Tackling chronic opioid use
Katherine Ellerby
Katherine Ellerby
RGN, RM, BSc (Hons),
Non-medical independent prescriber, NDFSRH
Practice Nurse, Framlingham Medical Practice, Suffolk & Clinical Research Nurse, Suffolk Primary Care
While not at the scale seen in the US, there is evidence of a significant increase in opioid prescribing in general practice, alongside increases in opioid drug-related deaths. It is therefore good practice to review patients who may be candidates for opioid-use reduction interventions and to support those undergoing dose tapering
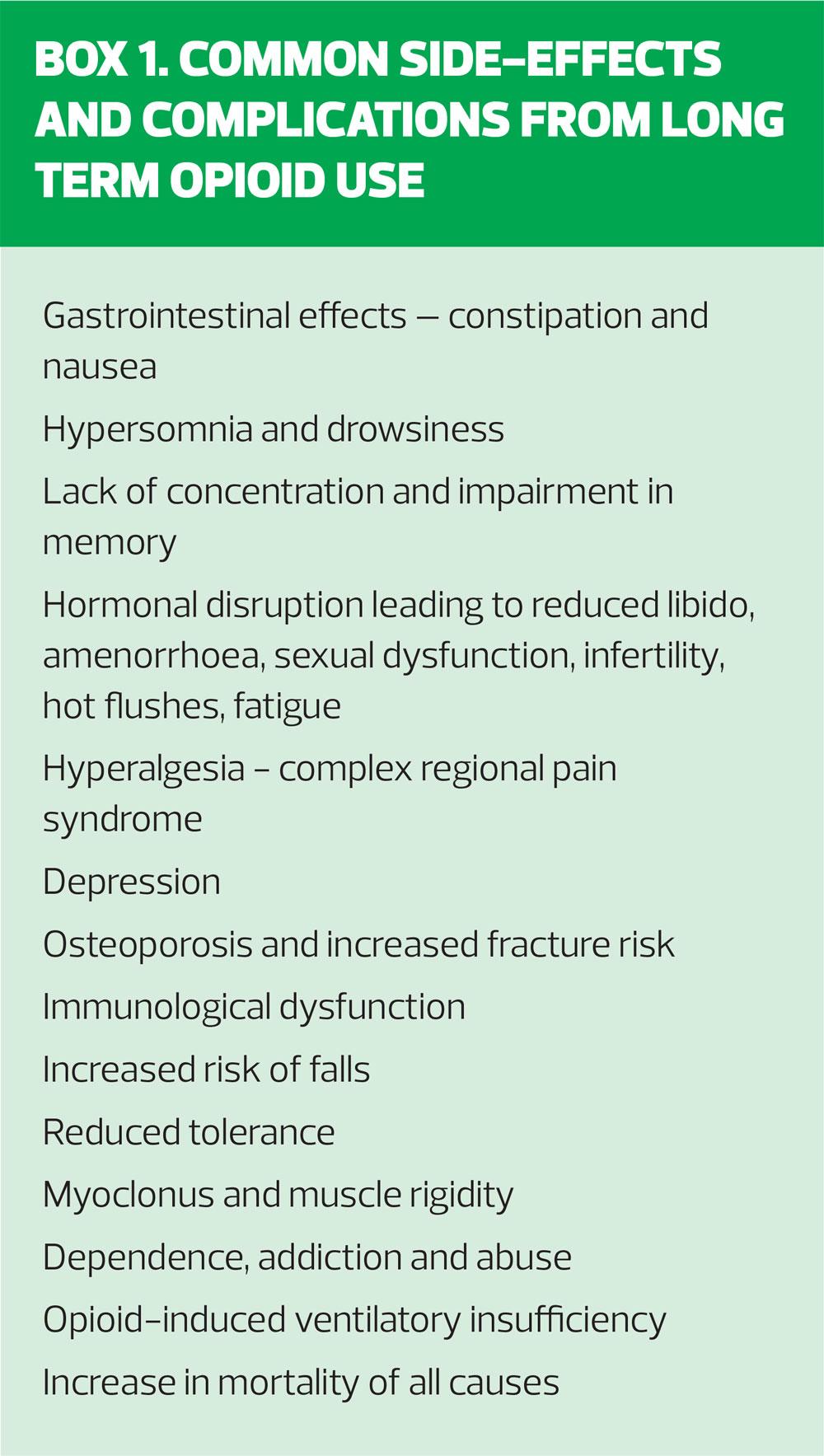
Opioid analgesics for non-cancer pain are frequently prescribed in primary care but there are increasing concerns about overuse and over-reliance on opioids – especially in light of substantial evidence demonstrating a lack of long term benefit.1 Not only that, patients