Blackouts: an evidence-based approach
Dr Gerry Morrow
Dr Gerry Morrow
MB ChB, MRCGP, Dip CBT
Medical Director and Editor,
Clarity Informatics Limited
Blackouts are a common problem and making a definitive diagnosis depends on the history and a detailed clinical assessment, and may require expert involvement to rule out serious pathology. Practice nurses are ideally placed to play a key part in the assessment, management and follow-up of affected patients.
DEFINITION AND PREVALENCE OF BLACKOUTS
A blackout is defined as a transient, spontaneous loss of consciousness followed by complete recovery. Blackouts are common. In the UK, 1 in 2 people will experience a blackout at some point in their lives, the most common underlying cause being vasovagal syncope.1
The prevalence of blackouts varies between age groups. A large, population-based cohort study of 2,336 men and 2,873 women aged 40 to 59 years found that blackouts were experienced by 16% and 19% of men and women, respectively.1 The prevalence rises in the elderly, one study of adults aged over 70 years reported a ten-year prevalence of blackouts of up to 25%.2
Approximately 1% of accident and emergency department visits in Europe are thought to be due to blackouts.
One meta-analysis reporting on 43,315 people presenting to emergency departments with syncope found that in 29% diagnosis was situational, orthostatic or vasovagal syncope. Heart disease was diagnosed in 10.4% of people, most frequently bradyarrhythmia (4.8%) and tachyarrhythmia (2.6%). One third of people were discharged without a diagnosis.3
Blackouts are a common presentation in primary care and practice nurses have an integral role in managing these patients.
CAUSES OF BLACKOUTS
Common causes of blackouts include the following illnesses:
- Neurally-mediated reflex syncope, which covers the concepts of vasovagal syncope (fainting), carotid sinus syndrome (which is hypersensitivity of the carotid sinus baroreceptor causing bradycardia and/or vasodilation), and situational syncope (faint with a specific identifiable trigger).4,5
- Orthostatic hypotension – a fall in systolic blood pressure of at least 20 mmHg (at least 30 mmHg in people with hypertension) and/or a fall in diastolic blood pressure of at least 10 mmHg within 3 minutes of standing.
- Cardiac abnormalities including bradycardia, tachycardia, low cardiac output, blood flow obstruction, vasodilatation, or acute vascular dissection.
With all three of these diagnoses the mechanism leading to transient loss of consciousness is temporary inadequacy of cerebral arterial blood flow, most often triggered by a fall in systolic blood pressure.
Epileptic seizures can also cause blackouts. The cause of loss of consciousness in these patients is due to abnormal discharge of cortical neurones.
COMPLICATIONS OF BLACKOUTS
Immediate complications from blackouts include injuries associated with sudden loss of consciousness. Vasovagal syncope and situational syncope are generally associated with a good overall prognosis. Orthostatic hypotension is also generally associated with a good prognosis although the person's long-term prognosis may be affected by some of the possible underlying causes for the condition (such as diabetes or Parkinson's disease).
An underlying cardiac cause for blackout is associated with a poorer prognosis. The 1-year mortality of people with cardiac syncope is greater (18% to 33%) than in people with non-cardiac causes (0% to 12%) or unexplained syncope (6%).3
One-year incidence of sudden death is about 24% for people with a cardiac cause, compared with 3% people with non-cardiac or unexplained syncope.3
The prognosis for a person with epilepsy will vary markedly depending on the person's epilepsy syndrome, frequency of seizures, and response to anti-epileptic drug treatment.6
Assessing a patient who may have had a blackout.
If the person with suspected blackout has sustained an injury or has not fully recovered consciousness, it may be prudent to arrange immediate emergency department assessment. If this is not required, then undertake the following assessment:
- Measurement of vital signs (including pulse rate, respiratory rate, oxygen saturation, and temperature). Repeat these, if this is clinically indicated.
- Lying and standing blood pressure.
- Assessment of other cardiovascular and neurological signs such as cardiac auscultation to detect heart murmurs and assessment for the presence of sensory, motor, speech, and vision deficits.
- If possible perform a 12-lead electrocardiogram (ECG) to assess for cardiac abnormalities, including disturbances of rhythm.
- Measure blood glucose levels, if hypoglycaemia is suspected.
- Take a blood sample for full blood count to check haemoglobin levels, if anaemia or bleeding is suspected.
