Multimorbidity: implications for general practice nurses
DR GERRY MORROW
DR GERRY MORROW
MB ChB, MRCGP, Dip CBT
Medical Director and Editor, Clarity Informatics Limited
Multimorbidity is becoming an increasing problem for the NHS as a whole and general practice in particular, contributing to escalating demand for services and workload. This article, based on the highly respected Clinical Knowledge Summaries module, offers some insights
Multimorbidity is an increasingly problematic issue for healthcare delivery and healthcare professionals. People with multimorbidity are more likely to attend and require health and social care assistance more frequently, especially unplanned admissions to hospital, iatrogenic problems from polypharmacy and are at risk of premature death.
The burden of care for these individuals is significant across primary, secondary and community care.
Multimorbidity is defined as a person having two or more long-term health conditions.
These could include:
- Physical or mental health conditions, such as diabetes or schizophrenia.
- Ongoing conditions, such as a learning disability.
- Symptom complexes, such as frailty or chronic pain.
- Sensory impairment, such as sight or hearing loss.
- Alcohol or substance misuse.
Multimorbidity is surprisingly common. In 2018 a retrospective cohort study in England the prevalence of multimorbidity was 27.2%.1
The authors of this study found that prevalence increases significantly with age. Half of the people identified had acquired at least one significant health condition by age 50 and by age 65 most were multimorbid.
Females have a higher prevalence of 30%, compared with 24% for males. A third (34%) of people affected had both a physical and mental morbidity.
Younger people with multimorbidity, that is those aged 18–24 years, were more likely to have a physical–mental comorbidity (56.5%), compared with 23.7% of people aged 75–84 years.
The proportion of people with multimorbidity who had a physical–mental comorbidity increased substantially with greater socioeconomic deprivation. It is also clear that the onset of multimorbidity occurred 10-15 years earlier in people in areas of socioeconomic deprivation.1
With an ageing population, multimorbidity is likely to become more common and an increasing problem for the whole healthcare economy.
- Increasing age.
- Female sex.
- Lower socioeconomic status.
- Pre-existing medical conditions (for example, hypertension, osteoporosis).
- Tobacco and alcohol use.
- Lack of physical activity.
