Prioritising workload during the pandemic
Helene Irvine
Helene Irvine
Practice Nurse Adviser, Wessex LMCs
Deputy Clinical Lead, RCGP Primary Care Development
Julia Taylor
Advanced Clinical Practitioner/GP Trainer
Clinical Lead for General Practice, Advanced Practice Strategy Group, Derbyshire
It has been said that general practice has been transformed more dramatically in the past few weeks than in the previous decade, but the rapid pace of change may leave some nurses in doubt about what they should – and should not – be doing
For some years general practice nurses have been shouting about the important and essential role that they have, which they feel often gets overlooked, taken for granted or misunderstood. Recognising the capabilities of nurses, and the level of practice that nurses work to in primary care will help in making it an attractive career option. The recruitment, training and support processes within primary care need to be improved to attract nurses into general practice and replace many of the current nurses who are approaching retirement age.
Nurses are now working differently, increasingly taking on a variety of roles that may not have been seen as a traditional role for all GPNs, including triage, video consultations and home visiting. The important and essential role that they have, which they feel often gets overlooked, taken for granted or misunderstood. Recognising the capabilities of nurses, and the level of practice that nurses work to in primary care will help in making it an attractive career option. The recruitment, training and support processes within primary care need to be improved to attract nurses into general practice and replace many of the current nurses who are approaching retirement age. Nurses are now working differently, increasingly taking on a variety of roles that may not have been seen as a traditional role for all GPNs, including triage, video consultations and home visiting. The impact on staff, workload and patient care will need to be reviewed, understood and learned from to understand which successes can be taken forward.
WHAT HAS HAPPENED?
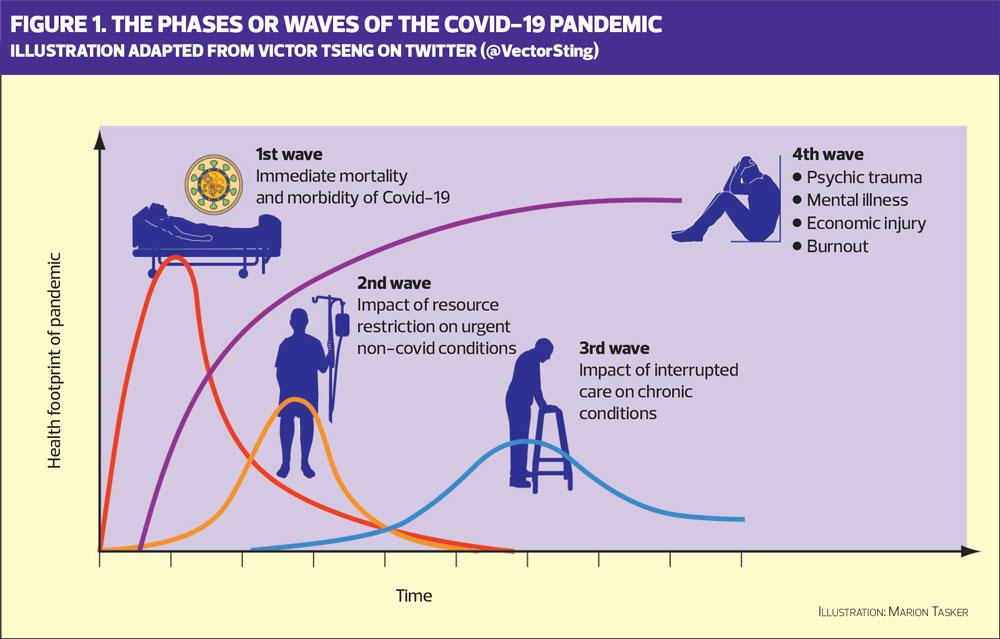
Nationally and regionally the focus has been on patient safety, ensuring patients receive the best possible care, support and advice. The challenge has been managing demand by balancing workload and workforce, including recruiting GP and nurse returners. The aim was to try and reduce the demand on hospitals to enable them to manage the increased capacity created by COVID-19. In a recent Tweet by Canadian doctor, Victor Tseng, this is referred to as stage 1 of the COVID-19 pandemic, illustrated in Figure 1.
Some people have been reluctant to access care as they do not want to over burden an already overstretched system but also for fear of being exposed to coronavirus. However, patients who need support for potentially significant symptoms should be able to access services appropriately. Anecdotal evidence would suggest that by the end of April, however, there has been an increasing number of patients contacting practices for advice other than for COVID-19. The knowledge, skills and experience of the nursing workforce should be used effectively and appropriately to meet this need.
