doi:10.1136/bmj-2023-075708
11. The Wildlife Trusts. A Natural Health Service: Improving Lives and Saving Money. Press release; 2023. https://www.ricardo.com/media/23ll4c2g/a-natural-health-service-press-release-final.pdf
12. Fidler L, Green S, Wintemute K. Pressurized metered-dose inhalers and their impact on climate change. CMAJ. 2022 Mar 28;194(12):E460. doi: 10.1503/cmaj.211747. PMID: 35347049; PMCID: PMC8967439.
13. Global Asthma Network. The Global Asthma Report 2022 https://globalasthmareport.org/data/Ch4Fig1.php?view=full
14. Bansal A, Franklin L, Twohig H. Optimising inhaled therapy for patients with asthma BMJ 2024; 386 :e080353 doi:10.1136/bmj-2024-080353
15. Leese D. Sheffield asthma guidelines; 2023 https://www.sheffieldccgportal.co.uk/clinical-guidance/asthma-guidelines
16. NHS England. The Atlas of Shared Learning Case Study; 2018. https://www.england.nhs.uk/atlas_case_study/the-gloves-are-off-campaign/
17. Isherwood, T. Personal communication, quoting Jon Otter (Director of Infection Prevention and Control, Guy's and St.Thomas' NHS Foundation Trust)
18. Isherwood, T. Personal communication
19. Drayton R, Smith H, Ratnappuli A. Sustainable practice: Switching to reusable vaginal speculums BMJ 2023; 383 :e075779 doi:10.1136/bmj-2023-075779
20. Rizan C, Bhutta M, Reed M, et al. The carbon footprint of waste in a UK hospital. J Clean Prod 2021;286:125446: https://doi.org/10.1016/j.jclepro.2020.125446
21. Pfleger, S. Personal communication. See Sharon Pfleger’s webinar for Greener Practice. https://www.greenerpractice.co.uk/information-and-resources/events-webinars/past-webinars/sharon-pfleger-medicines-and-the-environment-25-05-22/
22. RCGP Green Impact for Health Toolkit https://toolkit.sos-uk.org/greenimpact/giforhealth/login
Related articles
View all Articles