- Poor nutrition and obesity.
THE PROBLEM OF MULTIMORBIDITY
Multimorbidity has a highly significant effect on a person’s quality of life and life expectancy.
The reasons for this include firstly a high ‘treatment burden’. This means that the inherent difficulties of understanding and self-managing conditions, juggling multiple appointments with different healthcare specialists, managing complex drug regimens and adhering to radically altered lifestyle changes can result in conflict, fragmentation of care and ultimately failure in compliance with treatment.
In addition to this, issues with anxiety and depression are more common in people with multimorbidity, which can have an adverse impact on their ability to manage their conditions.
It is also important to note that people with cognitive impairment are particularly vulnerable and may have added difficulties in managing their conditions.
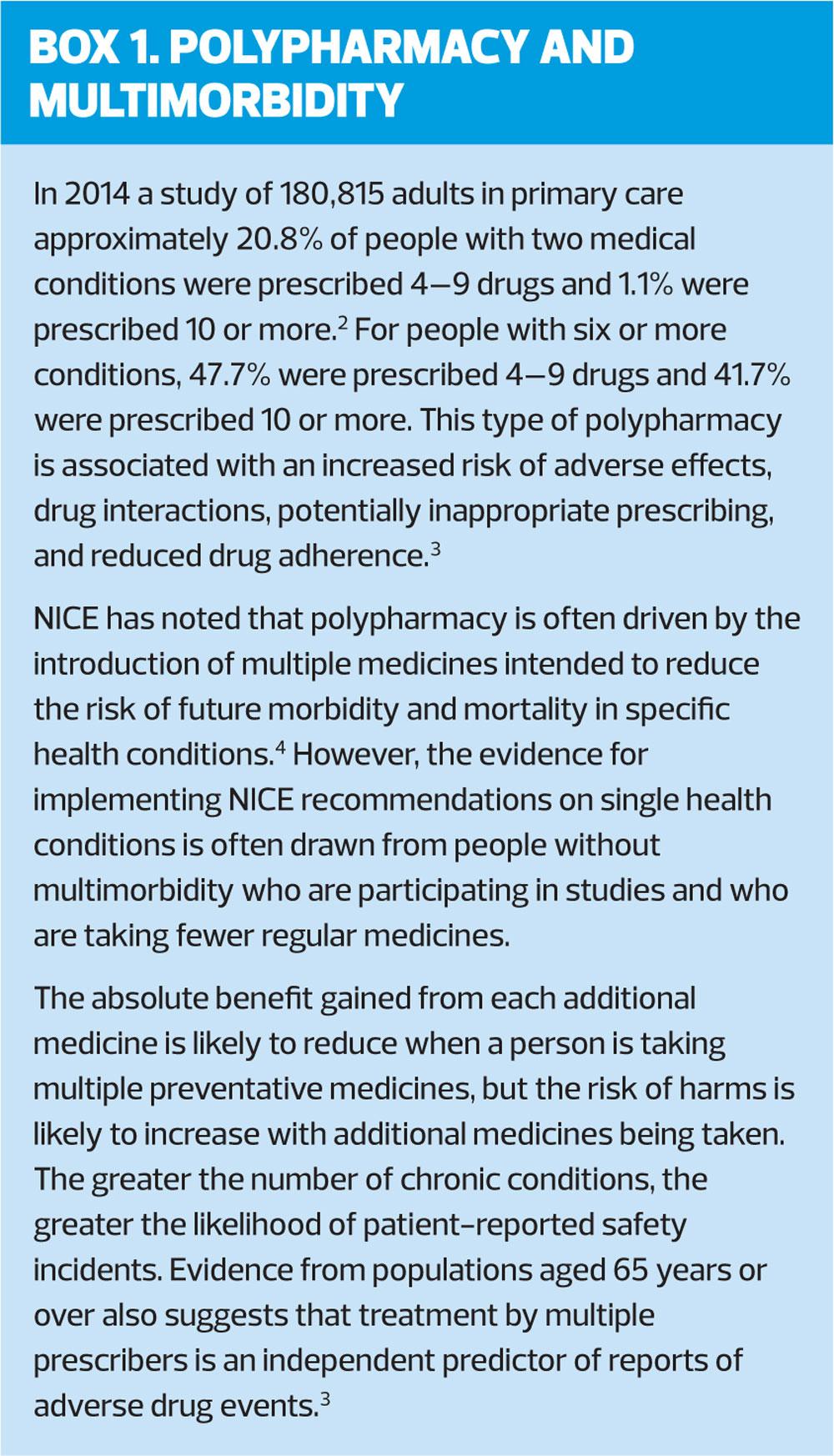
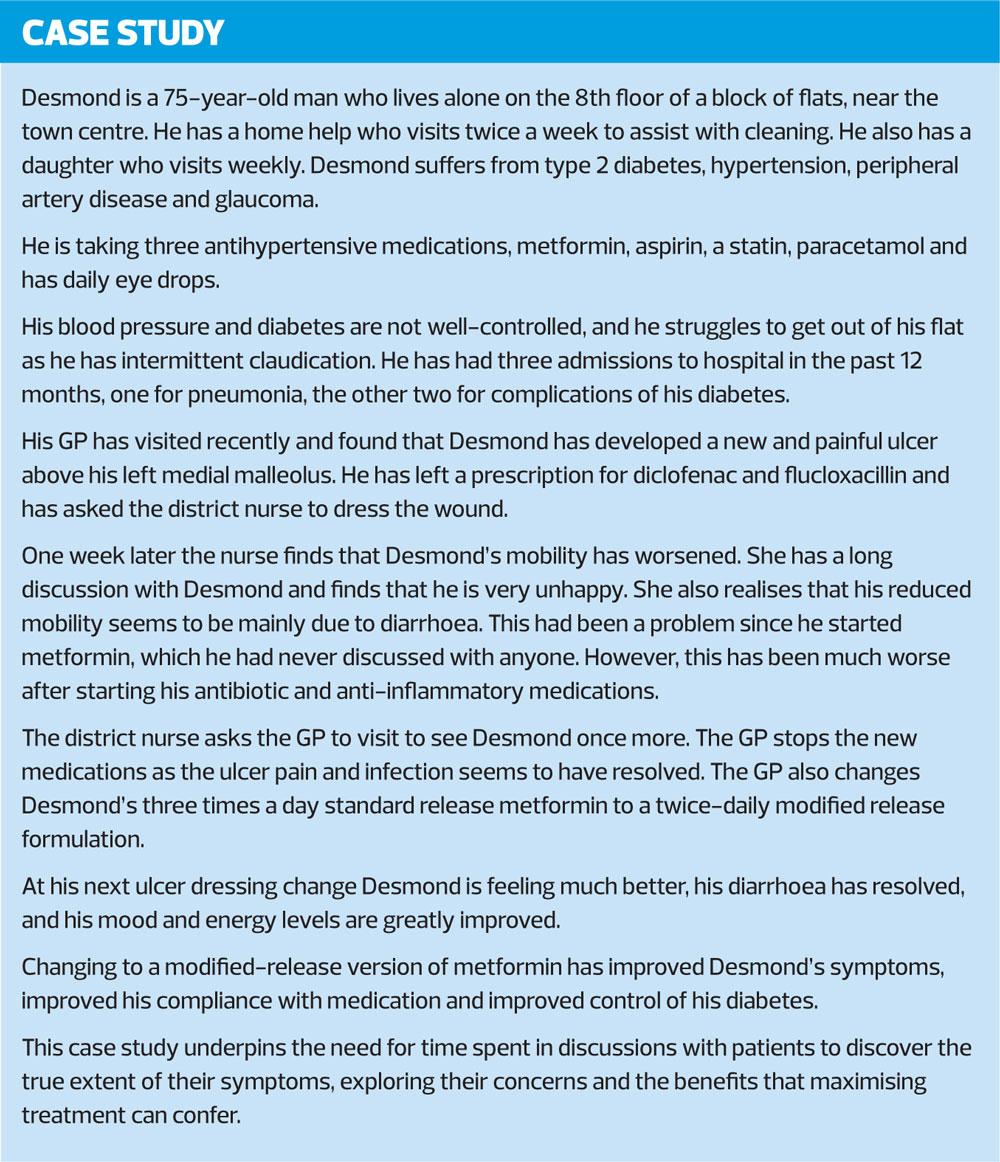
Also, polypharmacy in these individuals and the inevitable higher rates of adverse drug events are an ever-present danger. (Box 1) These risks are higher again in people who are older (particularly those with renal impairment), disabled, or people with mental health conditions. This can impose further constraints on self-care and adherence to treatment.
All this inevitably imposes an increased use of health services (including unplanned, or emergency care).
Finally, multimorbidity also has a negative impact on the health and wellbeing of carers.
ASSESSMENT
The management of people with multimorbidity is therefore an increasingly essential component of the toolbox of skills required by all healthcare professionals. The principles involved in caring for those with multimorbidity or are at risk of developing multimorbidity include an assessment of their condition and a ‘shared care approach’ to comprehensive overview of their disease burden.
Firstly, we should identify people who may benefit from an approach to care that takes account of multimorbidity, this could be done either opportunistically during routine care or proactively using healthcare records, for example, assessing the number of regular medicines a person is prescribed.
Specifically, it will be possible to identify from medication records those people taking 10 or more regular medicines or are prescribed fewer than 10 regular medicines but are at risk of adverse events.
Secondly, we should consider that people may need a multimorbidity approach, if:
- They find it difficult to manage their treatments or day-to-day activities, or
