Coaching – not just for Olympians
Beverley Bostock
Beverley Bostock
RGN MSc MA QN
Advanced Nurse Practitioner
Mann Cottage Surgery
President-elect, Primary Care Cardiovascular Society
Practice Nurse 2024;54(5):26-29
What is health coaching and how can it be used to prevent long term conditions and improve self-efficacy in people who already have a long-term condition so they can self-manage more effectively?
This summer, the Olympic and Paralympic games acted as a reminder about the power of the human body to achieve great things. While most people will never reach such heights in our sporting achievements, physical activity, along with other positive lifestyle behaviours, remains an important part of healthy living, offering benefits for mind and body. When an athlete receives the plaudits of success, recognition for the extended team that helped them to reach this point is, perhaps, less evident. For example, can you name Tom Daley’s diving coach?
Coaching someone to be the best they can be is a huge privilege and general practice nurses (GPNs) often find themselves in this role when supporting people to develop behaviour changes that will go on to reward people with better quality, and quantity, of life. Like those Olympic coaches, the impact that health coaches can have is highly significant.
LEARNING OUTCOMES
After reading this article, you should be able to:
- Define the term 'health coaching'
- Consider the role of the extended general practice team in health coaching
- Recognise the evidence base for optimising outcomes using health coaching
- Implement coaching techniques in practice
WHAT IS MEANT BY ‘HEALTH COACHING’?
Health coaching is a means of supporting people to identify if, why and how they can make changes to improve their physical and mental health, based on their own aims and preferred approaches.1 It uses behaviour change interventions based on psychological approaches, some of which have also been used in sports coaching and business leadership. Although health coaching is often used in the management of long term conditions, it can also be used in disease prevention, for example in people who have been identified as being at risk of developing diabetes or cardiovascular disease, where support with motivation to lose weight, stop smoking or develop a more active lifestyle is key. Health coaching can also help people with low mood to implement lifestyle and behaviour changes which can improve psychological wellbeing. It is an intervention which supports self-management, something which is encouraged in people living with long term conditions such as diabetes, cardiovascular disease, heart failure, asthma, and chronic obstructive pulmonary disease (COPD). Health coaching encourages people to become active and equal partners in their care, so that they can make informed decisions about setting goals and targets, based on their own situation, preferences and perspective. People living with long term conditions are encouraged to manage their condition on a day-to-day basis and know how to respond to signs that the condition is becoming unstable, before seeking medical help, but for many people this can be a challenge. A lack of understanding about the condition or what might help, along with low levels of health literacy in some, means that understanding and implementing a self-management plan is not straightforward. Health coaches can help people to understand more about their condition and how to optimise their well-being through improved health behaviours, including weight management, smoking cessation and other lifestyle changes.
WHO CAN DELIVER HEALTH COACHING?
For GPNs, health coaching is something that may well be a key element of practice already. For example, working with people using motivational interviewing techniques is often second nature to GPNs. Change is unlikely to happen unless people feel there is a point to making any changes, and the reason for changing behaviours will vary from individual to individual. A skilled GPN will help people to identify their motivation to change and maintain their momentum for change at times when it becomes more challenging. However, health coaching is not the sole preserve of GPNs.
The health and well-being team is made up of people with expertise in health coaching and who can engage with people to identify what they want to achieve and how they would like to achieve it. Healthcare workers such as social prescribers can consider the wider issues around support, including how people can access and prepare healthy foods, engage in physical activity, increase social interaction and ensure that they are getting financial assistance where needed. In some areas of the country, health coaching has been commissioned as a service, delivered by a specialist team. However, health coaching works best if the approaches used are embedded into all areas of practice. It should be seen as an integral part of supporting people with long term conditions, with all members of the healthcare team using this approach to optimise outcomes.
WHERE IS THE EVIDENCE FOR HEALTH COACHING?
