Meeting the needs of people with a learning disability
SARAH COLEMAN,
SARAH COLEMAN,
PGDip
Health Policy Officer, Mencap
The 1.4 million people with learning disabilities in the UK rely on primary care services, so it is vital that we are not only equipped to meet their needs, but can also help them navigate the rest of the NHS and ensure that colleagues in secondary care have the information they need to organise the right support
Mencap, the UK charity for people with learning disabilities, defines learning disability as ‘a lifelong reduced intellectual ability and difficulty with everyday activities, e.g. household tasks, socialising or managing money, affecting someone for their whole life.’1
People with a learning disability tend to take longer to learn and may need support to develop new skills, understand complicated information and interact with other people: in short, all the key elements of a successful interaction with a healthcare professional. Without the right support, many people with a learning disability will find it very difficult, and in some cases impossible, to access health services at all.
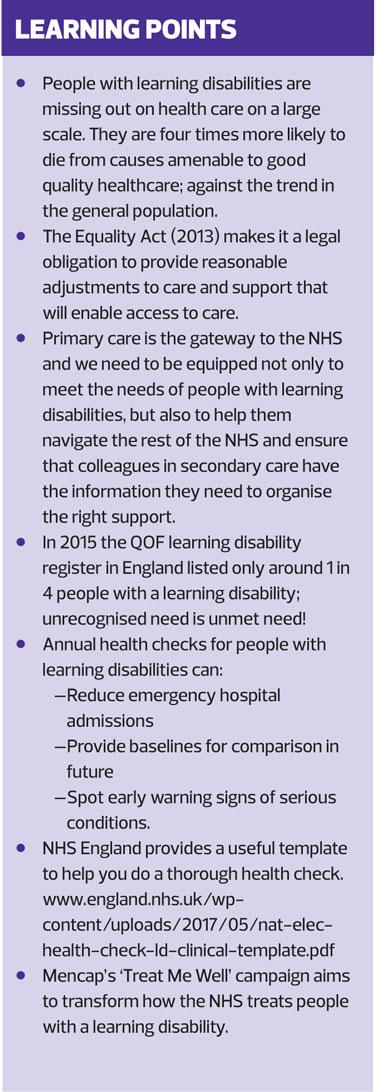
The consequences of missing out can be dire. The Confidential Inquiry into the Premature deaths of people with a Learning Disability, (CIPOLD),2 found that people with learning disabilities were missing out on a large scale and were four times more likely to have died from causes amenable to good quality healthcare than the general population. This is against the usual trend of avoidable deaths in the general population from causes that could have been preventable by public health measures. Consequently, many of the methods taken to improve health in the general population may not be effective in tackling the particular issues affecting people with a learning disability.
KEY ISSUES
There are a number of key issues for people with a learning disability.
Diagnostic overshadowing
This occurs when healthcare professionals fail to recognise symptoms of serious health conditions, attributing them instead to someone’s disability.
Delays in diagnosis and treatment
CIPOLD found this to be a major cause of avoidable death, because of issues such as diagnostic overshadowing and difficulty accessing healthcare services. CIPOLD did not find particular problems with people reporting they were ill or unwell in the first place.
Failures to follow the law
Failure to understand and implement the Equality Act,3 Mental Capacity Act,4 and Accessible Information Standard,5 can lead to people not being able to access health services or be involved in decision making and may result in the inappropriate issue of ‘Do Not Attempt Cardiopulmonary Resuscitation’ (DNACPR) orders.
Lack of reasonable adjustments to care
This can result in many people being unable to access the health services they need. This can arise due to people’s learning disability and support needs not being identified in the first place, or adjustments not being made once they are known.
Lack of co-ordination across care pathways
People with learning disabilities often have more than one long term health condition. However, CIPOLD found that a lack of co-ordination and information sharing between different care pathways, combined with a lack of awareness and/or misunderstanding of the support available to people with a learning disability in the community, could lead to people missing out on the care they needed.