WHAT HAVE WE LEARNED?
One of the positives is that patients appear to have been taking responsibility for their own health and this should be encouraged. Working closely with the new roles identified in the New GP contract such as link workers, health coaches and social prescribers will be essential to adopt the concept of person-centred care with the emphasis on wellbeing, care, prevention and support.
Nurses have expressed the view that one of the major positives to come out of the pandemic has been the improved communication and close working within their practice teams and other community staff, especially district nurses. This improved communication needs to be both maintained and developed. It will be interesting to see how this impacts on roles, competencies, the further development of integrated teams and breaking down of traditional boundaries. The focus is likely to be not on where the patient is seen but who is best placed to deliver the care.
WHAT NURSES CAN DO NOW?
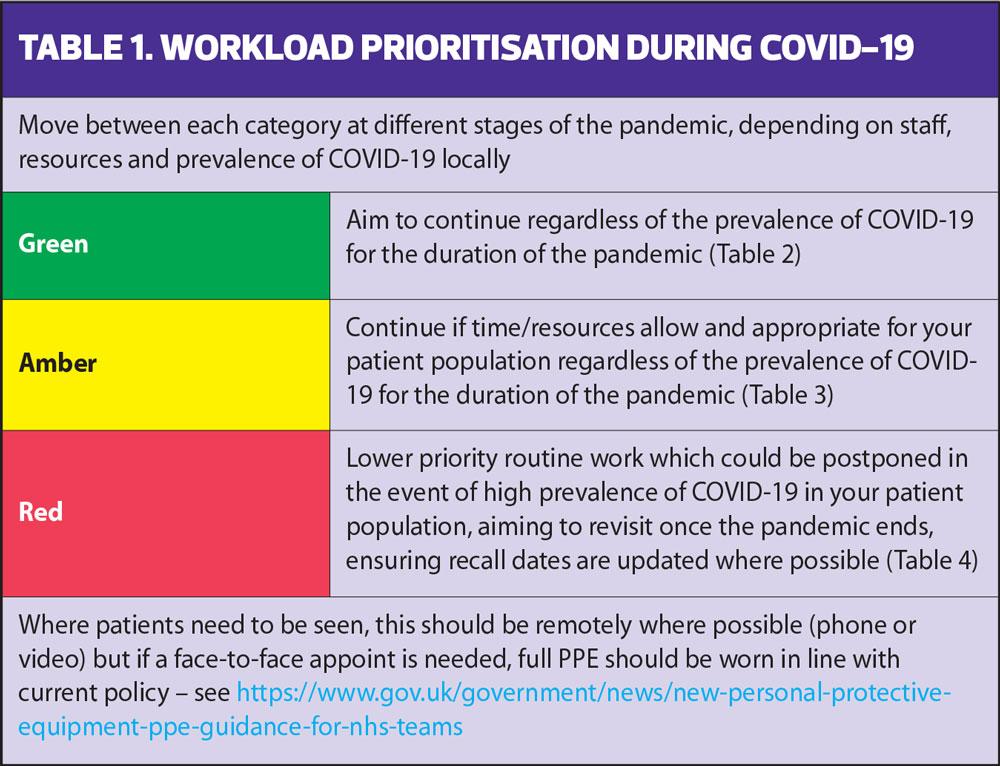
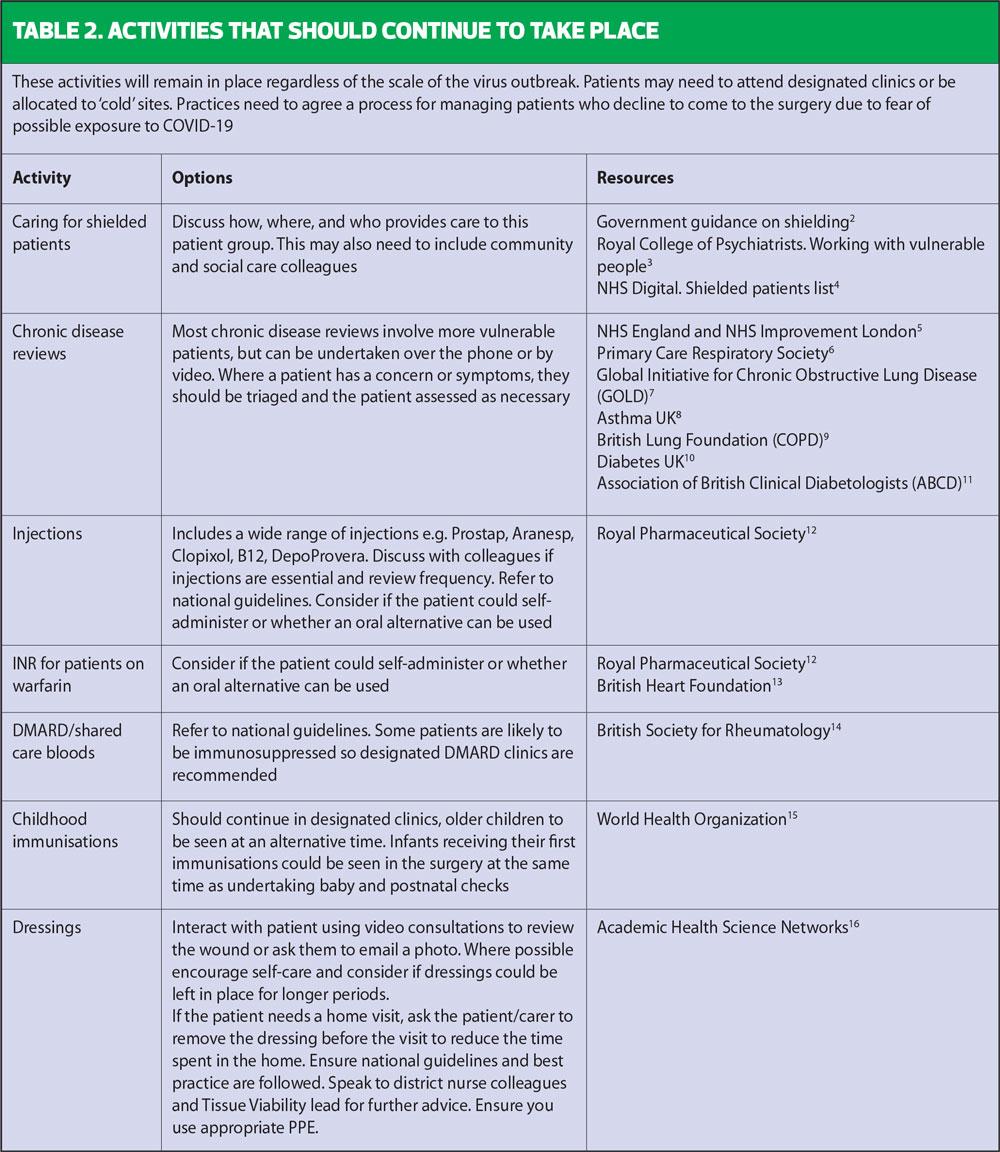
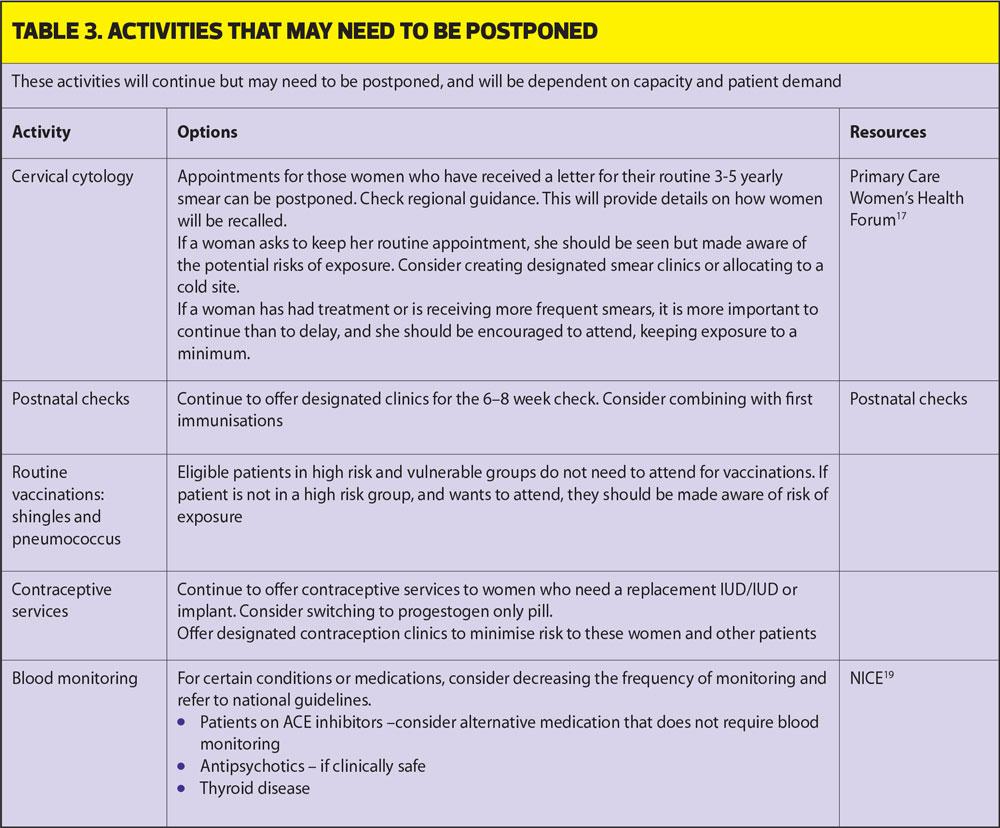
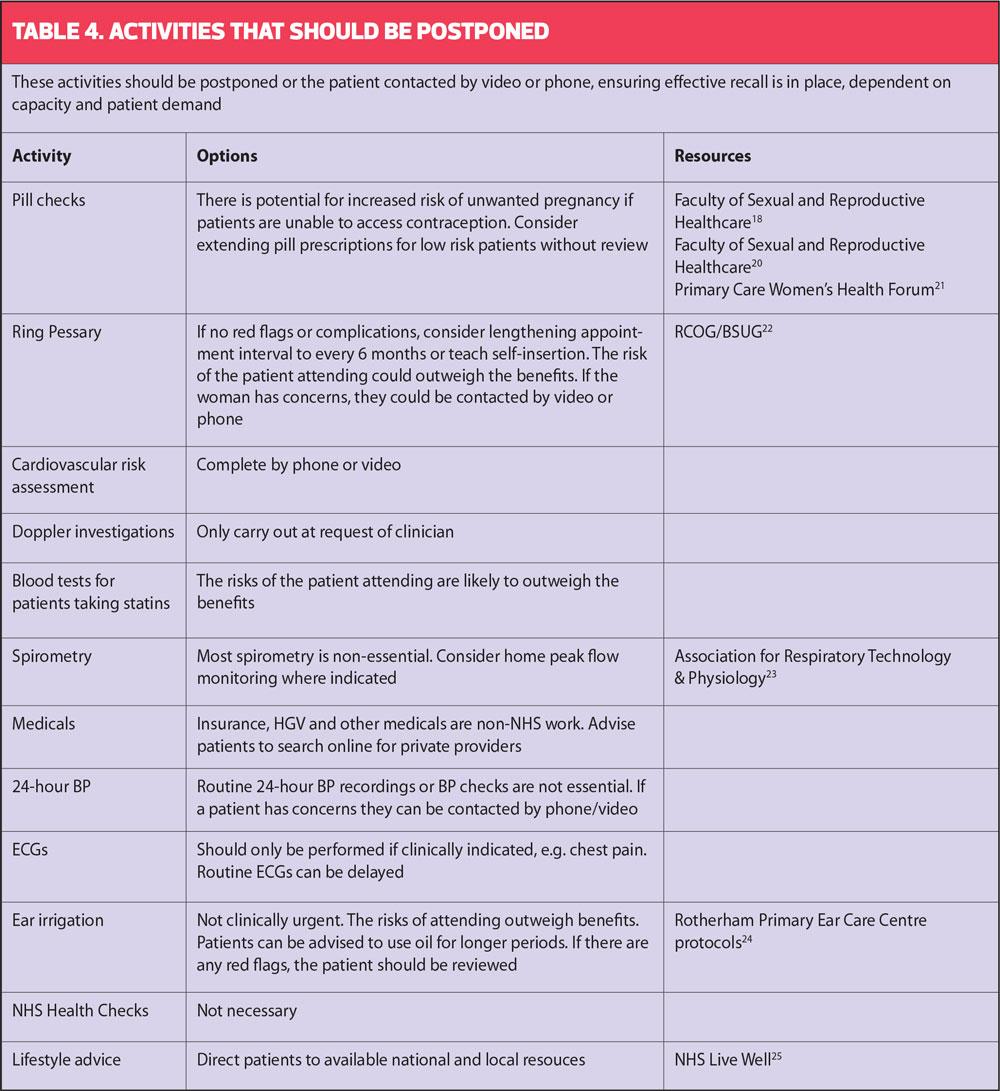
In March the RCGP and BMA produced Guidance on workload prioritisation during COVID-19 using a red, amber, green (RAG) rating system (Table 1).1
Many nurses and practices have already developed their own system for prioritisation of patients, but we thought it would be helpful to expand and develop the RCGP/BMA advice and came up with this advice.
