Ethical healthcare: is it under threat?
Beverley Bostock-Cox
Beverley Bostock-Cox
RGN MSc MA QN
Nurse Practitioner Mann Cottage Surgery, Moreton in Marsh
Education Lead, Education for Health, Warwick
As healthcare professionals we are privileged to be allowed access to the most private and intimate areas of peoples’ lives, but this comes with the responsibility of behaving ethically at all times. This article explores the basic bioethical principles that underpin healthcare and considers how these principles can be challenged in day-to-day practice
BIOETHICAL PRINCIPLES AND THE CODE OF CONDUCT
According to Beauchamp and Childress,1 there are four key bioethical principles:
- Autonomy
- Beneficence
- Non-maleficence
- Justice.
These four principles relate closely to the
so-called ‘4 Ps’ of the Nursing and Midwifery Council’s (NMC) Code of Conduct,2 which advises on how nurses and midwives should behave. These 4 Ps are:
- Prioritise people
- Practise effectively
- Preserve safety
- Promote professionalism and trust.
In the current climate of scarce resources and care by template, it is easy to forget these basic tenets and to breach the NMC code without even realising it, for example, by putting something else such as generic targets or formularies, before patient care. Those charged with balancing the books (or more often, seemingly, cutting those books down into pamphlets!) can appear to have a different agenda from our own, which is to offer the best standard of healthcare possible to people who are trusting us with their wellbeing. Even our own employers may insist that we focus on what we are paid to do (get the Quality and Outcomes Framework [QOF] points) and we may be discouraged from offering services that we ‘are not paid for’, such as smoking cessation. This can lead to a sense of dissatisfaction and impotence if we feel that we are not doing the best we can, but are simply ticking boxes.3
It is therefore interesting to consider how the NMC Code of Conduct and Beauchamp and Childress’s bioethical principles can actually provide a firm foundation, which enables us to resist pressure to ignore the ethical imperative.
AUTONOMY AND BENEFICENCE
Autonomy is an essential element of healthcare and links closely to the concept of prioritising the person in the consultation; the first of the NMC’s 4 Ps. As a clinician, you may be an expert in the subject of the consultation – asthma, diabetes, travel health, cervical cytology, for example – but the patient is the expert in their own, unique self. In an effective consultation respect for autonomy will mean that people are equipped with the requisite amount of knowledge to make their own, competent decisions and that these decisions will then be respected and supported by the professionals involved in their care, irrespective of whether we agree with their decisions. Respect for autonomy should be absolutely central to any healthcare transaction between patient and clinician.
However, autonomous decisions cannot be made without adequate information on which to base those decisions. For example, people who access screening programmes, such as breast, cervical, bowel or prostate cancer screening, or the NHS Health Check programme, should know why they are being offered screening and the implications of any findings. They should also have an appropriate amount of information and time to consider the impact of any interventions before deciding whether to proceed.4 All of this reflects the principle of autonomy, informed consent (or dissent) and shared decision-making, and conforms to the statements in the NICE Quality Standard (QS) on adult patient experience in NHS services.5
NICE QS
The NICE document highlights the importance of the NHS providing a good patient experience and recognises the value of providing a patient-centred service. The QS includes 14 quality statements reflecting some of the issues that are important in supporting autonomous decision making:
- Patients should be treated with respect and honesty (statement 1), and
- Healthcare professionals (HCPs) should be trained in effective communication skills in order to facilitate effective interactions (statement 2).
- Patients should be given the opportunity to discuss their health beliefs, concerns and preferences (statement 4), and
- Be supported by HCPs to understand the relevant treatment options, including the benefits and risks and potential consequences of those options (statement 5).
- Patients should be involved in shared decision making about investigations and treatments (statement 6), and
- Have the right to choose, accept or decline treatment and should know that these decisions will be respected and supported (statement 7).
- HCPs should ensure that all care is tailored to the needs and personal preferences of the individual (statement 9).
These statements, and the QS as a whole, broadly reflect the bioethical principles of autonomy and beneficence and indicate a desire within the NHS to move away from the paternalistic, medical model of care that has prevailed in the past. Although this all sounds good in theory, evidence of the practical implementation of these standards is far harder to achieve. How long an appointment would you need to fully achieve these standards?