Over-medication
Every day, an estimated 35,000 people with learning disabilities and/or autism are prescribed psychotropic medications with no clinical indication. The ‘Stopping Over-Medication of People with a Learning Disability, Autism or Both’ (STOMP) campaign from NHS England aims to tackle this problem.6
Poor communication
Despite the introduction of the Accessible Information Standard in 2016,5 we know that many people with a learning disability still experience difficulties communicating with healthcare professionals. This can include both verbal and written communication and extends to problems such as inaccessible telephone systems, not being spoken to directly in healthcare appointments or not being given enough time to understand vital information.
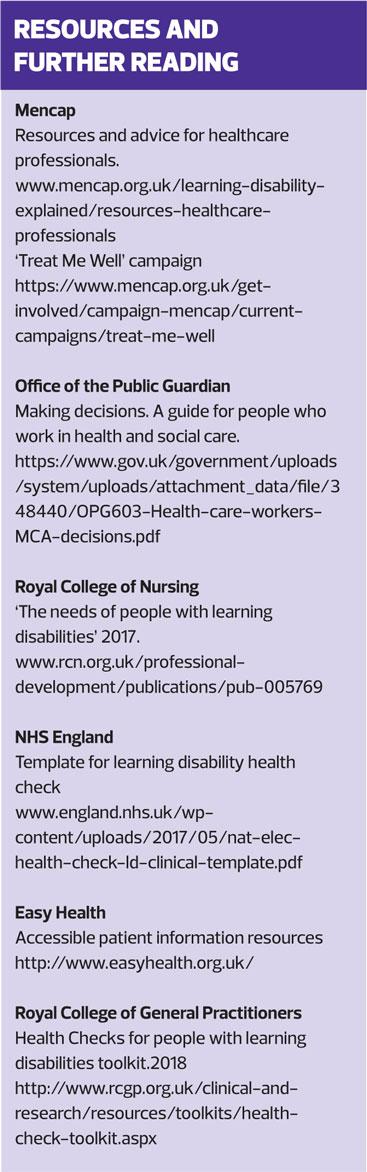
The Royal College of Nursing has produced a guide called ‘The needs of People with Learning Disabilities,’7 which can help you understand more. (See Resources and Further Reading)
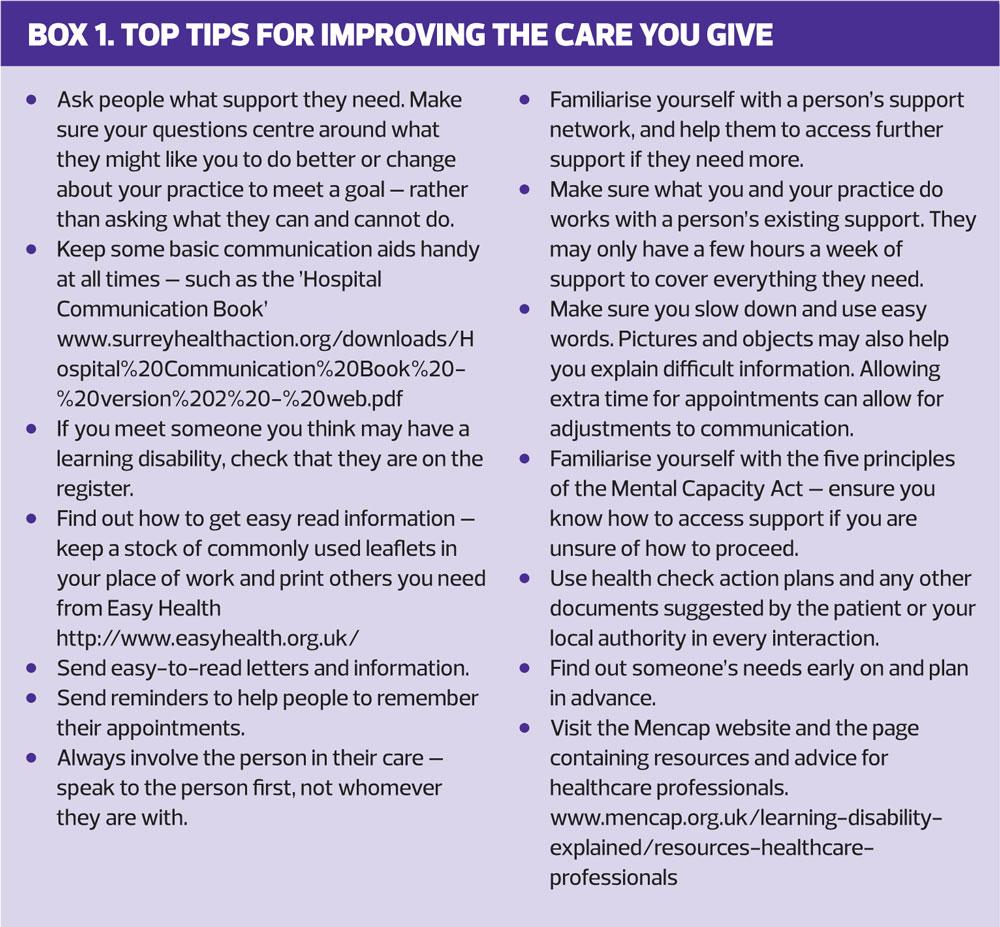
REASONABLE ADJUSTMENTS TO CARE
Reasonable adjustments to care make a big difference and are also a legal obligation under the Equality Act 2010.3 These adjustments are often small and simple, such as:
- Allowing a few extra minutes in an appointment to ensure that someone has the time they need to communicate
- Where possible, making sure someone can see a healthcare professional who knows them well
- Providing a leaflet in easy read information.
However, even these ‘simple’ adjustments may be reliant on an organisation providing the resources to make them happen: a colour printer for example, or an appointment system that can cater for longer sessions.
Some reasonable adjustments may require more planning and multidisciplinary working, e.g. organising sedation for a patient requiring a standard procedure, such as a blood test. However, with support at an organisational and commissioner level, this does not need to be difficult. It is important that organisations recognise that staff training may be necessary if they are to meet the needs of people with a learning disability. Similarly practices will need to be sufficiently flexible in order to accommodate adjusted care.