This is supportive guidance for COVID-19 to assist nurse colleagues in general practice, and although policies may vary in different areas, practices can adapt it to meet their own requirements and regional guidelines.
It is important where possible to reduce face-to-face contact. NHS Digital provides resources on how to carry out remote consultations: you can register with FutureNHS Collaboration Platform.
Each activity should be risk-assessed and a suitable effective and appropriate alternative way of providing care should be considered. The emphasis should be on patient safety and ensuring the staff member still works within their scope of practice.
It is essential to remember that general practice plays a vital role in identifying and treating acute illness and worsening of chronic disease during the pandemic, to prevent increased morbidity and mortality from non-COVID-19 causes.
WHAT ELSE CAN YOU DO?
Look after your own wellbeing
COVID-19 will have an impact on general practice staff in many ways – possibly through direct experience of the illness, bereavement or through the increased or just different pressures of working during and after a pandemic. Practices should consider identifying someone within the team who can signpost colleagues to organisations that can provide support. Speak to a colleague if support and advice about your mental health would be valuable. It’s good to talk.
QOF work
Although the Quality and Outcomes Framework has been temporarily suspended as part of the NHS’ efforts to remove barriers to the national COVID-19 response, if you do find that your workload is reduced, now would be an opportunity to contact patients by phone/video to review QOF progress and document the outcomes in the patient’s records.
Long term conditions
Consider undertaking virtual group consultations, taking advantage of the opportunity to access free training via https://www.events.england.nhs.uk.
Undertake medication reviews
If you are a non-medical prescriber you could undertake medication reviews using phone/video consultations. There may be additional prescribing-related work you could undertake, for example, identifying potential cost savings for your practice. Take advice from your CCG pharmacist.
Staffing issues
The COVID-19 situation has required some people to move into areas of practice that not within their specific job descriptions. This should be a temporary measure but it is an opportunity to review your current role, and look for opportunities to work more closely with colleagues across the primary care network, for example, in district nursing.
Consider having student nurses in your practice. A positive experience is likely to encourage them to consider working as a GPN. Speak to your local training hub.
Clinical supervision
Clinical supervision is essential to demonstrate the commitment of the organisation to its clinical staff. It encourages reflection on clinical practice, using a constructive approach, to support and enable clinical staff (including GPNs), with the aim of improving the quality of care provided to patients. Speak to your CCG, PCN or LMC lead about setting this up in your practice.
- This article has been adapted from a resource by the same authors, developed for general practice nurses in the Wessex LMCs, available at https://www.wessexlmcs.com/informationsupportfornursesduringcovid19
REFERENCES
1. RCGP Guidance on workload prioritisation during COVID-19. https://www.rcgp.org.uk/-/media/Files/Policy/A-Z-policy/2020/covid19/RCGP-guidance/202003233RCGPGuidanceprioritisationroutineworkduringCovidFINAL.ashx?la=en
2. Government guidance on shielding. https://www.gov.uk/government/publications/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19 GOV
3. Royal College of Psychiatrists. COVID-19: Working with vulnerable people. https://www.rcpsych.ac.uk/about-us/responding-to-covid-19/responding-to-covid-19-guidance-for-clinicians/community-and-inpatient-services/covid-19-working-with-vulnerable-patients
4. NHS Digital. Coronavirus (COVID-19) Shielded patients list. https://digital.nhs.uk/coronavirus/shielded-patient-list
5. NHS England and NHS Improvement London. Diabetes COVID-19 Key information. https://www.england.nhs.uk/london/london-clinical-networks/our-networks/diabetes/diabetes-covid-19-key-information/