It is important to take a detailed history and, if possible, ask the person and any witnesses about the details of the event, including the person's posture immediately before loss of consciousness, any prodromal symptoms (such as sweating or feeling warm/hot), their appearance (such as pallor, whether eyes were open or shut), the presence or absence of movement during the event (for example, limb-jerking and its duration), whether there was tongue-biting, whether any injuries occurred during the event , the duration of the event (onset to regaining consciousness), the presence or absence of confusion during the recovery period, or whether they noticed any weakness down one side during the recovery period.
Ask about any previous history including details of any previous blackouts, including number and frequency, their previous medical history and any family history of cardiac disease (including personal history of heart disease and family history of sudden cardiac death), and about their current medication that may have contributed to the blackout (for example, diuretics).
In all patients it is important to exclude the presence of a life-threatening cause for blackout, such as:
- Myocardial infarction and ischaemia. This may be suggested by a history of coronary artery disease (CAD) and preceding chest pain. The ECG may show signs of infarction such as ST-segment elevation, new left bundle branch block, and/or arrhythmia. However, a normal ECG does not exclude CAD. If there is any suggestion clinically that this is CAD, then the patient should be admitted for specialist review.
- Cardiac arrhythmia. This again is suggested by history of CAD, use of medicines that promote atrioventricular block or Torsades de Pointes, and/or history of Wolff-Parkinson-White syndrome, long QT syndrome, or Brugada syndrome. Abnormalities including ventricular arrhythmia (including ventricular ectopic beats) or sustained atrial arrhythmia may be seen on ECG.
- Pulmonary embolism. This diagnosis might be suggested by dizziness, shortness of breath, pleuritic chest pain, the presence of thromboembolic (TE) risk factors, such as previous TE disease, prolonged immobilisation (for example a flight lasting more than 4 hours), smoking, contraceptive pill or HRT use, known malignancy, or family history of thromboembolism. You should be aware that syncope is a relatively common finding in older people with a PE (24% of people aged over 65 years).
- Occult haemorrhage. This might be suggested by recent tissue trauma or signs/symptoms of gastrointestinal bleeding (including haematemesis, and melaena), ruptured aortic aneurysm (suggested by abdominal and sharp tearing back pain), ruptured ovarian cyst, ruptured ectopic pregnancy, retroperitoneal haemorrhage, or a possible ruptured spleen (usually because of trauma but can be spontaneous for example after glandular fever).
- Aortic dissection. This can be suggested by chest and sharp, tearing back pain. In these patients the ECG may be abnormal if the dissection involves the coronary vessels.
- Cardiac tamponade. This is suggested by a combination of low arterial blood pressure, distended neck veins, and distant, muffled heart sounds (Beck's triad). Symptoms include dyspnoea, tachypnoea, tachycardia, anxiety, restlessness, weakness, chest pain radiating to the neck, shoulders, or back, and discomfort that is relieved by sitting or leaning forward.
- Severe hypoglycaemia. This is suggested by confusion, anxiety, somnolence, palpitations, and lethargy. This diagnosis can be due to excessive administration of insulin in a patient with diabetes, hepatic disease, or an islet of Langerhans tumour.
- Addisonian crisis. This rare event should be suspected in people with Addison's disease. Symptoms can include nausea, vomiting, fever, hypotension, hyperpigmentation, and electrolyte abnormalities.
MAKING A DEFINITIVE DIAGNOSIS
To move to a definitive diagnosis in a patient with a blackout we can be more confident if we can find a grouping of signs or symptoms for each possible cause.
Suspect a possible underlying cardiac cause
If there is:
- An ECG abnormality, such as conduction abnormality (for example, complete right or left bundle branch block or any degree of heart block), evidence of a long (corrected QT > 450 ms) or short (corrected QT < 350 ms) QT interval, any ST segment or T wave abnormalities, inappropriate persistent bradycardia, ventricular arrhythmia (including ventricular ectopic beats), Brugada syndrome, ventricular pre-excitation (part of Wolff-Parkinson-White syndrome), left or right ventricular hypertrophy, pathological Q waves, atrial arrhythmia (sustained), paced rhythm.
- There is a blackout occurring during exertion. However, note that blackouts that are exercise-induced but occur shortly after stopping exercise rather than during exercise, may be vasovagal in origin
- Palpitations before the loss of consciousness occurs
- There is a family history of sudden cardiac death in people aged younger than 40 years and/or an inherited cardiac condition
- New or unexplained breathlessness
- The presence of a heart murmur
- A blackout in the absence of any prodromal symptoms in people aged older than 65 years.