are being burdened with a range of harmful and potentially serious side effects, including the risks of addiction and dependence. In truth, only around 20% of people taking long term opioids actually experience a reduction of pain, which means that nearly 80% are taking these drugs and getting no analgesic benefit but still experiencing adverse effects (Box 1).2
THE FACTS
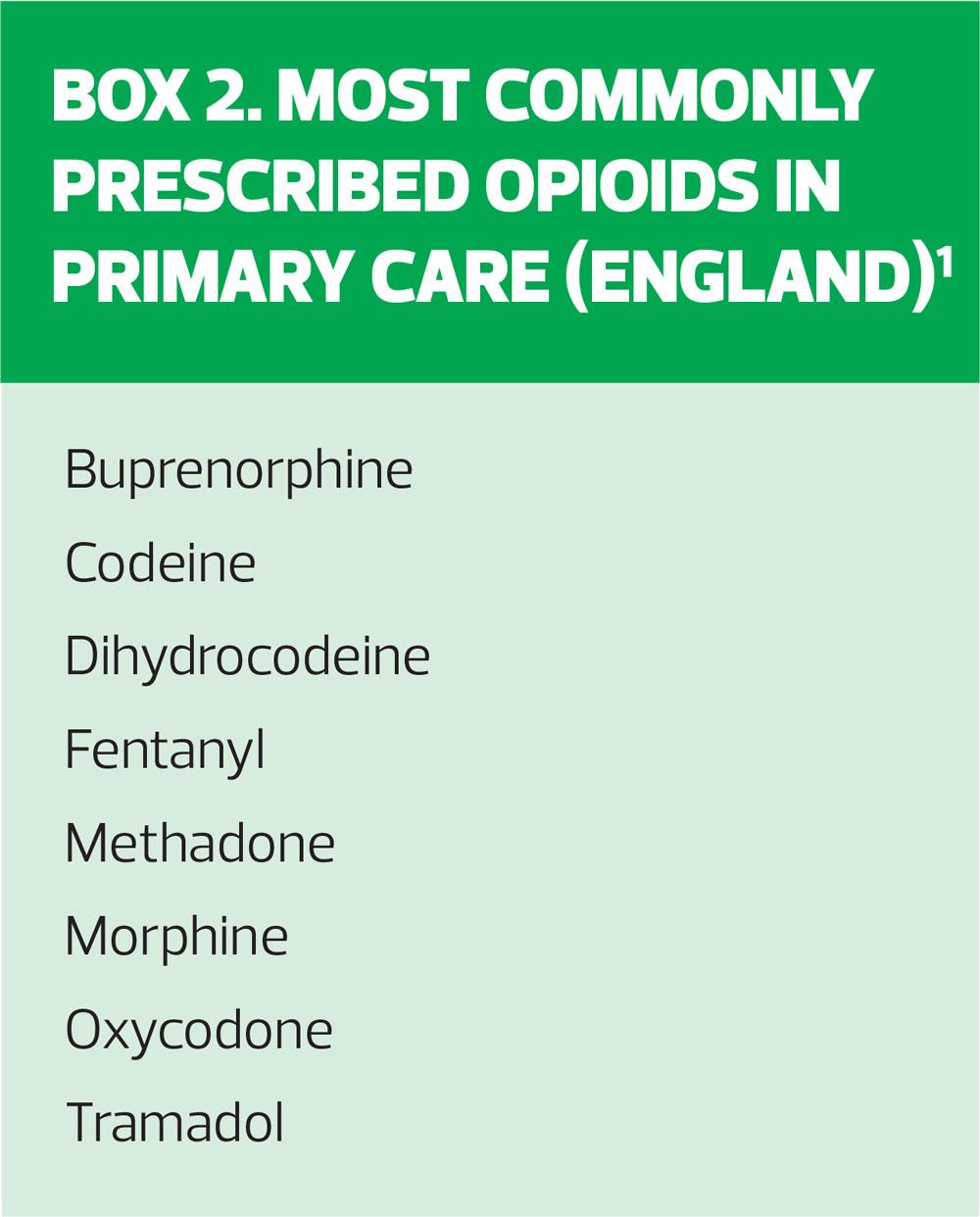
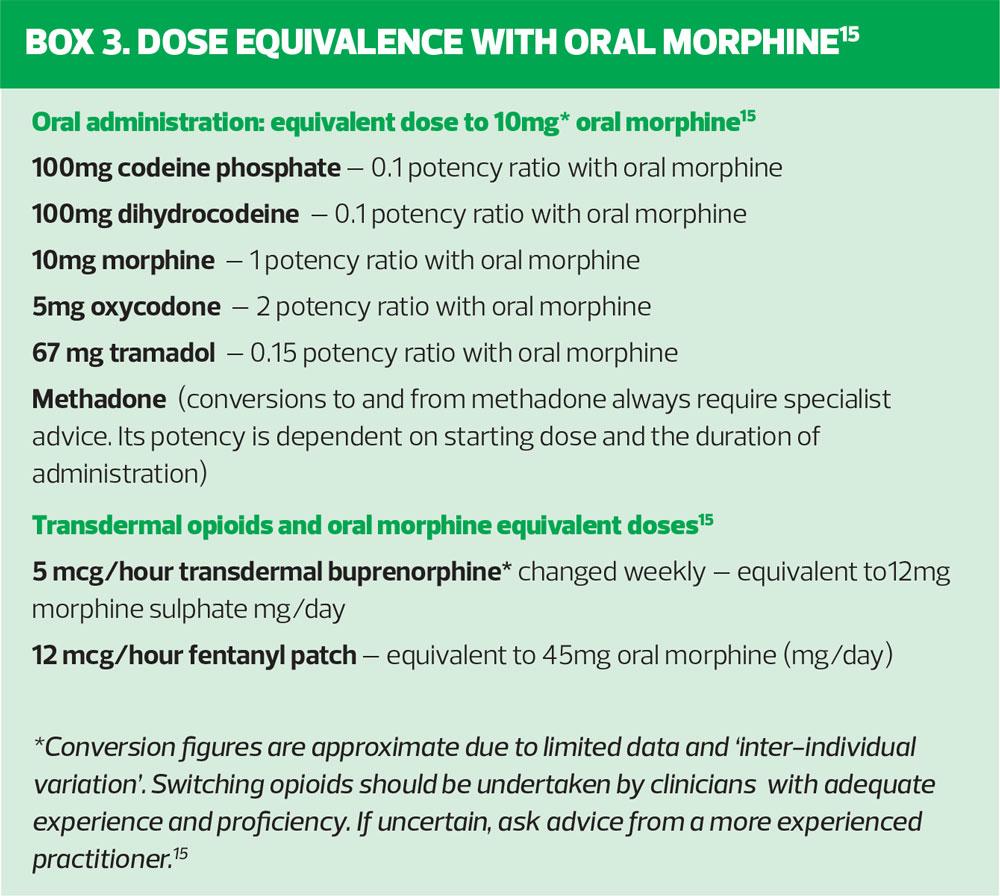
The significant increase in opioid prescriptions and the number of deaths attributed to their use make grim reading. There is huge variation – up to four times – in opioid prescribing in primary care, with higher rates in parts of the north west and north east of England compared with lower rates of prescribing by GP practices in the south, together with clear evidence of greater opioid use in areas of social deprivation where there are also higher rates of obesity, smoking and depression.3 We also know that patients of lower socio-economic status are more likely to experience chronic pain.2 The bare facts are that in England and Wales, the number of prescriptions for opioIds has increased over a 10-year period from 14 million in 2008 to 23 million in 2018 – more than a 60% increase.4 Deaths attributed to opioids have also risen: between 2001 and 2011, deaths in England, Scotland and Wales increased from 500 to almost 900.2 Box 2 identifies the eight most frequently prescribed opioids in England, and dose equivalence to oral morphine is shown in Box 3. Mortality from tramadol, in particular, is increasing with latest figures suggesting it causes 240 deaths a year in England and Wales.5 Clearly the overuse of opioids for non-cancer pain is a public health issue.