It is clear that HCPs should be able to offer clear, unbiased advice regarding the options available to an individual and should be trained to communicate these options effectively, so that each individual can reach a point of informed choice and can act autonomously. The HCP has the factual knowledge about the medical options available (e.g. statin therapy in people with a cardiovascular risk score over 10%) and the individual has to interpret this information in light of their own unique knowledge of ‘self’ which allows them to decide if and how to apply this information to their own situation. This is in line with the philosopher and ethicist John Stuart Mill’s view that an individual’s opinion about well-being immeasurably outweighs that held by anyone else.6
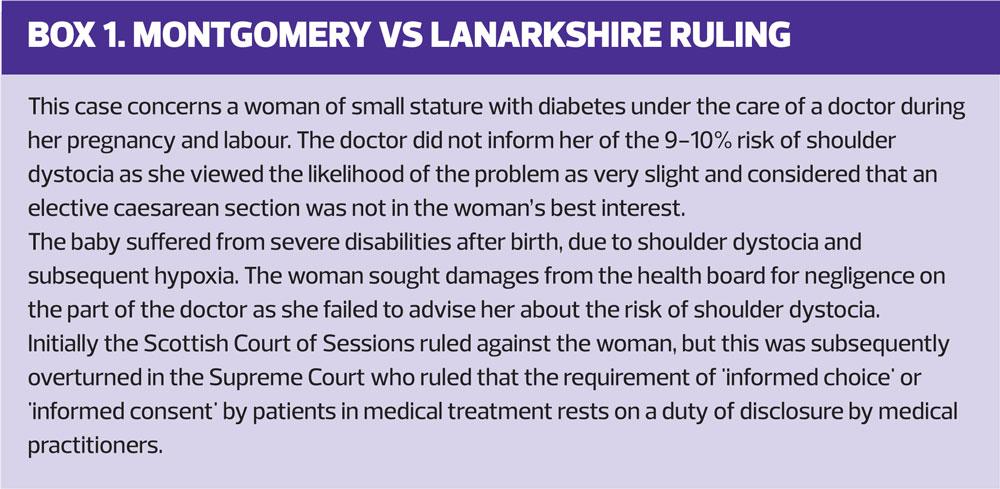
Montgomery vs Lanarkshire case
In any given situation the HCP is tasked with explaining to the patient the nature and significance of the risks and benefits of any intervention. The recent Montgomery ruling (Box 1) underlines the importance of the concept of material risk becoming central to informed decision making.7 When discussing the risks and benefits of any intervention, clinicians should consider whether a reasonable person in the patient’s position, would be likely to attach significance to the risk. As a result of the judgment in the Montgomery case it is vital that clinicians keep detailed records of the information provided to the patient about any significant risk involved in a proposed treatment. The ruling is clear that significance is not determined by how common a side effect is.
If the HCP has managed to do all of this (and we won’t debate the practicalities of this in what might be a 10-minute appointment) the patient is then given the opportunity to accept the recommendations or reject them. This may sound like informed, autonomous decision-making. However, the concept that the patient is truly ‘informed’ and autonomous is open to challenge.
Often, we tend to tailor information in order to ensure that people go along with the accepted view of what should happen (e.g. engaging in screening or immunisation programmes, taking drugs to impact on risk factors, making lifestyle changes to improve long-term outcomes) rather than actually facilitating choice. True beneficence, which respects the patient’s autonomy, would aim to understand the person’s views on what constitutes well-being for them and whether quitting smoking, losing weight or taking medication is part of that view. If quitting smoking is not something that they want to do for holistic reasons (for example, they enjoy smoking, they have friends who smoke and they would feel ostracised if they quit) then the beneficent clinician should be able to recognise and respect those views. This should be the case despite recommendations that smoking cessation is something that HCPs should discuss with smokers at every opportunity, and in spite of the fact that NHS computer templates are designed to remind the clinician (and therefore the patient) about the importance of quitting for as long as that patient continues to smoke.8
Beneficence should not just mean doing good, but doing good in a way which recognises and reflects the patient’s own values as being central to any decision about health related issues. The NHS does not, therefore, always support clinicians to act in line with the view that decisions made by competent individuals should be respected, even if their views and actions are at odds with what clinicians are taught as being ‘best’ for those individuals.9 Rather than being concerned or irritated at the perceived irrationality of ‘unwise’ decisions, the beneficent clinician recognises that perhaps longevity is not the most important thing for all people and that other aspects of their lives may take precedence.
NON-MALEFICENCE
If autonomy and beneficence link to the first two Ps of the NMC Code of Conduct (prioritise people and practice effectively) then the principle of non-maleficence goes hand in hand with the third P, preserve safety.
The Hippocratic Oath (and versions of the same), with the underlying concept of primum non nocere (first do no harm), is based on the importance of not putting patients at risk.10 Once again, careful discussion with individuals, aimed at getting informed consent, will ensure that the inevitable risks of any intervention are carefully weighed up against the benefits and that these are applied specifically to the individual in question and their unique circumstances.