There is evidence for health coaching in a range of conditions and populations including in long term conditions.2,3 Conn and Curtain describe the benefits of health coaching, with improvements seen in nutrition, physical activity, weight management, medication adherence, and holistic benefits for physiological, behavioural, psychological and social outcomes.4 There are additional benefits for the healthcare team too, including increased job satisfaction through improvements in patient satisfaction, more effective consultations, and enhanced multidisciplinary professional collaboration.4
IMPLEMENTING HEALTH COACHING IN PRACTICE
It is important to think about how, where, when and why health coaching might be used. To that end, a co-production approach is recommended. This means that the team planning to implement the service encourages end-users to be part of developing it, so that it is fit for its intended purpose. Too often in healthcare, plans are put in place for a service or intervention which does not resonate with the people for whom it is intended. Co-design and co-production are ways of ensuring that services are designed by, with and for, the users of the service.
Health coaching can be offered on a one-to-one basis or in groups. Some people will prefer one approach above another, but clearly there are benefits to the NHS from seeing more than one person at a time. This is one of the reasons group consultations work well, helping to address workload as well as healthcare needs.5,6 However, group consultations offer people the opportunity to have their annual review in a group setting, whereas health coaching in groups is different. For example, health coaching can be offered by non-clinical personnel as the primary aim is to enable people to self-manage with confidence.
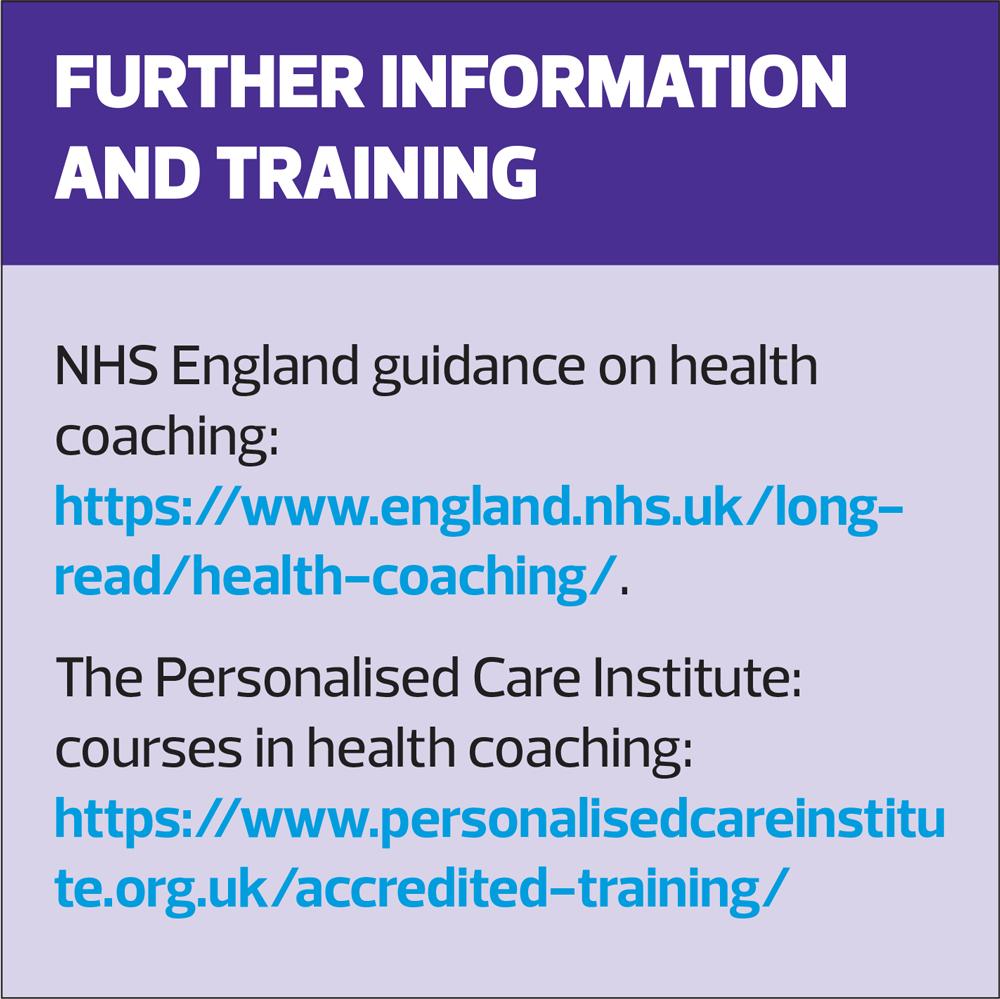
NHS England recommends that adequate resources are provided to ensure health coaching is successful, including training, time and funding. Supervision should be available to people offering health coaching as a way of developing practice and providing an opportunity for reflection and learning. Evaluation of any health coaching service that has been put in place is important to ensure that the anticipated benefits have actually been realised.