TOOLKIT TO TAPER OPIOID USE
Researchers from the University of East Anglia (UEA) have shared an evidence-based approach to tackling the issue of chronic opioid use for non-cancer pain.6 The Toolkit for Tackling Chronic Opioid Use in Non-Cancer Pain recommends seven essential components which the researchers believe are key to programmes to taper opioid prescribing and gives examples of best practices and resources to aid GPs, prescribing nurses and nurse practitioners alike. So, how can we implement this into our practice?
THE SEVEN KEY FEATURES OF THE TOOLKIT
1. There needs to be a clear expectation that opioid de-prescribing is the responsibility of prescribers
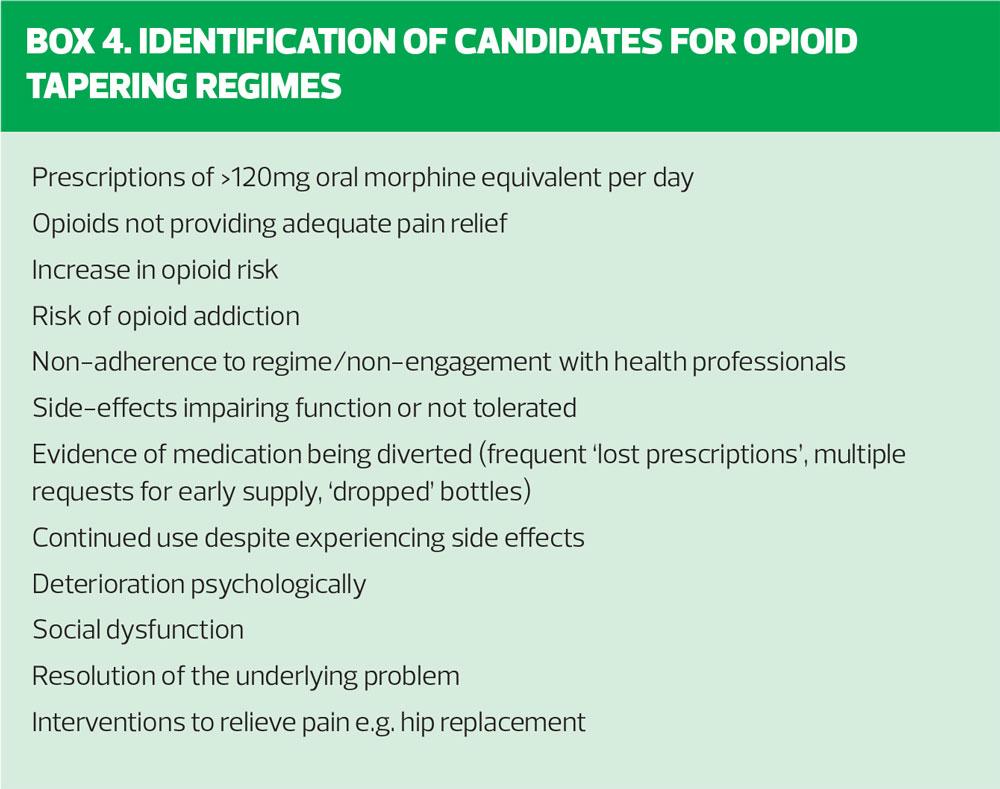
The principle recommendation is that de-prescribing of opioids must be seen as an absolute priority and the toolkit advocates that practices should be incentivised to do so by their CCG through Prescribing Incentive Schemes/Prescribing Quality Improvement Schemes. The toolkit highlights work undertaken by the Brighton and Hove CCG Medicines Management Team as an example of good practice in targeting high dose opioids in chronic non-malignant pain to improve patient care and health outcomes.7 The incentivised target identified patients who met specific criteria for opioid use (drug/dose/strength) but who were neither on the palliative care register nor had a diagnosis of cancer as identified through GP clinical system searches. These patients were then offered a review by clinicians for individual management and collaborative goal-setting, with CCG support for intervention and dose reduction programmes, provision of resources to support alternative measures to reduce pain, signposting to other programmes and secondary care support. Practices therefore need to identify those patients on their list who are no longer benefiting from opioid use or may be at risk of dependence and consider an interventional approach to tapering their use (Box 4).