An example of this is the treatment of people with diabetes. In the past, sulfonylureas were often prescribed as a cheap and effective way of lowering blood glucose. Indeed, the NICE guidelines on type 2 diabetes continue to recommend their use,11 in spite of the fact that they are also associated with harm, such as hypoglycaemia, weight gain, the need to self-monitor (which in itself has been associated with an increase in mental health problems) and a potential increase in cardiovascular risk.12–14 In contrast, the American Diabetes Association/European Association for the Study of Diabetes (ADA/EASD) guidelines now recognise that the cardiovascular benefits of newer drugs, such as SGLT2 inhibitors and the GLP1 liraglutide, require them to be placed as second line therapies at least, thus offering the best balance of beneficence and non-maleficence and meeting the NMC’s requirements to practise effectively whilst preserving safety.15–18
Another example of failing to take action to prevent harm is with inhaled corticosteroids (ICS) in chronic obstructive pulmonary disease (COPD). High doses (i.e. fluticasone propionate 500mcg bd, which is equivalent to 2000mcg daily of a standard ICS) have been linked to harmful side effects, including a 64% increased risk of developing diabetes.19 These inhalers should be discontinued, but what has happened in some areas is that they have simply been replaced with a cheaper inhaler with the same dose of ICS and the same level of risk, rather than taking the opportunity with the switch to move to a lower dose combination or, where appropriate, discontinue the ICS altogether and move to a dual bronchodilator. This is not only unethical, breaching the concept of non-maleficence, but it is also medico-legally unwise.
JUSTICE
The bioethical principle of justice underlines the importance of equality and equity in accessing healthcare: if a patient can be prescribed medication in one area of the country but the same medication cannot be prescribed in another, that would not be just. Clinicians are often led to believe that they are not ‘allowed’ to prescribe medication which is not on their local formulary, but this is not so. It may be that there is a preference for certain inhalers, direct oral anticoagulants or insulins in the locality, but that does not mean that they are forbidden. If a clinician deems a non-formulary medication to be right for their patient, it should be prescribed as not doing so would be a breach of ethical and professional responsibility.
Utilitarianism
Sometimes, the concept of utilitarianism is used to argue against tailored care, i.e. the greatest good for the greatest number. Utilitarianism, however, has many critics in the history of philosophy and we should remember that the intervention that costs more initially sometimes pays the biggest dividends in the long term, and that this long term gain may have a big impact on others too. In diabetes care, for example, most of the money spent on treating diabetes is spent on treating the complications,20 and spending more initially (as in the SGLT2 versus sulfonylurea example above) will reap benefits for the individual, the NHS and society as a whole through reducing complication risk in the long term. It’s unfortunate that NHS budgets are often short term and therefore, of necessity, lack vision.
Limiting access by referral
Another example of how access to healthcare can be limited by unjust practices is when access to treatment is limited by referral, i.e. a drug that is freely available in general practice in one area requires the patient to attend another service in order to access it in another area. Examples of this might include some diabetes drugs and medication to support smoking cessation – specifically varenicline, which is not available over the counter but which some patients struggle to access from their GP or nurse. Often the cry is ‘But we are not paid to provide smoking cessation services!’ So let’s revisit that cry, using bioethical principles, the NMC code of conduct and other key elements of working as a healthcare provider.
SMOKING CESSATION, ETHICS AND THE NMC CODE OF CONDUCT
First, the NMC Code of Conduct:
- Prioritise people – the patient wants to access smoking cessation support with you. They know you, they like you and they find attending surgery convenient
- Practise effectively – you should have the competence to provide this service as it is a level one (i.e. basic) competency in the Royal College of General Practitioners (RCGP) competency document for general practice nurses.21 You should therefore be able to provide the service that your patient has requested. If not, you need to complete your training with www.ncsct.co.uk
- Preserve safety – assuming you are competent, you should know how to ensure your patient gets the correct treatment at the appropriate dose and for a suitable period of time (e.g. varenicline must be given for at least 12 weeks.22)
- Promote professionalism and trust – you have behaved professionally, and the patient should know that you are acting on their behalf, as their advocate, reflecting their needs and preferences.
Now from the standpoint of the four bioethical principles:
- Autonomy – the patient has been able to make an informed decision about if, how, where and when to access smoking cessation support
- Beneficence – they have been supported to ensure that what they do prioritises their overall well-being
- Non-maleficence – any harm has been minimised (i.e. by not sending them away to see someone else and by knowing how to implement effective smoking cessation support)
- Justice – there is equality of access for people irrespective of their geographical location, work patterns or other possible barriers to treatment.