- Receive care and support from multiple services and need additional services, or
- Have both long-term physical and mental health conditions, or
- Have frailty or are at risk of falls, or
- Frequently seek unplanned or emergency care
To assist with a comprehensive risk assessment, we should consider using a validated tool. These include Electronic Frailty Index (eFI), Predicting Emergency Admissions Over the Next Year (PEONY) or QAdmissions to identify adults with multimorbidity who are at risk of adverse events, such as unplanned hospital admission or admission to care homes.
These tools provide prompts and questions enabling users to employ an evidence-based approach to assess and quantify multimorbidity emergency admission risk for individuals.
How to assess a person with multimorbidity or at risk of multimorbidity
Establish the extent of the disease burden. Specifically, ask how the health problems affect their day-to-day life, this should include a discussion of the following areas;
- Mental health issues, including anxiety and depression
- How disease burden affects their wellbeing?
- How their health problems interact and how this affects quality of life?
Establish the extent of the treatment burden. Specifically, ask how treatments affect their day-to-day life. Consider including questions about
- The number and type of healthcare appointments and where these take place?
- The number and type of medicines they take and how often they experience harms from medicines?
- Their use of non-pharmacological treatments such as diets, exercise programmes and psychological treatments?
- Any effects of treatment on their mental health or wellbeing?
Explore the person's attitudes to their treatments and the potential benefits and harms of those treatments. Follow shared care principles when making decisions about medicines and take into account your understanding of the person's knowledge, beliefs and concerns about medicines.
Also ask about, and consider:
- Their social circumstances, financial constraints, living conditions and social support
- Their health ‘literacy’ and their ability to comprehend treatment regimens
- Their functional autonomy and ability to perform independent tasks of daily living
- Assessing their potential coping strategies
- The possibility of depression and anxiety. It is key to consider identifying these conditions including an assessment of any suicidal ideation
- The presence of chronic pain and the adequacy of current pain management.