2. Information about the consequences of excess opioid use
The old adage ‘forewarned is forearmed’ is never more relevant. Do we, as GPNs, feel fully informed about excess opioid use and do we feel capable enough to address the consequences of this during consultations with our patients? The Faculty of Pain Medicine (FPM) of the Royal College of Anaesthetists has a wealth of resources relating to opioid prescribing for us to access for our clinical practice. FPM recommends that opioid treatment should not be continued in cases where severe pain persists despite the use of opioids as it is evidently ineffective.8 Furthermore, the guidance suggests that doses above an oral morphine equivalent of 120mg/day (see Box 3 for FPM dose equivalents) provide no greater therapeutic benefit but the risk of side-effects continues to escalate. In addition, ineffective prescribing is associated with a significant financial burden, due to the use of concomitant medications to prevent and manage side-effects and the increased use of the healthcare system through increased GP appointments, A&E attendances and hospital admissions, not to mention the social implications and reduced quality of life, dependence and poor social functioning associated with opioids.
The Toolkit singles out the Dorset CCG resource pack on Opioid Prescribing for Chronic pain for use in Primary Care, which provides not only information on the consequences of excess opioid use but also guidance on opioid use, tapering regimes, resources and case studies.9 Undoubtably, as practitioners we need to have the understanding of the consequences of excess opioid use to have confident conversations with our patients and share factual and evidence-based information.
3. Information about how to taper