With health coaching, it is essential to work with the individual or group to identify the motivation to change. Strong communication skills based on listening, empathy and positivity will be needed by the healthcare practitioner to establish a relationship which enhances self-efficacy. Motivational interviewing is an approach which aims to identify what the person wants to change and then supports them to work out how best to achieve this. One of the fathers of motivational interviewing is William Miller. In a recent article, he described motivational interviewing as an approach which can help people to recognise and utilise what already exists within them, i.e., their own knowledge and strengths.7 Using motivational interviewing techniques, two questions can be asked to assess the individual’s readiness to change and confidence in making changes:
1. On a scale of 1-10, how important is making this change to you, and
2. On a scale of 1-10, how confident are you that you can achieve this change?
Exploration of the scores given and the reasons for those scores can help people to move closer to making individualised choices. Readiness to change is an essential part of health coaching so this should be determined through the use of tools such as the Prochaska and DiClemente change cycle.8 Cognitive behavioural therapy techniques can be used to help reframe behaviours, improve mood and develop a new perspective about changing unhelpful health behaviours.9,10
EXAMPLES OF HEALTH COACHING IN PRACTICE
Health coaching: a one-to-one approach
Helena has type 2 diabetes (T2D) and has struggled to manage this effectively. She finds it hard to make changes to her diet and activity levels and she has been reluctant to take medication. She was offered health coaching with the local coach, who was based in her GP surgery. The coach began by exploring Helena’s thoughts about her diabetes and how important she thought it was to achieve better control. Helena said that she was not too concerned initially as it was ‘only a bit of sugar’ and she had seen family members with T2D who were not overly worried about it either. However, she did flag up the fact that several family members had developed complications from diabetes and said that this did concern her. After discussing T2D with her GPN, however, she has realised that there were things she might do to reduce her risk of complications and her ‘importance’ score had increased from 5 to 8. However, her ‘confidence’ score, based on her ability to make changes, was low at just 2.
The health coach asked her about this score – it wasn’t zero, but it was low (7 is considered to be a ‘good’ score, indicating the likelihood of success) so the coach worked with her to explore her low level of confidence. Helena said that she had tried so many ways to lose weight and although she could lose it, she found it harder to maintain the loss. The health coach reflected back to Helena that she could lose the weight and enquired about how she had done this in the past. Gradually, Helena and the coach developed a plan for improving her diet and activity levels on a budget and they continued to meet as Helena worked her way back to better health. The skills Helena learnt regarding planning her meals and activities and accessing healthy foods at lower cost, has meant that she has now maintained her weight and her diabetes control for three years.