Encourage people with multimorbidity to clarify what is important to them, including their personal priorities, which may include:
- Maintaining their independence
- Participating in family life, work or upcoming social activities
- Preventing specific adverse outcomes
- Reducing any treatment burden.
- Improving the quality and length of their life
- Pain and symptom relief, including any palliative care needs.
This is clearly a long list of questions, considerations and detailed inquiry for a single health professional to undertake. It may therefore form part of an overall care plan, over multiple appointments across a multidisciplinary team.
FRAILTY
Frailty is defined as a ‘clinically recognizable state of increased vulnerability resulting from aging-associated decline in reserve and function across multiple physiologic systems such that the ability to cope with every day or acute stressors is comprised’.5
Frailty is an essential consideration to be aware of in people with multimorbidity.
When assessing frailty, consider using one of the following:
- An informal assessment of gait speed (for example, time taken to answer the door, time taken to walk from the waiting room).
- A formal assessment of gait speed. Taking more than 5 seconds to walk 4 metres indicates frailty.
- Self-reported health status. Ask the person how they would rate their health on a scale of 0–10. A score of 6 or less indicates frailty.
- The PRISMA-7 questionnaire. Three or more positive responses to the following questions suggests the need for further clinical review.6
1. Are you more than 85 years old?
2. Are you male?
3. In general, do you have any health problems that require you to limit your activities?
4. Do you need someone to help you on a regular basis?
5. In general, do you have any health problems that require you to stay at home?
6. If you need help, can you count on someone close to you?
7. Do you regularly use a stick, walker or wheelchair to get about?
It is important to note that we should cautious about assessing frailty in people who are acutely unwell and that we should not use a physical performance tool to assess frailty in people who are acutely unwell.
MANAGEMENT OF MULTIMORBIDITY
An approach that takes explicit account of multimorbidity is not always required. However, as the complexity or impact of multiple conditions increases, or as the complexity of treatment or care increases, so does the need for management strategies which take specific account of multimorbidity.7
When taking a multimorbidity approach, we should focus on how the person's health conditions and their treatments interact and how this affects quality of life. We need to be cognisant of the person's individual needs, preferences for treatments, health priorities, lifestyle and goals.
When dealing with single health conditions we should take into account the benefits and risks of following guidance and recommendations for these conditions. We should aim to improve quality of life by reducing treatment burden, adverse events, and unplanned care. A useful precept is ‘adding life to years rather than solely adding years to life’.
We should strive to improve coordination of care across services. The lack of which, is often criticised when adverse events occur in healthcare.
We should always discuss the purpose of a multimorbidity approach with the person. This might include reducing the treatment burden and optimising care and support by identifying:
- Ways of maximising benefit from existing treatments
- Treatments which could be stopped because of limited benefit. (For example, a person who has been taking bisphosphonate for osteoporosis for at least 3 years should be told that there is no consistent evidence of further benefit from continuing a bisphosphonate for another 3 years, or harms from stopping a bisphosphonate after 3 years of treatment. We should therefore discuss stopping bisphosphonate after 3 years and include patient choice, fracture risk and life expectancy in the discussion.)
- Treatments and follow-up arrangements with a high treatment burden
- Alternative arrangements for follow-up to coordinate or aim to optimise the number of appointments
- Ways of reducing or stopping medicines with a higher risk of adverse events (for example, falls, gastrointestinal bleeding, or acute kidney injury)
- Identifying simple non-pharmacological treatments as possible alternatives to some medicines
- Consider using a screening tool (for example, the STOPP START tool in older people) to identify medicine-related safety concerns and medicines the person might benefit from but is not currently taking
- Plan a review to monitor the effects of any treatment changes and to decide whether further changes are required, including potentially restarting treatment.
- Discuss with people who have a limited life expectancy or frailty if they wish to continue treatments recommended in guidance on single health conditions that may offer them limited overall benefit.
Develop and agree an individualised management plan with the person, which should include:
- What will be recorded and actions which will be taken
- Goals and plans for future care (including advance care planning)
- Starting, stopping or changing medicines and non-pharmacological treatments
- Prioritising healthcare appointments
- Anticipating possible changes to health and wellbeing
Assigning responsibility for coordination of care and ensuring this is communicated to other healthcare professionals and services.
- Other areas the person considers important to them
- Timing of follow-up and how to access urgent care
- Consider self-management where appropriate depending on the person's preferences
- Share copies of the management plan in an accessible format with the person and (with their permission) other people involved in care.