Currently there seems to be a very mixed picture of how individual healthcare professionals and the services they work in are able to meet the need for reasonable adjustments; yet the need for them is constant and must be met by everyone working in the health service. That is why Mencap’s new campaign, ‘Treat Me Well’, is focused on reasonable adjustments and learning disability training for healthcare professionals. The Learning Disability Core Skills and Education Framework from Health Education England sets out the skills and knowledge required to meet the needs of people with a learning disability and as part of the campaign we are calling for this to be used across health services in order to plan training.8
SUPPORT TO MAKE DECISIONS
The Mental Capacity Act (MCA),4 is a key piece of legislation. First, it states that everyone must be assumed to have capacity to make their own decisions. It places a duty on services to give individuals the support they need to make each decision before they can be assessed as not having capacity. When this does occur, and a best interest decision needs to be made, the individual must be as involved as they can be, as must those close to them. Not following the MCA can leave people left out of decisions affecting their care and, at worst, can result in inappropriate decisions to withhold lifesaving treatment.
Policy and training frameworks can tend to put more focus on what to do when someone lacks capacity to make a decision, without an equal focus on how to support people to be involved in decision making themselves. Extra time, accessible information, creative ways of explaining or communicating, support to retain information and effective use of advocacy can all make a big difference, and it is important that all healthcare professionals are confident in supporting people to make their own decisions.
THE ROLE OF SUPPORTERS
Some people with a learning disability may bring their own supporters to appointments. Everyone has a different relationship with their supporter – who may be paid staff or family carers – and everyone will need different support to manage their healthcare. The person themselves and their supporter can help you understand their role and how best to include them in appointments. Always engage directly with the person with a learning disability unless you are directed otherwise. Ask how they like their supporter to be included: an experienced supporter will know what to do and help you to make sure the person is included – others may need more support from you.
In this time of austerity, people’s support is increasingly limited, and pressure on carers is immense. You can help by making sure that waiting time is kept to a minimum and that people are easily able to book appointments that suit them.