Suspect epilepsy as an underlying cause
If there are any of the following:
- Prodromal déjà vu, or jamais vu
- A bitten tongue
- Head-turning to one side during the blackout
- Loss of bowel and bladder control
- Unusual posturing
- Prolonged limb-jerking
- Confusion following the event.
Suspect an uncomplicated vasovagal syncope (faint)
If there is:
- An absence of features to suggest an alternative diagnosis (note: brief seizure activity can occur during uncomplicated faints and is not necessarily diagnostic of epilepsy) and
- The presence of features suggestive of uncomplicated faint (the 3 'P's):
— Posture – blackout occurred after prolonged standing. Similar episodes may have been prevented by lying down.
— Provoking factors – such as pain or a medical procedure.
— Prodromal symptoms – such as sweating or feeling warm/hot before the blackout occurred.
Suspect situational syncope
If there are no features to suggest an alternative diagnosis, and:
- Syncope is clearly and consistently provoked by straining during micturition (usually while standing), defecation, or by coughing or swallowing.
- Suspect carotid sinus syndrome if the blackout(s) occurred while turning the head to one side, particularly in men aged 50 years or older.
Suspect orthostatic hypotension
If there is an absence of features suggesting an alternative diagnosis, and:
- A typical history – light-headedness, dizziness, weakness, tunnel vision. Symptoms should not occur while supine, should get worse on standing, and should be relieved by sitting or lying down. Symptoms are often worse early in the morning, in hot environments, after meals, after standing motionless, and after exercise.
- If the above criteria are met, measure lying and standing blood pressure (with repeated measurements while standing for 3 minutes). A fall in systolic blood pressure of at least 20 mmHg (at least 30 mmHg in people with hypertension) and/or a fall in diastolic blood pressure of at least 10 mmHg within 3 minutes of standing confirms the diagnosis.
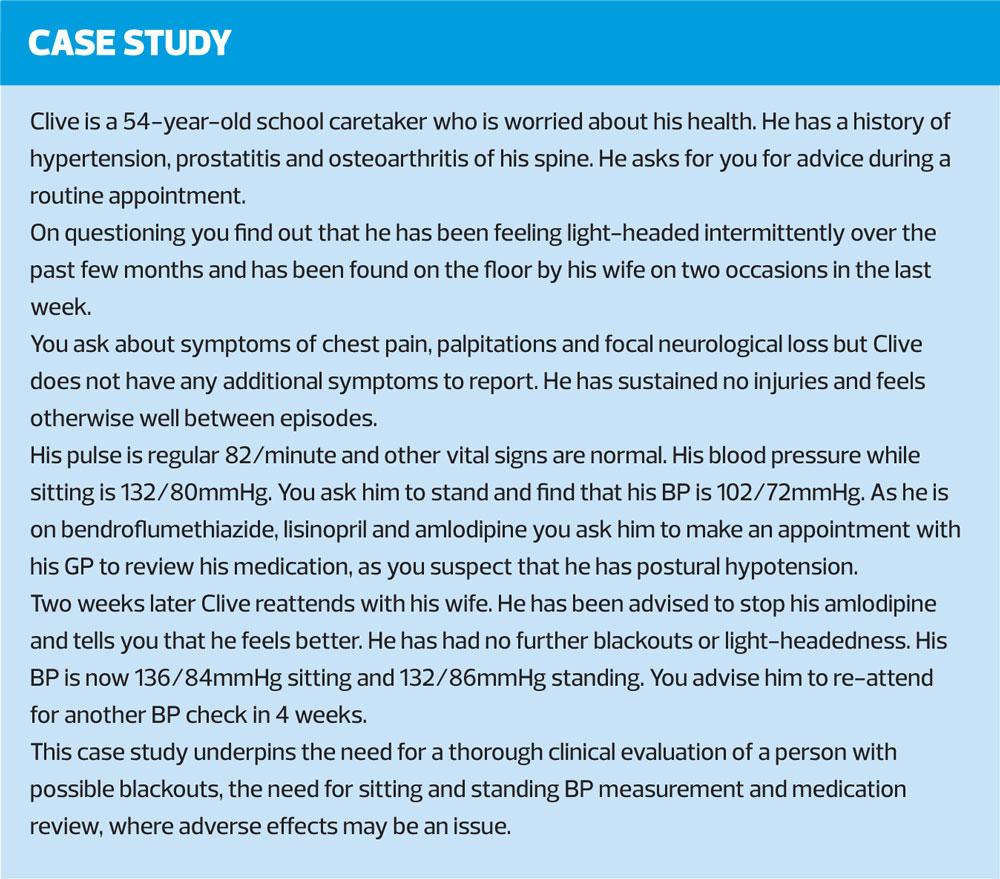
Note: potential underlying causes for orthostatic hypotension include treatment with alpha-blockers, diuretics, tricyclic antidepressants, antihypertensives (particularly diuretics), levodopa or dopaminergic agonists, volume depletion, physical deconditioning due to prolonged bed rest, diseases causing peripheral neuropathy (such as diabetes mellitus), Parkinson's disease, or Lewy body dementia.