Health coaching – a group approach
In a deprived part of a rural community, people with COPD often turned down pulmonary rehabilitation (PR) referrals because the service was too difficult to access for many of them. In recognition of how effective PR can be, the local health coaching service developed a modified PR programme to be based in the GP surgery. People with COPD who had declined PR were invited to join the surgery group for four 1-hour long sessions on what COPD is, how to manage breathlessness, how to keep their chest clear of sputum, and how to implement lifestyle changes such as healthier eating, physical activity, and smoking cessation to improve their quality of life. Attendees were encouraged to discuss what they wanted from the programme and what their fears and expectations were. Based on these reflections, the coaches were able to tailor the programme to the needs of the group, rather than focussing on ‘educating’ them. People shared their concerns about how the evolution of the condition and how their symptoms might deteriorate. They shared their worries about physical activity making them more breathless and how they felt that this was a sign that it was damaging their health. This group dynamic was a powerful catalyst for discussion around what might help, and which beliefs and preconceptions might be ill-founded. Chair-based exercises were introduced, with short walks around the surgery grounds. Discussions around how to improve nutritional status, through food choices and home food preparation, how to use breathing techniques to improve sputum clearance, and a range of other topics were led by the participants, with input from the coach, rather than the other way around. People linked up with each other to offer support outside of the group. People participating in these sessions reported a stronger sense of being able to look after themselves more effectively, along with lower levels of anxiety about their COPD.
SUMMARY
Health coaching uses behaviour change techniques and motivational interviewing approaches to support greater self-efficacy and improved self-management in a range of long term conditions, and for people at risk of developing these conditions. Specific training is available to develop the skills required to be a health coach, and the principles are appropriate for all members of the healthcare team to follow. There is a strong evidence base for the effectiveness of health coaching, which means that clinicians and others should consider how they can learn and implement health coaching techniques in practice.
REFERENCES
1. Gierisch JM, Hughes JM, Edelman D, et al. The Effectiveness of Health Coaching. Washington (DC): Department of Veterans Affairs (US); 2017. https://www.ncbi.nlm.nih.gov/books/NBK487697/
2. Kivelä K, Elo S, Kyngäs H, Kääriäinen M. The effects of health coaching on adult patients with chronic diseases: a systematic review. Patient Educ Couns 2014;97(2):147–157. https://doi.org/10.1016/j.pec.2014.07.026
3. Fortmann AL, Soriano EC, Gallo LC, et al. (2024). Medical Assistant Health Coaching for Type 2 Diabetes in Primary Care: Results from a Pragmatic Cluster Randomized Controlled Trial. Diabetes Care 2024;47(7):1171–1180. https://doi.org/10.2337/dc23-2487
4. Conn S, Curtain S. Health coaching as a lifestyle medicine process in primary care. Austr J Gen Pract 2019;48(10):677–680. https://doi.org/10.31128/AJGP-07-19-4984
5. Berbert A, Neher J, Safranek S. Do group visits improve HbA1c more than individual visits in patients with T2DM? J Fam Pract 2020;69(1):E21–E22. https://www.mdedge.com/familymedicine/article/216322/diabetes/do-group-visits-improve-hba1c-more-individual-visits-patients
6. Jones T, Darzi A, Egger G, et al. (2019). PROCESS AND SYSTEMS: A systems approach to embedding group consultations in the NHS. Future Healthc J 2019;6(1):8–16. https://doi.org/10.7861/futurehosp.6-1-8
7. Miller WR. The evolution of motivational interviewing. Behav Cognit Psychother 2023;51(6):616–632. https://doi.org/10.1017/S1352465822000431
8. Prochaska JO, DiClemente CC. Stages of change in the modification of problem behaviors. In M. Hersen, R. M.Eisler, & P. M. Miller (eds),Progress in Behavior Modification(pp. 184–212). Sycamore, IL, USA: Sycamore Publishing; 1992.
9. Jenkinson E, Knoop I, Hudson JL, et al. The effectiveness of cognitive behavioural therapy and third-wave cognitive behavioural interventions on diabetes-related distress: A systematic review and meta-analysis. Diabetic Med 2022;39(11): e14948. https://doi.org/10.1111/dme.14948
10. Li Y, Buys N, Ferguson S, et al. The evaluation of cognitive-behavioral therapy-based intervention on type 2 diabetes patients with comorbid metabolic syndrome: a randomized controlled trial. Diabetol Metab Syndr 2023;15(1):158. https://doi.org/10.1186/s13098-023-01100-2