If you meet a patient who you feel may benefit from more social care support, it may be wise to help them to ask for more support from their local authority and have their care needs reassessed – or indeed, for some people, to be assessed for the first time. Remember that carers have a right to ask for an assessment of their needs too.
AN UNKNOWN NEED IS AN UNMET NEED
A key reason that people miss out on the reasonable adjustments they need, is because the need for support is unknown. Sometimes the healthcare professional is completely unaware of the person having a learning disability to begin with. The importance of good record keeping, thorough history checking and sharing of information cannot be overstated.
People with learning disabilities are likely to have a number of difficulties in communicating relevant information about their medical history. Many will rely on you to support them to do this. It’s important that you know how to find out about someone’s support needs, record them and how to share with others if necessary. You can help people to share their own information and keep track of their healthcare with a health action plan – which we’ll talk about later.
CIPOLD found that GP referrals commonly did not mention learning disability, and hospital ‘flagging’ systems, to identify people with a learning disability who needed reasonable adjustments, were limited. If you need to refer someone to hospital and think they may need support or reasonable adjustments, you can get in touch with the Learning Disability liaison nurse at the hospital (most have one) or flag it with the community learning disability team. Consider supporting the person to fill out a hospital passport, which they can use to communicate their needs with hospital staff. A template for this is available at www.mencap.org.uk/advice-and-support/health/our-health-guides.
It is important to identify the kinds of support someone will need in a referral, rather than just mentioning a learning disability. The staff on the other end may not be as familiar with how to support someone with a learning disability as you! Tell people what they need to know to provide the right support.
Recently, there has been a drive to encourage people to add additional information to their Summary Care Record, which can include top line information about their support needs. Information about a medical diagnosis may be relevant, but it’s the support people actually need which is really helpful. It may also be useful to note things that a person CAN do with the right support.
All this relies on a primary care provider knowing which patients have a learning disability in the first place and we know there are problems with this too. Clinical codes and registers can help us to identify patients, but we also know that not every person with a learning disability is known to their GP or other services.
QUALITY AND OUTCOMES FRAMEWORK
Every GP practice should have a register of all patients, of all ages, with a learning disability as part of the QOF contract with NHS England. In 2015 the QOF learning disability register in England listed only around one-in-four people with a learning disability: three out of four are missing.9 This ‘missing’ majority may not have received a diagnosis of learning disability at all, or they may have received support at school which has now stopped. It is really important that people are on the register. They are out there, and they are using primary care services: your job is to help find them.
One of the best ways to encourage people to be on the register is to focus on the benefits and support they could receive once their needs are recognised, rather than it being about labelling. The important message here is that people do not need to have undergone a formal assessment with social services to be on the learning disability register; this is a matter that the clinician can decide. If you feel a patient probably has a learning disability, and may benefit from the kinds of support we have discussed, including an annual health check, consider adding them to the register. NHS England is currently developing resources to help with identifying people with a learning disability and there may also be local screening tools available for you to use.
It is also important to note that even if patients are given a clinical code that indicates learning disability, such as the code for Down’s syndrome, they are not automatically added to the QOF learning disability register. One of the best ways to make sure your QOF register is populated to the best of your ability is to run systematic checks against a series of Read codes. You can find more information about this in the RCGP toolkit.10 (See Resources and Activity 3) Make a habit of checking, when you see someone you know to have a learning disability, that they are on the register. We would also recommend that you contact your local learning disability team and cross check your register with theirs.
ANNUAL HEALTH CHECKS
Annual health checks are part of NHS England’s Enhanced Service for people with learning disabilities. GP practices receive £140 for every check completed. These checks can:
- Reduce emergency hospital admissions
- Provide baselines for comparison in future
- Spot early warning signs of serious conditions.
They are also an excellent opportunity to get to know a patient better and find out more about how the practice can meet their support needs. This is why they should be done by someone who knows the patient well and/or who will be involved in leading on their care. Generally, annual health checks are only offered to those on the QOF register, which is another reason it is vital that everyone with a learning disability is on it.