Polypharmacy with antihypertensive and antidepressant medicines is often the cause of orthostatic hypotension in older people.
MANAGEMENT AND REFERRAL STRATEGY9
If the person with blackout has sustained an injury, has not fully recovered consciousness, or an immediately life-threatening underlying cause is suspected, use clinical judgement to determine appropriate initial management and the urgency of specialist follow-up. If required, arrange urgent admission to hospital, via ambulance if necessary.
For all people experiencing blackouts being initially managed in primary care, practice nurses are ideally placed to provide a risk assessment. This assessment should begin with a discussion the possible causes of their blackouts, results of tests they have had, reasons for any further investigations they are offered, and the nature and extent of uncertainty in the diagnosis.
Additionally, you should advise all people who have experienced a blackout that they must not drive while waiting for a specialist assessment. Depending on the outcome of the specialist assessment, advise that the person may then be obliged to report the event to the Driver and Vehicle Licensing Agency (DVLA). For more information, see Assessing fitness to drive: a guide for medical professionals at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/736938/assessing-fitness-to-drive-a-guide-for-medical-professionals.pdf.
Advise people experiencing blackouts that they may need to report this to their employer as there may be implications for health and safety at work.
If there are clinical features suggestive of an underlying cardiovascular cause (which does not require immediate hospitalisation) refer urgently for a cardiovascular assessment. Also consider referring anyone aged older than 65 years who has experienced a blackout without prodromal symptoms for cardiovascular assessment.
People in whom psychogenic non-epileptic seizures or psychogenic pseudosyncope are suspected as differential diagnoses should be referred for neurological assessment as the distinction between epilepsy and non-epileptic seizures can be complex.
If uncomplicated vasovagal syncope or situational syncope are suspected as the underlying cause for blackout, and there are no features to raise clinical or social concerns then you should arrange an ECG and its interpretation within 3 days if this has not yet been recorded.
Explain the mechanisms causing the syncope. A helpful patient information leaflet on fainting is available from NHS Choices, at https://www.nhs.uk/conditions/fainting/.
Advise on possible trigger events, and strategies for avoiding them. If the trigger events are unclear, advise the person to keep a record of their symptoms, when they occur and what they were doing at the time, to understand what causes them to faint and reassure them that their prognosis is good.
Practice nurse expertise here is invaluable in providing patient education and encouraging patients to capture information in a ‘diary of events’ format.
Advise them to seek primary care follow-up if they experience further blackouts, particularly if these differ from any recent episodes.
For people with suspected vasovagal syncope with recurrent episodes of blackout adversely affecting their quality of life, or representing a high risk of injury, consider offering referral for a tilt test to assess whether the syncope is accompanied by a severe cardioinhibitory response (usually asystole).
For people with suspected carotid sinus syndrome and for people with unexplained syncope who are aged 60 years or older, offer cardiology referral for carotid sinus massage as a first-line investigation.
For all people with unexplained syncope (including after negative carotid sinus massage test in those for whom this is appropriate), offer ambulatory ECG. Specialist referral may then be indicated depending on the results of this investigation and/or if there is still uncertainty regarding the underlying cause.
For all people with a history suggestive of orthostatic hypotension in whom the diagnosis was not confirmed by differences in lying and standing blood pressure, refer for specialist cardiovascular assessment.
For people in whom orthostatic hypotension is confirmed as the diagnosis you should consider the likely causes, review any drug therapy, and eliminate any potentially causative drugs where possible. Explain the mechanisms causing the blackouts and provide written patient information which is available from the Newcastle upon Tyne Hospitals Falls and Syncope service10.