Identification of patients that require de-prescribing of opioids is one thing but actively implementing tapering regimes can be quite another. The Toolkit advocates the use of individual tailoring as more successful than prescriptive regimes. Undertaking an assessment of risk and associated factors is necessary to shape such an approach. For example, consider:
- The patient’s emotional and mental wellbeing
- Accompanying alcohol/substance abuse?
- History of opioid or prescription treatment misuse
- How the patient has historically engaged in healthcare services
- Opioid dose, duration of treatment, and concomitant medications, especially benzodiazepines, gabapentinoids or sedatives
- Current side-effects experienced versus level of improvement in pain
Both the Faculty of Pain Medicine and West Suffolk CCG have produced excellent guidance documents and resources to aid clinicians in tapering and stopping long term opioid treatment, as highlighted in the Toolkit.10,11 This guidance suggests that tapering regimes should include:
- Discussion and explanation of the need for reducing/stopping opioids
- Goal setting with the patient
- The role of tapering and choice of reduction scheme
- Assessment and monitoring of pain and effect of tapering on mood
- Close collaboration and support during tapering
- Withdrawal symptoms and management
- Additional support from drug and alcohol services when required
- Referral to secondary care if not successful
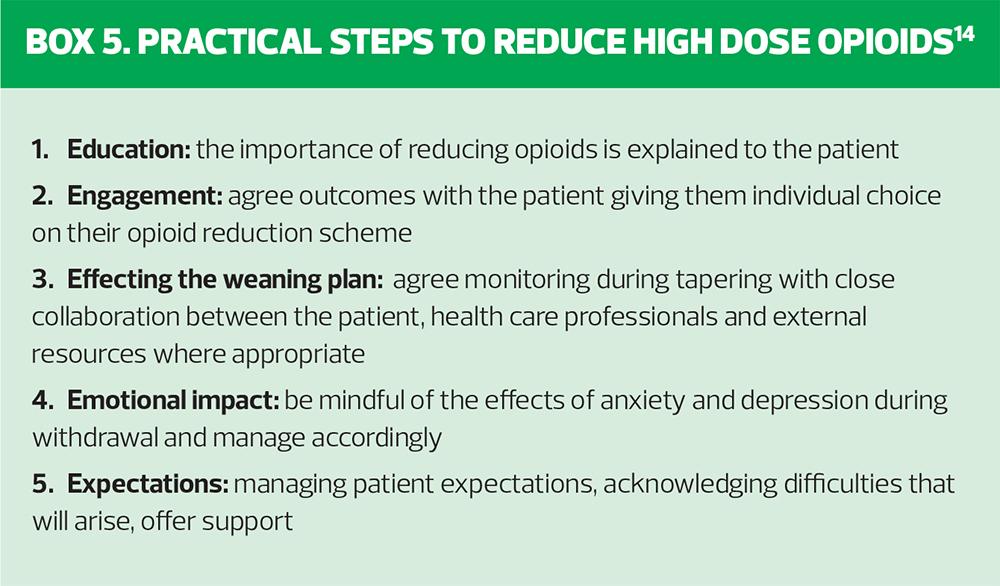
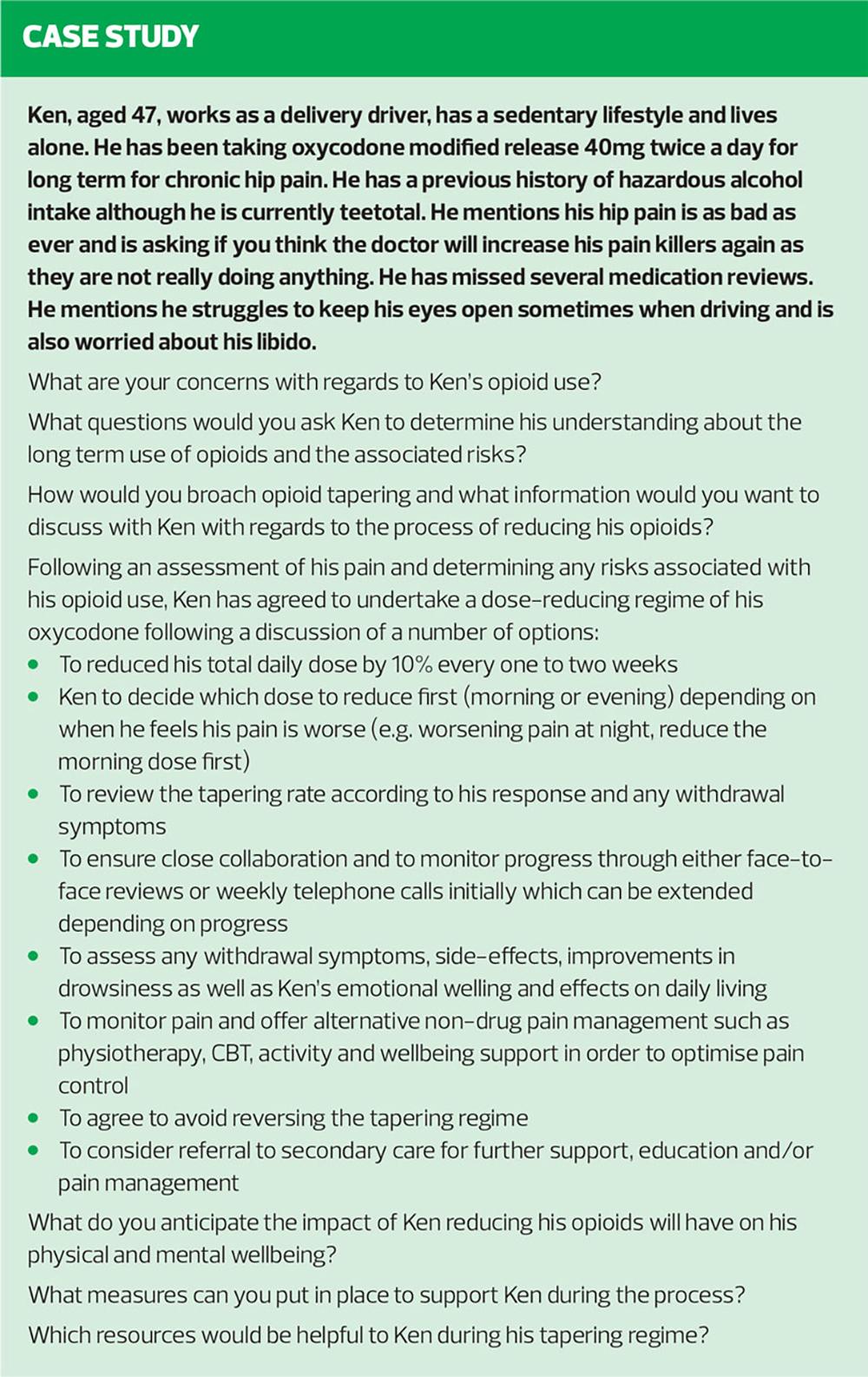
Box 5 highlights practical steps to reducing high dose opioids in terms of supporting patients through the process of tapering. Rates of tapering vary accordingly to each individual patient – some patients may be receptive to faster tapering whereas others may need a slower regime. The resource box provides a number of excellent resources with a variety of tapering regimes from a number of CCGs around the country, recommended in the toolkit and which provide informative further reading.