Smoking cessation is one of the most important things any healthcare provider can engage in to improve the health of their patients. If we are being paid to provide diabetes care, respiratory care, reduce cardiovascular risk, screen for cancer etc., we are being paid to provide smoking cessation. This should be considered to be central to the care we provide, not as a bolt on.8,23
ETHICS AND LONGEVITY
The World Health Organization defines health as … a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity’.24
Nonetheless, the presence of disease is known to be linked to poor physical, mental and social well-being.25
Interventions aimed at increasing the length of time that people live are the cornerstone of NHS care. (While there is little doubt that smoking cessation is effective, the evidence for the clinical and cost effectiveness of the NHS health check programme is controversial.26) Health-related quality of life, however, includes not only physical and mental health, but also the ability to carry out the activities of daily living, social relationships, and financial status.27 We may tend to think that our role is to reduce morbidity and mortality from avoidable diseases, such as cardiovascular disease, but disease morbidity can come in a range of guises, such as loneliness, isolation, loss of dignity and financial hardship. Interventions aimed at lengthening lifespans therefore have the potential to increase suffering. This sits badly with the bioethical principle of non-maleficence, ‘primum non nocere’ – first do no harm.
The Global Burden of Disease study,28 indicated the increasing tendency for older people to be living longer but in poorer health, with the greatest reduction in their quality of life occurring towards the end of their lifespan. Studies of older patients’ views on quality of life versus quantity are limited, possibly indicating the general reluctance to address the issue of the period of time at the end of life, including the risks and benefits of prolonging lifespans. There is a body of discussion on end of life care for people with a terminal illness but far less on the views of elderly people who are not terminally ill but are ‘dying’ nonetheless.
One study in older people with cancer indicated a preference for quality of life over quantity.29 In a review of end of life care in terminal heart failure, it was noted that, in a health environment where the focus is on ‘curing’, there may be significant challenges about having meaningful discussions about quality versus quantity of life and end-of-life planning.30 If this is so when treating terminal illness, it is likely to also be an issue with people who are simply ageing rather than imminently dying, yet it is rarely discussed.
Fortunately, there is a developing recognition that in older people, quality of life may be the most important element of their care. Tools such as the STOPP START guide,31 may help patients and clinicians to decide when to initiate and stop drug treatments. The top five drugs associated with adverse drug reactions in older people should be a key priority for discussion. These include:
- Non-steroidal anti- inflammatory drugs
- Diuretics
- Warfarin
- ACE inhibitors and angiotensin receptor blockers
- Anti-depressants.32
Reasons for prescribing (or continuing) medication in older people might include if the drug gives daily symptomatic benefit, prevents rapid worsening of symptoms, or replaces a hormone vital for normal function e.g. levothyroxine.33
CONCLUSION
Ethical principles are an essential part of every consultation carried out in general practice and yet time constraints and issues around knowledge and comprehension of these principles may prevent truly ethical healthcare from being the norm. Healthcare law is the close sibling of ethical practice, as seen in the Montgomery case, and clinicians should be aware of the opportunities and challenges afforded if ethically and legally competent consultations are going to be carried out in order to reduce risk to patients and clinicians alike.
Conforming to ethical principles in day to day practice increases the likelihood of both patient and clinician staying as legally safe and ethically sound as possible within tailored, patient-centred consultations. GPNs should remember their NMC Code of Conduct and should be prepared to advocate for the patient if they feel that safe and ethical practice is being compromised.
REFERENCES
1. Beauchamp TL, Childress JF. Principles of Biomedical Ethics. 2013 Oxford University Press, Oxford
2. Nursing and Midwifery Council. 2015. The Code https://www.nmc.org.uk/globalassets/sitedocuments/nmc-publications/nmc-code.pdf
3. Ipsos MORI Research. The recruitment, retention and return of nurses to general practice nursing in England. 2016 https://www.england.nhs.uk/wp-content/uploads/2017/07/recruitment-retention-return-of-nurses-to-general-practice.pdf
4. Stacey D, Légaré F, Col NF, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Library. 2017 doi:10.1002/14651858.CD001431.pub5.