We know that annual health checks can differ in quality: some people report only being seen for 10 minutes while others experience a complete check. The new template from NHS England will help you to do a thorough health check. (See Resources) The template includes markers for various health conditions and also gender/age specific questions. An annual health check is also a great opportunity to add additional information to the summary care record. To find out more about annual health checks or to support someone with a learning disability to find out more about them, see the Mencap campaign ‘Don’t Miss Out’ at www.mencap.org.uk/advice-and-support/health/dont-miss-out/
HEALTH CHECK ACTION PLANS
Every health check should result in a patient being offered a health check action plan. However, the data and anecdotal evidence suggest this is often not happening, despite it being a prerequisite of the health check payment.
Health check action plans can be invaluable in supporting a person to manage their health and for all parties involved in a person’s care to be kept informed. However, it is common for people with a learning disability to report their plan not being used, which can make the exercise seem pointless. We need all healthcare staff to use health check action plans in every interaction with people with a learning disability.
CONCLUSION
The responsibility to meet the needs of people with a learning disability is shared across the health service and relies not only on individuals adjusting their own practice but also on organisations and systems providing the resources and support healthcare professionals need. It is important for us to remember that what may seem like a big or complicated change for an individual staff member to make, does not seem at all unreasonable when we think of the health service as a whole and the resources that are available within it.
We also need to remember why we are making adjustments. We are doing it so that:
- People can access the person-centred care they need, first time around
- They can remain healthy for longer
- They can access diagnoses and treatments in a timely way that means they have a greater chance of getting better.
Doing things differently may seem, in a cash and resource strapped service, like extra work or extra money, but in the long run it is actually more efficient and makes good financial sense, as well as being the right thing to do.
The situation is by no means all bleak. We know there is some excellent practice out there, but sadly this is not standard. There is a need for those of us who work in primary care to share good practice and encourage others. We need to speak out if we are not able to meet the needs of someone with a learning disability and to keep calling for the systems and resources we need to support them. Those of us with leadership, management and commissioning responsibilities need to ensure that staff are trained, aware and ready to make the reasonable adjustments that can make such a difference to our patients. In addition, we need to lobby to ensure that local healthcare systems are able to work together to accommodate true multi-disciplinary working.
Regardless of how someone’s learning disability affects them – it is how we run our health service and deliver our care that really makes the difference to whether someone is able to access the good quality healthcare they need.
REFERENCES
1. Mencap. What is a learning disability? Our definition, 2016. www.mencap.org.uk/learning-disability-explained/what-learning-disability
2. University of Bristol. Confidential Inquiry into premature deaths of people with learning disabilities (CIPOLD), 2013 http://www.bristol.ac.uk/media-library/sites/cipold/migrated/documents/fullfinalreport.pdf
3. The Equality Act – Full act: http://www.legislation.gov.uk/ukpga/2010/15/contents
4. Mental Capacity Act 2005 https://www.legislation.gov.uk/ukpga/2005/9/contents
5. Accessible Information Standard
https://www.england.nhs.uk/ourwork/accessibleinfo/
6. NHS England. Stopping over-medication of people with learning disability, autism or both, 2016 https://www.england.nhs.uk/wp-content/uploads/2017/07/stomp-gp-prescribing-v17.pdf
7. Royal College of Nursing. The needs of people with learning disabilities. 2017. Publication code 005769 www.rcn.org.uk/professional-development/publications/pub-005769
8. NHS Health Education England. Learning disabilities core skills education and training framework, 2016. http://www.skillsforhealth.org.uk/images/resource-section/projects/learning-disabilities/Learning-Disabilities-CSTF.pdf
9. Public Health England. People with learning disabilities in England 2015: Main report, 2016 https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/613182/PWLDIE_2015_main_report_NB090517.pdf
10. Royal College of General Practitioners. Health Checks for people with learning disabilities toolkit, 2018 http://www.rcgp.org.uk/clinical-and-research/resources/toolkits/health-check-toolkit.aspx