4. Prescribers with appropriate knowledge and skills to initiate tapering discussions and navigate the patient pathway
The toolkit advocates that prescribers who initiate opioid tapering need to be able to confidently explore the patient’s beliefs and concerns associated with a reduction in their analgesics. Knowing the availability of local resources and referral pathways to pain management specialists, mental health services and drug dependency organisations is vital in order to offer additional support when needed. Offering alternative pain treatment management such as activity programmes, physiotherapy, CBT, relaxation techniques and mindfulness programmes through wellbeing support may be additional weapons in your arsenal to aid opioid tapering.
As nurses we must always practise within our NMC Code.12 In truth, how many of us working in primary care feel we have the skills, knowledge, competence and experience to undertake opioid tapering? But with good guidance, knowledge, professional support and the judgement to seek further advice and referral this can certainly be an extension of the GPN/ANP role in Primary Care.
The toolkit recommends training programmes for practice nurses, including online courses such as the 10 minute CBT programmes, the Charlie Waller Memorial Trust mental health awareness and behaviour change for practice nurses, and the Mental Health Awareness for Practice Nurses with e-Learning for Health. As well as undertaking such training, shadowing medical colleagues can provide opportunities to expand your knowledge.
5. A consistent approach by all members of the healthcare team
Fully supporting a patient who is tapering their opioid analgesia needs to be consistent amongst all individuals and organisations for any intervention to be truly effective. Communication and the avoidance of conflicting advice and approach are paramount. What systems could you consider to put in place to ensure consistency of communication for your patient both within your own practice setting and as part of the wider disciplinary team? Is this truly achievable and how would you manage a situation where there is a conflict of advice or disengagement with the process by the patient? Food for thought certainly but situations that are absolutely essential to consider as part of the management of opioid tapering. The Toolkit identifies the benefits of shared training materials within all disciplines involved in opioid tapering and a shared and agreed system of communication to avoid inconsistencies and to be able to fully support the patient.
6. Comprehensive education for patients
This seems obvious but are patients aware of, and understand the risks of opioid use and reduced benefits with long-term use? Are we, as GPNs, confident enough to manage a patient’s expectations? As recommended by the Toolkit, the Somerset Community Pain Management Service website has information for patients – and indeed professionals – to share and inform about pain management such as understanding pain, goal setting, looking at modifiable factors in pain relief and top tips for coping with pain.13
It is evident that those patients undergoing opioid tapering who are also fully informed, and have access to further resources to support the process, are more likely to succeed. Patient education is therefore a fundamental part of tackling chronic opioid use, to ensure they understand the consequences of excess opioids, what they should expect from a tapering regime and where to access support along what may be an arduous journey. The level of patient engagement is pivotal to the success or failure of any intervention and education and understanding is a prerequisite.
7. A pathway for patient management including access to appropriate levels of psychological and physical support
The Toolkit acknowledges that pathways for supporting patients through opioid tapering will vary depending on locally available resources, population demographics and regional variations. Developing bespoke pathways that take into account local needs and services is recommended by the researchers as an effective approach to intervention. This could certainly be at CCG level or within the emerging Primary Care Networks, to amalgamate local resources in the community, with mental health services, social care and pharmacy services as part of the pathway.
The Live Well with Pain online resource has practical tips and advice for clinicians and patients alike such as: supporting self pain management and using ‘The Pain toolkit’; useful guidance and templates for opioid prescription reviews; opioid decision guide; resources for tapering opioids and top tips from pain specialists in primary and community care.
IS THERE A ROLE FOR GPNs?