- Provide instructions for safety-netting, such as symptoms of adverse effects and recommendations about the appropriate management
- Clarify whether, and how, they would like their partner, family members and/or carers to be involved in key decisions about the management of their conditions and review this regularly
- If applicable, consider preferences of informal caregivers or family.
Once more this is an exhaustive list of considerations and detailed inquires for a single health professional to undertake. It should therefore form part of an overall care plan, over multiple appointments across a multidisciplinary team.
The need for self-management of multimorbidity
The World Health Organization (WHO) suggests that prioritising care coordination and self-management support is a strategy which helps address safer care for people with multimorbidity.8
They suggest that this should include promoting self-management to help people with multiple conditions take responsibility for their well-being and safety; implementing education and engagement strategies for people with multimorbidity; and supporting informal caregivers, such as friends, carers and family.
THE IMPORTANCE OF INFORMATION AND ADVICE
When managing someone with multimorbidity we should provide appropriate lifestyle advice depending on their morbidities. For example, for people with cardiovascular disease this should include increasing exercise, healthy eating, smoking cessation, and reducing alcohol intake.
We should also explain when and why they should return for follow-up appointments, describe circumstances in which they should make an appointment out with these intervals, and provide written information and signpost to additional sources of information. (See Resources)
THE IMPORTANCE OF FOLLOW UP
Follow up intervals for people with multimorbidity should be determined using clinical judgement and agreed with the person in the management plan. This should consider their individual circumstances, the range of morbidities and treatments and risk of unplanned admissions and other risks.
Follow up should include:
- An evaluation of progress in achieving the person's priorities.
- A review to monitor the effects of any changes made.
- A decision on whether any further changes to treatment are needed (including restarting a treatment).
It is important for medications to be reviewed regularly to ensure that essential laboratory tests are undertaken, side effects are detected, patients are given essential information and are involved in decisions about their medicines, and that therapy is optimised.3
Specifically, the NICE guideline Older people with social care needs and multiple long-term conditions recommends that care plans should be reviewed and updated regularly, and at least annually, to recognise the changing needs associated with multiple long-term conditions. 9–11
CONCLUSION
A person living two or more long-term health conditions has multimorbidity. Almost 30% of UK adults are living with multimorbidity, and this increases with age and socioeconomic deprivation.
Multimorbidity is associated with an increased burden on all areas of healthcare provision but importantly reduces both quality of life and life expectancy for the individual affected.
Management of the condition is focussed on identification of those at risk, detailed assessment to minimise disease and treatment burdens.
REFERENCES
1. Cassell A, Edwards D, Harshfield A, et al. The epidemiology of multimorbidity in primary care: a retrospective cohort study. B J Gen Pract 12 March 2018; https://bjgp.org/content/early/2018/03/12/bjgp18X695465
2. Payne, R.A. and et al. Prevalence of polypharmacy in a Scottish primary care population. Eur J Clin Pharmacol 2014;70(5):575-581. https://link.springer.com/article/10.1007%2Fs00228-013-1639-9
3. Duerden M, Avery T, Payne R. Polypharmacy and medicines optimisation: making it safe and sound. The King's Fund, 2013. https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/polypharmacy-and-medicines-optimisation-kingsfund-nov13.pdf
4. NICE KTT18. Multimorbidity and polypharmacy, Key therapeutic topic (KTT) 2017. https://www.nice.org.uk/advice/ktt18
5. Xue Q-L. The Frailty Syndrome: Definition and Natural History. Clin Geriatr Med 2011;27(1):1-15. doi: 10.1016/j.cger.2010.08.009.
6. Raiche M, Hebert R, and Dubois MF. (2008) PRISMA-7: a case-finding tool to identify older adults with moderate to severe disabilities. Arch Gerontol Geriatr 2008;47(1):9-18
7. Academy of Medical Sciences. Multimorbidity: a priority for global health research, 2018. https://acmedsci.ac.uk/file-download/99630838
8. WHO. Multimorbidity: technical series on safer primary care, 2016. http://www.who.int/patientsafety/topics/primary-care/technical_series/en/
9. NICE NG22. Older people with social care needs and multiple long-term conditions, 2015 https://www.nice.org.uk/guidance/ng22
10. NICE Clinical Evidence, Clinical Knowledge Summaries: Multimorbidity, 2018 https://cks.nice.org.uk/multimorbidity
11. NICE NG56. Multimorbidity: clinical assessment and management, 2016. https://www.nice.org.uk/guidance/ng56
Related articles
View all Articles