5. NICE QS15. Patient experience in adult NHS services. 2012. https://www.nice.org.uk/guidance/qs15
6. Mill JS. On Liberty. 1885. New York, NY JB Alden pg. 128
7. Montgomery v Lanarkshire Health Board. 2015 UKSC 11 https://www.supremecourt.uk/decided-cases/docs/UKSC_2013_0136_Judgment.pdf
8. Department of Health. Smoke free pledge. 2018 http://smokefreeaction.org.uk/wp-content/uploads/2018/01/smoke-free-pledge_v13.pdf
9. Brock DW, Wartman SA. When competent patients make irrational choices. N Engl J Med 1990;322;1595-1599
10. Oxtoby K. Is the Hippocratic oath still relevant to practising doctors today? BMJ 2016; 355 i6629 doi: https://doi.org/10.1136/bmj.i6629
11. NICE NG28. Type 2 diabetes in adults. 2017 https://www.nice.org.uk/guidance/ng28
12. Sola D, Rossi L, Schianca GP, et al. Sulfonylureas and their use in clinical practice. Arch Med Sci 2015;11:840–8. doi:10.5114/aoms.2015.53304
13. Malanda UL, Welschen LM, Riphagen II, et al. Self-monitoring of blood glucose in patients with type 2 diabetes mellitus who are not using insulin. Cochrane Database of Systematic Reviews 2012; Jan 18;1:CD005060. doi: 10.1002/14651858.CD005060.pub3.
14. Evans JMM, Ogston SA, Emslie-Smith A, et al. Risk of mortality and adverse cardiovascular outcomes in type 2 diabetes: a comparison of patients treated with sulfonylureas and metformin. Diabetologia 2006;49: 930. https://doi.org/10.1007/s00125-006-0176-9
15. Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). 2018 http://diabetologia-journal.org/wp-content/uploads/2018/09/EASD-ADA.pdf
16. Zinman B, Wanner C, Lachman JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in Type 2 diabetes. N Engl J Med 2015;373:2117-2128 DOI: 10.1056/NEJMoa1504720
17. Neal B, Perkovic V, Mahaffey KW, et al, on behalf of the CANVAS Program Collaborative Group. Canagliflozin and cardiovascular and renal events in Type 2 diabetes. N Engl J Med 2017;377:644-57
18. Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med 2016;375:311-322 DOI: 10.1056/NEJMoa1603827
19. Suissa S, Kezouh A, Ernst P. Inhaled corticosteroids and the risks of diabetes onset and progression. American Journal of Medicine 2010;123(11):1001-6. doi: 10.1016/j.amjmed.2010.06.019.
20. Hex N, Bartlett C, Wright D, Taylor M, Varley D. Estimating the current and future costs of Type 1 and Type 2 diabetes in the United Kingdom, including direct health costs and indirect societal and productivity costs. Diab Med 2012;29(7):855–862
21. RCGP. General Practice Nurse Competencies. 2015 http://www.rcgp.org.uk/policy/rcgp-policy-areas/nursing.aspx
22. Champix (varenicline) Summary of Product Characteristics. Pfizer Ltd. 2018 https://www.medicines.org.uk/emc/product/266/smpc
23. Public Health England. Health matters: stopping smoking – what works? 2018 https://www.gov.uk/government/publications/health-matters-stopping-smoking-what-works/health-matters-stopping-smoking-what-works
24. World Health Organization. Constitution of the World Health Organization: Principles. 1948 http://www.who.int/about/mission/en/
25. Naylor C, Parsonage M, McDaid D, et al. Long-term conditions and mental health: the cost of co-morbidities. The Kings Fund. 2012 https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/long-term-conditions-mental-health-cost-comorbidities-naylor-feb12.pdf
26. McCartney M. Where’s the evidence for NHS health checks? BMJ 2013;347 doi: http://dx.doi.org/10.1136/bmj.f5834
27. Centers for Disease Control and Prevention. Measuring healthy days: Population assessment of health-related quality of life.2000. https://www.cdc.gov/hrqol/pdfs/mhd.pdf
28. Global Burden of Disease Study. Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 388: 1459–1544
29. Meropol NJ, Egleston BL, Buzaglo JS, et al. Cancer patient preferences for quality and length of life. Cancer 2008;113(12):3459–66
30. Howlett J, Morrin L, Fortin M, et al. (2010). End-of-life planning in heart failure: It should be the end of the beginning. Can J Cardiol 2010;26(3):135–141.
31. NHS England. Toolkit for general practice in supporting older people living with frailty. 2017 https://www.england.nhs.uk/wp-content/uploads/2017/03/toolkit-general-practice-frailty.pdf
32. Pirmohamed M, James S, Meakin S, et al. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18820 patients. BMJ 2004; 329(7456):15-19.
33. NHS England. Toolkit for general practice in supporting older people living with frailty. (STOPP START Medication Review Tool) 2017 https://www.england.nhs.uk/wp-content/uploads/2017/03/toolkit-general-practice-frailty.pdf
Related articles
View all Articles