So, what is the GPN’s role in opioid tapering - direct or indirect? There will be GPNs who feel confident and have the requisite expertise and experience to manage patients who have been using long term opioids for non-cancer chronic pain and are happy to instigate intervention programmes as part of a multidisciplinary team. For many it will be a question of vigilance in identifying patients who are at risk. For example, those patients who have repeat upon repeat prescription for opioids, which may not have been reviewed for some time. It could become evident when seeing patients for consultations, including Long Term Conditions review or through medication reviews. A patient may express symptoms relating to side effects of their opioid over-use such as somnolence, poor concentration or constipation. They may present with pain that is showing no improvement despite taking increasing amounts of analgesia, or they may be avoiding self-management options. Having an awareness of these patients, referring to colleagues and directing patients to resources would be a fundamental step in the process of opioid tapering.
CONCLUSION
While opioid use is clearly beneficial for managing pain for our end-of-life patients, its role in non-cancer chronic pain is more equivocal. In general practice we need to be proactive in identifying patients who would benefit from opioid tapering. But there will inevitably be practical and psychological challenges that will ensue. Will we, as GPNs, worry about the consequences? The impact of opioid withdrawal can be fraught with emotional upheaval, hampered by withdrawal symptoms, patient disengagement with the process – not to mention managing the pain itself with alternative therapy.
With training, the right pathways, the necessary support and referral opportunities, we can, as members of the primary care team, initiate effective interventions that ultimately improve the overall patient outcome.
REFERENCES
1. Mordecai L, Reynolds C, Donaldson L, et al. Patterns of regional variation of opioid prescribing in primary care in England: a retrospective observational study. Br J Gen Pract 2018;68(668):e225-e233
2. Live well with pain. The great opioid side-effect lottery. 2018. livewellwithpain.co.uk/resources/medicines-and-your-patient/the-great-opioid-side-effect-lottery/
3. Chena T-J, Chenb L, Kerry M et al. Prescription opioids: Regional variation and socioeconomic status – evidence from primary care in England. Int J Drug Policy 2019;64:87-94
4. GP Online. Toolkit helps GPs tackle 'chronic' rise in opioid prescribing May 2019 www.gponline.com/toolkit-helps-gps-tackle-chronic-rise-opioid-prescribing/article/1584380
5. Royal College of Anaesthetists, Faculty of Pain Medicine. Office for National Statistics Data. www.rcoa.ac.uk/faculty-of-pain-medicine/opioids-aware/clinical-use-of-opioids/ons
6. University of East Anglia. Toolkit for Tackling Chronic Opioid Use in Non-Cancer Pain. 2019. Available at: http://www.uea.ac.uk/pharmacy/research/chronic-opioid-use-in-non-cancer-pain/toolkit
7. NHS Brighton and Hove Clinical Commissioning Group. Prescribing Quality Improvement Scheme and Action Plan: Prescribing Incentive Scheme 2017-2018 www.gp.brightonandhoveccg.nhs.uk/prescribing-quality-improvement-scheme-and-action-plan
8.Royal College of Anaesthetists, Faculty of Pain Medicine/ Public Health England. Opioids Aware: A resource for patients and healthcare professionals to support prescribing of opioid medicines for pain. www.fpm.ac.uk/faculty-of-pain-medicine/opioids-aware
9. NHS Dorset Clinical Commissioning Group. Dorset Opioid Prescribing for Chronic Pain: Resource Pack, 2018
10. NHS West Suffolk Clinical Commissioning Group. Opioid Tapering Resource Pack, 2018.
11. Royal College of Anaesthetists, Faculty of Pain Medicine. Tapering and Stopping, 2019. www.rcoa.ac.uk/faculty-of-pain-medicine/opioids-aware/structured-approach-to-prescribing/tapering-and-stopping
12. Nursing and Midwifery Council. The Code: Professional standards of practice and behaviour for nurses, midwives and nursing associates, 2018. www.nmc.org.uk/standards/code/
13. Somerset Community Pain Management Service. www.somersetpain.co.uk
14. Oxford University Hospitals. Guidance for opioid reduction in primary care, 2017 www.ouh.nhs.uk/services/referrals/pain/documents/gp-guidance-opioid-reduction.pdf
15. Royal College of Anaesthetists, Faculty of Pain Management: Dose Equivalent and Changing Opioids, 2019. www.rcoa.ac.uk/faculty-of-pain-medicine/opioids-aware/structured-approach-to-prescribing/dose-equivalents-and-changing-opioids