All practice nurses have a pivotal role in advising the person of simple lifestyle changes that can lessen symptoms of orthostatic hypotension. These changes can include, first sitting when going from a supine to a standing position, eating frequent, small meals, liberalising dietary salt intake (unless they have been diagnosed with hypertension), drinking at least 2 litres of water a day, avoiding alcohol, tilting the head of the bed up during the night, and avoiding straining during bowel movements.
Advise the person to seek further practice nurse or GP follow-up if their symptoms do not improve with the above measures.
Conclusion
Blackouts are common and problematic for patients. Making a definitive diagnosis depends on a clear history of the event and a detailed clinical assessment. Patients who suffer blackouts may require expert involvement to rule out a serious cardiac or neurological pathology for their loss of consciousness. Practice nurses are ideally placed to be a key part of these patients’ assessment, management and follow-up.
REFERENCES
1. Savage DD, Corwin L, McGee DL, et al. Epidemiologic features of isolated syncope: the Framingham Study. Stroke 1985;16(4):626-629.
2. Lipsitz LA, Wei JY, Rowe JW. Syncope in an elderly, institutionalised population: prevalence, incidence, and associated risk. Q J Med 1985;55(216):45-54.
3. D'Ascenzo F, Biondi-Zoccai G, Reed MJ, et al. Incidence, aetiology and predictors of adverse outcomes in 43,315 patients presenting to the Emergency Department with syncope: an international meta-analysis. Int J Cardiol 2013; 167(1):57-62
4. BMJ Best Practice. Assessment of syncope, 2018. BMJ Publishing Group.
5. BMJ Best Practice. Neurally mediated reflex syncope, 2018. BMJ Publishing Group.
6. Elger CE, Schmidt D. Modern management of epilepsy: a practical approach. Epilepsy & Behavior 2008;12(4):501-539.
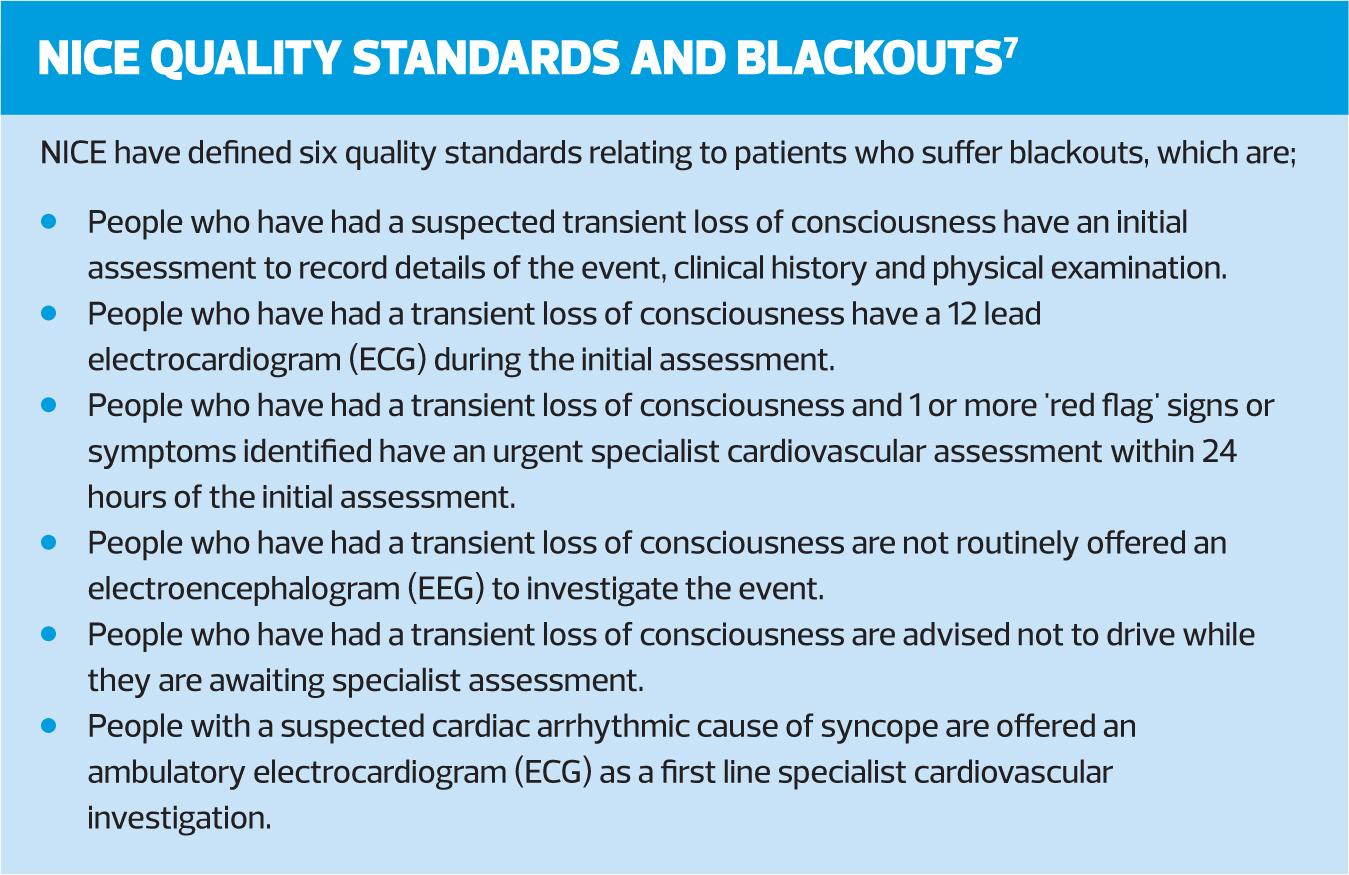
7. NICE QS71. Transient loss of consciousness (‘blackouts’) in over 16’s. Quality Standard 71, October 2014 https://www.nice.org.uk/guidance/qs71/chapter/List-of-quality-statements
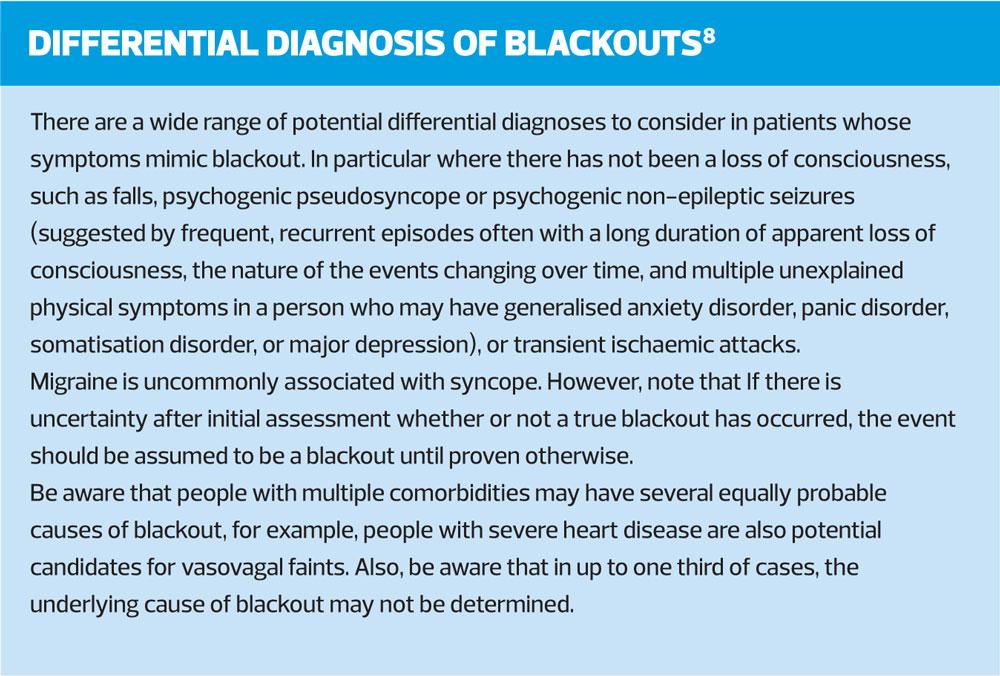
8. NICE Clinical Evidence. Clinical Knowledge Summaries. Blackouts, 2019 https://cks.nice.org.uk/
9. Fitzpatrick AP, Cooper P. Diagnosis and management of patients with blackouts. Heart 2006;92(4):559-68.
10. Newcastle upon Tyne Hospitals Trust Falls and Syncope Service. Orthostatic Hypotension, 2018. http://www.newcastle-hospitals.org.uk/services/care-of-the-elderly_treatment-and-medication_orthostatic-hypotension.aspx