6. Primary Care Respiratory Society. Crisis management for asthma and COPD during the UK COVID-19 epidemic; 19 March 2020. https://www.pcrs-uk.org/news/crisis-management-asthma-and-copd-during-uk-covid-19-epidemic
7. Global Initiative for Chronic Obstructive Lung Disease (GOLD). COVID-19 guidance. https://goldcopd.org
8. Asthma UK. Coronavirus (COVID-19). Health advice for people with asthma. https://www.asthma.org.uk/advice/triggers/coronavirus-covid-19/
9. British Lung Foundation. Coronavirus and COVID-19. https://www.blf.org.uk/support-for-you/coronavirus
10. Diabetes UK. Coronavirus and diabetes. https://www.diabetes.org.uk/about_us/news/coronavirus
11. Association of British Clinical Diabetologists. COVID-19 (Coronavirus) Information for Healthcare Professionals. https://abcd.care/coronavirus
12. Royal Pharmaceutical Society. Clinical resources during COVID-19. https://www.rpharms.com/resources/pharmacy-guides/coronavirus-covid-19/coronavirus-cpd-resources#warfarindoac
13. QE Gateshead. Subcutaneous self injection for anticoagulation treatment. https://www.qegateshead.nhs.uk/sites/default/files/users/user53/gynaeoncology/IL426%20Subcutaneous%20Self%20injection%20for%20anti-coagulation%20treatment.pdf
14. Newcastle upon Tyne Hospitals NHS Foundation Trust. Patient self administration of medicine policy; July 2011. http://www.newcastle-hospitals.org.uk/PatientSelfAdministrationofDrugs201107.pdf
15. Gloucestershire CCG. Vitamin B12 Deficiency. Glos Care Pathway. https://g-care.glos.nhs.uk/pathway/867/resource/11
16. British Heart Foundation. Anticoagulants and NOACs. https://www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/drug-cabinet/novel-anticoagulants
17. British Society for Rheumatology. COVID-19: guidance for rheumatologists. https://www.rheumatology.org.uk/news-policy/details/covid19-coronavirus-update-members
18. World Health Organization. Guidance on routine immunization services during COVID-19 pandemic in the WHO European Region (2020). http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/novel-coronavirus-2019-ncov-technical-guidance/coronavirus-disease-covid-19-outbreak-technical-guidance-europe/guidance-on-routine-immunization-services-during-covid-19-pandemic-in-the-who-european-region-2020
19. Royal College of Nursing. COVID-19 (coronavirus). https://www.rcn.org.uk/covid-19
20. Public Health England. Routine childhood immunisation schedule. https://www.gov.uk/government/publications/routine-childhood-immunisation-schedule
21. Primary Care Women’s Health Forum. How to manage contraceptive provision without face-to-face consultations; March 2020. https://pcwhf.co.uk/resources/how-to-manage-contraceptive-provision-without-face-to-face-consultations/
22. Academic Health Science Networks. NWCSP Help and Advice (Wound care). https://www.ahsnnetwork.com/nwcsp-help-and-advice
23. Primary Care Women’s Health Forum. NHSEI and PHE smear taking during COVID-19. https://pcwhf.co.uk/resources/nhsei-and-phe-smear-taking-during-covid-19/
24. Faculty of Sexual and Reproductive Healthcare. Clinical Effective Unit clinical advice to support provision of effective contraception during the COVID-19 outbreak. https://www.fsrh.org/documents/fsrh-ceu-clinical-advice-to-support-provision-of-effective/
25. NICE. (Search for blood monitoring). https://www.nice.org.uk/search?q=blood%20monitoring
26. Faculty of Sexual and Reproductive Healthcare. Updated guidance on combined hormonal contraception. https://www.fsrh.org/standards-and-guidance/documents/combined-hormonal-contraception/
27. Royal College of Obstetricians & Gynaecologists/British Society of Urogynaecology. BSUG guidance on management of urogynaecological conditions and vaginal pessary use during the COVID-19 pandemic. https://www.rcog.org.uk/globalassets/
documents/guidelines/2020-04-09-bsug-guidance-on-management-of-urogynaecological-conditions-and-vaginal-pessary-use-during-the-covid-19-pandemic.pdf
28. Association for Respiratory Technology & Physiology. ARTP COVID-19 Update; 18 March 2020. https://www.artp.org.uk/News/artp-covid19-update-18th-march-2020
29. Rotherham Primary Ear Care Centre and Audiology Services. Protocols. http://www.earcarecentre.com/professionals/protocols/
30. NHS Live Well. https://www.nhs.uk/live-well/
Related articles
View all Articles